A Team Effort: Strong Provider-Detailer Relationships to Amplify Evidence-Based Care (Part II)11/3/2020
Overview: The DETAILS blog presents a special two-part series of what it takes to build a strong provider-detailer relationship from the perspective of a long-time academic detailer and then, from one of her local physician partners that’s received AD for almost 15 years. You can read Part One here. In Part Two, we get a chance to speak with Dr. Robert ‘Bob’ Schwartz, a Vermont family physician and medical director who discusses the impact of AD on his clinical practice. Bob reflects on what a strong provider-detailer relationship looks like from the perspective of a clinician, especially in the midst of COVID-19, and offers his advice to other providers considering AD. An interview with Winnie Ho, NaRCAD Program Coordinator. Tags: Detailing Visit, Evidence-Based Medicine  Winnie: We’re so excited to have the chance to speak with a clinician who’s been receiving AD for a long time! Can you tell us a little bit about how you came to work with the Vermont Academic Detailing Program? Bob: It’s been several years that I’ve been blessed with Amanda Kennedy’s presence on the AD service. I would say that it actually all started back when we first decided we were not going to allow pharmaceutical representatives in the office about 20 years ago. We decided that it wasn’t a good use of our time. Then Amanda and the Vermont Academic Detailing Service came onto the scene. They presented a formal alternative to learn about medications from a non-biased view – and so we’ve participated in every single session since then. W: That’s incredible!  B: The program is great – I think what’s really critical is that the program has such a high level of professionalism that you can be completely trusting of the information that you’re getting. My colleagues and I are always so thrilled when there’s another topic ready. I know how long it takes to get these things set up. You know it’s not just something someone slaps together on a random afternoon. Amanda is an absolutely amazing professional, and the fact that she’s been with us for so long helps develop a personal relationship and it builds trust. W: This relationship has been developed over more than a decade! Here at DETAILS, we don’t always get a chance to ask about what happens after the detailer leaves the office. What challenges in clinical care make it critical to lean on Amanda as a trusted source of evidence and resources? B: I like that AD is not about a specific medication, but rather a specific medical condition. As a clinician, I think about the patient sitting in front of me with COPD, not about who I can get on a specific drug. Pharmaceutical detailers only talked about specific medications and you couldn’t trust the information as unbiased. They never gave you the whole picture. What’s really important in medicine is how all the pieces fit together, and that’s really hard as a clinician to figure out on your own. With AD, I can reach out to say that I have COPD patients and I really want to get more knowledge about COPD. 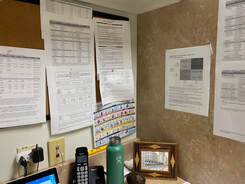 Dr. Schwartz's desk with AD Materials accumulated through the years from the Vermont Academic Detailing Program Dr. Schwartz's desk with AD Materials accumulated through the years from the Vermont Academic Detailing Program W: Right, and there’s an abundance of research that’s difficult to sort through on your own. B: AD is one of the few places that you can get this comprehensive evaluation of a specific condition and the medications that surround that. The other thing is that they bring materials. It might be a one-page sheet with diabetes medications based on class, relative cost, brand and generic names, and dosage. Or, it might be a COPD assessment score tool that I can easily refer to. These clinical aids are a big part of what detailers bring for us. W: Absolutely – those materials take a long time to create! I wanted to dive a little deeper into the provider-detailer relationship. What role do you think trust plays in sustaining a provider-detailing relationship for the long-term?  B: When we ask Amanda a question that she doesn’t know the answer to, she will tell us that she doesn’t know, but will look into it. A week later, you get an e-mail with information that she’s put together. We trust her and know that the dynamic of the relationship is not manipulative. We know that the information is carefully researched and that she’s not going to fill in the blanks by winging it. All of our detailing sessions have an unstructured portion where we can ask specific questions of Amanda. It allows the providers in our practice to have an organic conversation about a specific issue, and it can be hard to replicate this without the support of a detailing program. W: It’s always important to acknowledge what we know and what we don’t know, especially right now with COVID-19. It’s disrupted a lot of things, and I imagine for our healthcare providers, more than ever, there’s a lot of extra challenges. Our detailers’ main goals have always been to support their local providers and to be there with them through obstacles as they arise. What would you want detailers to understand about the challenges that COVID has brought on for clinicians?  B: Everything has been changing over the last several months and navigating COVID challenges takes up a lot of time. However, we still have to take care of our diabetes and our COPD patients and so more than ever, it’s critical that we have access to information that is streamlined, accurate, and that we can be confident in. I always tell people that medicine and life are team sports, and if you think you’re going to excel at either one of those alone, you’re going to be disappointed every time. We need Amanda on our team because she fills this vital role, that’s even more vital to have filled today. W: And finally, we know that there’s a lot of other clinicians who may be on the fence about receiving AD because they’re unfamiliar with it, or may have lingering distrust from pharmaceutical representatives. As someone who’s received AD for a long time, what advice would you give to other providers who may be considering these visits?  B: I conceptualize AD like this – it’s like getting on the super highway instead of taking the secondary roads. I could drive to Chicago and never leave a two-lane highway, or I can get on the 90 and drive on that to Chicago all the way. To other clinicians – we have certain responsibilities to ourselves and our patients, and one of those responsibilities is to keep up with what’s going on and to know how to use it to better care for our patients. What I would tell other clinicians is that, you have this responsibility anyway – why not have another team member who’s an expert on this and give this information to you in an hour what would have taken you six hours to do yourself? We’ve loved our partnership with Amanda, and we look forward to what comes next out of it. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Bob Schwartz, MD, is a family physician at Northshire Medical Center in Manchester, Vermont. He’s served as the Associate Medical Director for Dartmouth Hitchcock Putnam, a multi-specialty group in the southwestern part of Vermont. Dr. Schwartz completed his family medicine training at Lancaster General Hospital in Lancaster, PA following his medical education in the Honors program at Northwestern University. He currently lives in East Dorset, Vermont. Trust, Mutual Respect, and Transparency: Building a Strong Provider-Detailer Relationship (Part I)10/20/2020
Overview: The DETAILS blog presents a special two-part series of what it takes to build a strong provider-detailer relationship from the perspective of a long-time academic detailer and from one of her local physician partners that she's detailed for almost 15 years. In Part One, we speak with Amanda Kennedy, PharmD, BCPS, who serves as the Director of the Vermont Academic Detailing Program and has been an active detailer since 2002. The Vermont Academic Detailing Program sees about 450-500 providers a year on 1-2 clinical topics. In Part Two, we hear from Dr. Robert “Bob” Schwartz, a Vermont family physician who reflects on his experiences with academic detailing visits with Amanda. Stay tuned for Part Two! An interview with Winnie Ho, NaRCAD Program Coordinator. Tags: COVID-19, Detailing Visits, E-Detailing  Winnie: Amanda, thank you for taking the time to reflect on the relationships you’ve built through the years with local providers. What would you say are the key elements for building a strong provider-detailer relationship, and why? Amanda: Trust and mutual respect. If the clinician doesn’t trust you, then it’s going to be very hard to make recommendations for practice change. Mutual respect goes both ways. As much as I am providing a service, I also expect the clinician to show up and be engaged in our visit, because only then can we have the kind of conversation that gets at the heart of the behavior change we hope to see. W: Engagement is such a key component of these visits, especially for creating a safe space for providers to be open and honest with the detailers about their concerns and needs. I want to take you back to the start and ask you to reflect on what it was like to be brand new to AD. What advice would you give to a new detailer in those shoes?  A: Confidence is key. You can study and practice everything with your team, but at some point you have to get out there and just do it. Building that relationship requires confidence and the belief that you have something valuable to offer. When you only have a few opportunities a year to meet with clinicians, you have to capitalize on those moments. It can be difficult to establish that rapport and trust when contact is infrequent. It’s about persistence, patience, and continuing to show the clinician that you want to be helpful. Some things can get in the way, such as not having the same clinical background as the provider you’re working with, and not always feeling qualified. But remember, you wouldn’t have been hired in this role you weren’t qualified! W: That’s certainly important to keep in mind. You were also recently introduced to a new playing field – virtual visits. Compared to traditional in-person visits, what’s it like starting new relationships through e-Detailing?  A: Virtual visits can be efficient, because we eliminate the cost of travel, we can reach more people and more often. Most of the content of that first call is the same as in person. On a first visit, most of what you’re doing is the introduction of your work and your program. I’m transparent about everything with them. I don’t bring up my materials or share my screen until that clinician has had the opportunity to ask me any questions they have. I give them a chance to see me as a person first, without distractions. This takes a few minutes longer virtually than in person, and it can be harder to gauge body language, but it’s an important first step in establishing a relationship. W: That’s a good piece of advice for many programs making that transition into e-Detailing, as I know it was a big concern about starting these relationships over a new medium. Do you have an example of how maintaining these relationships can support better health outcomes for patients?  A: Yes. While our team was putting together information on a COPD campaign, I was meeting with Dr. Schwartz on a different topic. At the end of our visit, I told him about the next topic and asked him what was concerning him about it. He asked for more information on benzodiazepines and patients with COPD. While this specific information wasn’t included in the overall COPD campaign, I’ve personally been looking for good articles that would be helpful for his particular interest. In attending to this specific request, I’m showing him that I’m listening to and addressing his need. W: That’s some strong needs assessment! And I’m sure that information will be put to good use. You’ve been in this field for 18 years - have you seen how your support has resulted in clinical behavior changes over the years? A: The most rewarding thing for me is going into a clinic and seeing a tattered version of a handout we used five years go, or a clipped out table taped up on a board. That’s how you know your information has stuck around and has had a long-term impact.  Also, on visits, if a provider is struggling to think of how to incorporate a behavior change into their practice, I have stories from other providers and can provide suggestions and ideas that have worked for them. I can leverage a community of long-term relationships. W: Have you found that these strong relationships allow you to get more out of a detailing visit, especially when there are some difficult conversations? A: Yes, absolutely. It’s important to know, especially right now, that we’re suffering a community-wide trauma because of COVID-19. Out patients need their providers, but those providers have their own challenges going on too. There are family issues, financial issues, and community issues. Our jobs as detailers is to be a support as much as we can, and to help providers make beneficial changes for patients that are rooted in evidence.  We’re currently doing a topic on managing stress related to COVID, but before we get into how providers can help their patients, we pause and ask them how they’re doing. I’ve had providers share deeply personal information with me that can be important in understanding how to best support them in addition to them supporting their patients. They know that they can trust us. W: As we wrap up, what would your final advice be to other detailers looking to replicate your success? A: My advice? It doesn’t take 18 years to build a relationship with someone. It just takes enough of your effort to show that you’re really trying and taking opportunities to be of service. It means showing that you’re trustworthy, and that you’re going to respect and support them just like you’re promising them that you will. (Part One of Two). Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Amanda Kennedy, PharmD, BCPS, is the Director of the Vermont Academic Detailing Program at the University of Vermont’s Office of Primary Care. She has also been an active academic detailer for nearly 20 years. Amanda regularly serves as a faculty facilitator for NaRCAD’s Academic Detailing Techniques trainings. In addition to her role with academic detailing, Dr. Kennedy is a Professor of Medicine at the University of Vermont’s Larner College of Medicine. She currently serves in the Department of Medicine Quality Program, teaching and mentoring physician residents, fellows and faculty in quality improvement and health services research. An interview with Vishal Kinkhabwala, MD, MPH, HIV Prevention Activities Coordinator, HIV Prevention Unit, Michigan Department of Health and Human Services. The overarching goal of the HIV Prevention Unit is to expand access to PrEP for patients throughout the state of Michigan. by Anna Morgan, MPH, RN, PMP, NaRCAD Program Manager Tags: Conference, Detailing Visits, E-Detailing, HIV/AIDS, PrEP  Anna: We’re so happy to be catching up with you today, Vishal! Can you tell us a little bit about yourself and how you got into the work of academic detailing? Vishal: My background is in both public health and medicine. After finishing medical school, I realized that as much as I loved the clinical aspect, I wanted something that combined both my passions of public health and clinical medicine. My first job after graduating was in New York where I linked newly-diagnosed HIV patients into care. About a year later, I found an opportunity at the Michigan Department of Health and Human Services that fit with what I ultimately wanted to do, HIV prevention. My current work is focused on ending the HIV epidemic in Wayne County. One of my favorite parts of my job is detailing, which I do part-time. Our program officially began detailing in September of 2019. We’re in the process of making the jump to e-Detailing, but we’re still in the planning stages. Anna: Before we chat about how you and your team have been preparing for e-Detailing, let’s talk about how clinicians in Michigan have received your messages around PrEP. Were clinicians receptive to your detailing efforts when you were conducting in-person visits? Vishal: Most clinicians that we detailed were either already familiar with PrEP or had that enthusiasm to learn about it. Many of the clinicians were excited about helping with MDHHS’s overall goal of increasing patient access to PrEP and talking about the associated HIV prevention counseling. Clinicians were typically familiar with PrEP but weren’t aware of the nitty-gritty details of how to prescribe and manage it. A big part of what we discussed during our detailing visits was identifying which patients are candidates for PrEP. Our program’s purpose is to increase access, even if it’s just for one or two patients.  Anna: It’s wonderful that the clinicians you’ve detailed have been supportive of your program’s goals. Transitioning to e-Detailing will certainly be easier knowing that you have support from clinicians. What have you learned so far from planning for e-Detailing? Vishal: It’s been fun prepping for e-Detailing with our team. The big thing I’ve learned through networking with detailers from other jurisdictions is to be flexible and be prepared for any situation, especially in the virtual environment. You might have one idea of how your session will go, and it could go in the opposite direction, which is part of the charm of detailing. It’s about forming a connection and tailoring your methods to what the clinicians' and practices' needs are. I’m a relationship-oriented person, and I feel like that’s one of the most rewarding parts of doing this. One of the things that also excites me about virtual education is the access to information right at your fingertips. For example, I was detailing a clinician about PrEP and HIV prevention last year who asked me, "Well, I have this issue with a lot of patients with STDs. Can you talk to me about STD treatments?" It was an in-person visit, so I only had the materials that I had brought with me, which were all focused on HIV. The beauty of doing e-Detailing is that you can have resources pulled up and can get the information for the clinician almost instantaneously. As I said earlier, detailing is all about having that relationship, meeting the clinician where they're at, and serving their needs. Virtual education gives you another tool to be able to do just that. 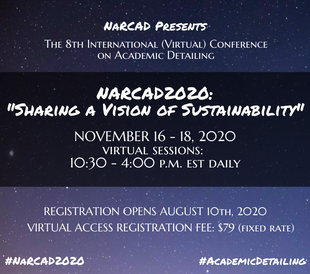 Anna: What a positive spin on e-Detailing! Speaking of sustainability, that’s the theme for our upcoming conference. You attended our conference last year in Boston and will be presenting at our virtual conference this year. What were some key takeaways from last year’s conference that you were able to bring back to your program and implement? Vishal: Last year’s conference was my first exposure to NaRCAD and the world of detailing- it was honestly one of the coolest experiences I’ve ever had. It was great to be exposed to e-Detailing through the virtual detailing panel before it was even brought to the forefront during COVID. Because I was hired a few months prior to the conference, I had not attended a training yet. I joined the “AD 101” breakout group, which was supremely helpful. When I got home, I did mock detailing sessions with my colleague and reviewed all the resources on the NaRCAD website. I also practiced detailing on the stress balls I have in my office! Anna: It’s so nice to hear how impactful the conference was for you as a new detailer. We strive to include a diverse audience of new and veteran detailers each year. What are you looking forward to most about this year’s conference? Vishal: There are so many absolute rock stars in the field of detailing. I’m looking forward to getting to see familiar faces and meet new faces over the virtual platform. I’m excited for the exchange of ideas, programs, and concepts. So many people have given me ideas for our program in Michigan. It’s such a good feeling when I can say that not only have I received help from others, but that I’m able to inspire other people. It’s also comforting to know that this is such a passionate group of people that no matter the adverse situation, the work continues getting done. I’m counting down the days until the conference in November! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Vishal has been working with the Michigan Department of Health and Human Services since August 2019 as the HIV Prevention Activities Coordinator. His work focus is on program planning and implementation for the Ending the HIV Epidemic Initiative, focused on southeastern Michigan. As part of this initiative, he works as a part-time Academic Detailer with a focus on HIV Prevention with the overarching goal of increasing access to PrEP throughout the state of Michigan. He completed his Master of Public Health degree from Benedictine University in Lisle, IL in August 2013 and his Doctor of Medicine degree from Avalon University School of Medicine in Willemstad, Curacao in June 2018. Prior to working for the State of Michigan, Vishal worked for the New York State Department of Health as a Disease Intervention Specialist, working on a pilot HIV Molecular Clusters initiative. Vishal is particularly looking forward to moving the Michigan Department of Health and Human Services PrEP Detailing program forward into the realm of virtual “eDetailing.”  Jerry Avorn, MD, Co-Director, NaRCAD Tags: COVID-19, Detailing Visits, E-Detailing, Jerry Avorn The pandemic has changed everything about our lives and our work. Some occupations have been able to adapt to the new abnormal, such as programmers and financial traders. Others have found it harder to do their jobs as before, like brain surgeons and academic detailers. For the latter, in a socially-distant, avoid-human-contact world, how can we pursue an activity that has as its very definition in-person, interactive communication? Academic detailing programs around the country and the world have been grappling with this challenge. And unlike our colleagues the brain surgeons, we have been able to come up with some plausible solutions, even if nothing is quite the same as being up close and personal. We’ve been learning about the virtues and limits of Zoom/Skype/WebEx. If we’re paying attention, using them can bring into sharp focus the central aspect of interactivity, on steroids. It’s a little like becoming a better runner by strapping weights on your ankles (or so my athletic friends tell me). A non-adept academic detailer can mis-use a Zoom encounter even worse than a face-to-face one: “Sit still for 20 minutes while I do this presentation at you.” That will fail on a platform even more calamitously than it does in person. (One clue is when the prescriber mutes their video to read their e-mail.) But if we’re open to it, the e-encounter can focus our attention even more on whether we’re learning where the clinician is coming from, getting feedback, actively asking what sub-topics they most want us to cover. The artificiality and forced intimacy of a screen-to-screen encounter, and the reason we currently have to do our work like this, can also focus us even more on another key aspect of academic detailing, empathy. “How are you holding up?” or “I bet COVID has really changed your practice” are opening statements that can address the 800-pound virus in the (virtual) room, acknowledging the obvious strangeness and discomfort that afflict so many conversations in these awful times. On a more concrete level, pandemic-style education is also forcing us to come up with new ways to use our educational materials. What to do when you can’t focus a practitioner’s attention on a particular graph or table you’re showing them because they’re dozens of miles away? Displaying a PDF of a document and whizzing around your cursor is one easy, but primitive solution. What about presenting a list of topics hot-linked to a detailed display for each? Or completely re-formatting our materials (stop moaning) for better adaptability to a computer screen?  Those of us who also used to teach in classrooms have learned that with a little work (ok, a lot of work) coronaeducation can even be better than what we’ve been used to doing: using links to video clips or animations, real-time interactive polling, techniques that maybe we could have been using in the classroom, but weren’t. Another key advantage of academic e-Detailing, if we can figure out how to make it work well, is the prospect of having a virtual visit with a clinician without the sunk time of getting to their office – a major enhancement in working with practitioners who may be an hour’s drive or more from the educator’s base. The benefit for our field in productivity and cost-effectiveness could be considerable. Contrary to naïve beliefs that “Soon everyone will be protected by the vaccine and we can get back to normal,” this virus probably won’t let us return fully to the old ways any time soon. Instead, it will force us to mutate our work to cope with it. And in the process, not only will we be able to continue our work, we may even discover better ways of doing it. Be strong and stay safe. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation! Biography.
Jerry Avorn, MD, Co-Director, NaRCAD Dr. Avorn is Professor of Medicine at Harvard Medical School and Chief Emeritus of the Division of Pharmacoepidemiology and Pharmacoeconomics (DoPE) at Brigham & Women's Hospital. A general internist, geriatrician, and drug epidemiologist, he pioneered the concept of academic detailing and is recognized internationally as a leading expert on this topic and on optimal medication use, particularly in the elderly. Read More. Evidence into Value and Action: Reflections on 30 Years of AD in South Australia (Part Two)10/5/2020
An interview with Debra Rowett, BPharm, Adv Prac Pharm, FPS, the Director of the Drug and Therapeutics Information Service (DATIS) in Adelaide, Australia. Debra joins Winnie Ho, NaRCAD Program Coordinator in a two-part conversation about a 30-year career of pioneering academic detailing in Australia and reflects on the past, the present, and the future of the field. In Part Two, we discuss the evolution of academic detailing as the world of healthcare changes. You can read Part One here. Tags: Detailing Visits, Evidence-Based Medicine, International, Medications, Program Management  Winnie: You wear so many hats when it comes to AD. How have those roles changed over your time with DATIS? Debra: Before I was Director of DATIS, my role was primarily around developing our detailing materials, and evaluating the evidence and our program. I was always interested in the synthesis of evidence and turning that into value for clinicians. I was a clinical pharmacist who was working with people across many disciplines, and there was a growing body of evidence, but translating that into practice was always a challenge.  W: I think you touch on a fundamental aspect of AD – that we turn evidence into value, and that we translate all this research into action. It’s very critical that AD continues to provide that independent, trusted, unbiased source of information to ensure evidence is disseminated responsibly and utilized properly. D: I would agree with that, very much. We live in an information-dense era and much of the information is synthesized and aggregated at the population-level, but clinicians are responsible for decisions at the individual patient level. I think AD is about bringing evidence to the point at which clinical decision making is made. W: I’m curious about your experience with evaluating evidence for AD materials. It’s clearly a difficult, but super important aspect of AD. You have all these clinicians who are trying their best to make the best possible decision for their patient – and AD comes in, and in many ways, helps share in that responsibility.  D: Evaluating evidence is also about recognizing what we don’t know in the evidence. When reviewing the evidence for an AD program, we look for where there are gaps in the evidence, where there’s controversies, and differences in opinion about the evidence. No matter how well done, you make choices along that entire process about what to include, what to exclude – and even with the synthesized evidence, there is still human judgement about how to use it. W: Right, and that human judgement also needs to focus on how that evidence came to be and how it was produced. D: Absolutely. As we know evidence-based medicine is not just about the randomized controlled trials and published evidence, it’s about the intersection of published evidence, clinical judgement, and the patient’s specific needs, goals, and circumstances. The real opportunity for AD is that you can personalize this information for the provider to work with.  W: It’s extraordinarily rewarding work, and it’s a constant process in grappling with the things we don’t know. As someone who has been in this work for a long time and has had to adapt a long-standing AD program to changing guidelines and medical evidence, you’ve likely seen some big shifts in the medical consensus. Take opioids for example – the consensus around the safety of its use has had a dramatic change over the years. How have you adapted when the evidence base can sometimes change quickly within a few years? D: It’s important that we come to providers with a balanced view, and that we acknowledge with them that there is uncertainty, that there is complexity, and that it isn’t easy to make these decisions with their patients. There’s a lot of things that we don’t know. If you come with too much certainty, you lose credibility because translating evidence into routine clinical practice is complex. Every time a medicine is prescribed for and used by a patient, we’re forecasting how the future will proceed - the exact benefits and harms that a patient will experience are uncertain.  People are living longer and with multimorbidity which presents new medical challenges. We’re seeing more people living with issues like musculoskeletal problems, hypertension, diabetes, renal problems, atrial fibrillation, and surviving their myocardial infarctions. The number of medications that patients take now compared to 30 years ago have increased. There are individual guidelines for each condition, that don’t necessarily take the other comorbidities into account. The drugs used to treat one issue may lead to treatment conflicts for another condition and needs to be taken into consideration. It’s not just in one area of practice that has changed too, or just our demographics – we’re seeing fewer solo General Practitioners and more team-based practice in Australia. AD needs to take all of that into account when considering how to detail, and also who to detail.  W: Can you explain what you mean by “who to detail”? D: It’s important to understand who the decision-maker is and what the decision you’re trying to address is – for some of our AD programs it might involve other health professionals; it’s not always the doctor. W: Right, and this whole of office approach looks at all the players involved in the continuum of care, and acknowledges that they may play a role in how clinical decisions are ultimately made.  D: Yes, and I think this is why AD is even more important now than it was when we first started. It allows us to bridge individual condition silos, and helps providers navigate multimorbidity. Healthcare is never a one-size fits all, even for an individual. Their circumstances and treatment goals can change over the course of their lives. AD can personalize the information and tailor it to the needs of the clinician. AD can also be the conduit between population level evidence and its translation into clinical decision making - that is one of its greatest strengths. W: NaRCAD has been lucky to see overarching growth of AD programs everywhere, along with all of its exciting new innovations and evolutions. Any final thoughts on AD before we hear from you at our upcoming conference? D: One of the things I try and impart when teaching the method of AD is to value the knowledge of the person you are detailing. There is a lot of listening that occurs in successful AD if you are truly to meet the needs of the provider you are visiting. If you keep at the very heart of what you do, respect for learning together and hold true to the principles of academic detailing, you will meet incredible people everywhere you go. It makes for a wonderful career. (Part Two of Two) Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Debra Rowett, BPharm, Adv Prac Pharm, FPS, has led an academic detailing team for over 20 years and is a member of the team which designed, developed and delivered the “Best Practice in Educational Visiting” training for academic detailers in Australia. Debra has worked closely with NPS Medicinewise since their inception and has provided consultancies to other national and international academic detailing programmes. Debra is an experienced academic detailer with expertise in designing, developing, training, implementing and evaluating academic detailing programmes. Debra has served as the President of the Australian Pharmacy Council and is currently the Vice President of the Council of Pharmacy Schools. Debra has worked extensively in the area of quality use of medicines, inter-professional practice, policy and health workforce development in Australia. Debra is a member of the national Drug Utilisation Sub-Committee of the Australian Pharmaceutical Benefits Advisory Committee (PBAC). An interview with Julie Anne Bell, MPH, Program Manager of Clinical Operations, Bureau of HIV, New York City Department of Health and Mental Hygiene. The mission of the Clinical Operations and Technical Assistance Program (COTA) is to provide innovative, culturally responsive, needs-based technical assistance and training to organizations and individuals working with people impacted by HIV. by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Detailing Visits, E-Detailing, HIV/AIDS, Materials Development  Anna: Thanks for joining us today, Julie Anne! Can you tell us about yourself and what brought you to your role as Program Manager of Clinical Operations at the New York City Department of Health and Mental Hygiene? Julie Anne: My first position out of graduate school was as a research assistant in the HIV program at the State University of New York. I’ve moved through a lot of sexual health work and have been with the Bureau of HIV at the New York City Department of Health and Mental Hygiene for three years. I love the programmatic work that I do in my current role. I deliver training, tailored technical assistance and public health detailing to clinical and non-clinical providers who care for people with HIV. Being a content expert and bringing the information directly to the clinics to support them is rewarding and, most of all, fun.  Anna: It sounds like your career path has led you to a wonderful position! What detailing topic is your program currently working on? Julie Anne: We’ve been focused on developing a public health e-Detailing campaign to support and strengthen providers’ initiation of immediate antiretroviral treatment, or “iART”. iART is for people newly diagnosed with HIV or returning to care after a long lapse. It recently became a standard of care in New York. Immediate initiation of ART is associated with several health benefits for people with HIV, including a significant decrease in the time to viral suppression, which ultimately, reduces the risk of disease progression, morbidity, and mortality for people with HIV as well as onward transmission and new HIV diagnoses. Prescribing ART immediately versus waiting for the patient to return after all lab work/genotype results come back can feel like a paradigm shift for providers, but HIV medications have advanced so much in terms of their high threshold to resistance and there is no longer a need to wait. Anna: Your team recently completed a campaign on strengthening the integrated care approach, which is a team-based approach where mental health care and medical care is offered to patients in the same setting. How did your previous campaign help shape your new iART campaign?  Julie Anne: During our previous campaign, we brought providers an array of materials and resources to help them meet New York City’s Ending the Epidemic benchmark. We included HIV-specific materials and resources, as well as additional tools to address substance use, housing, and mental health in order to strengthen their integrated care approach. Among those HIV-specific materials and resources was information about iART. During our detailing sessions, providers were consistently reporting the same barriers to implementing iART in their clinics. Barriers that were reported were lack of clinic workflow for iART, not knowing how to get the medications covered/paid for immediately, and feeling uncomfortable prescribing ART before receiving a lab based confirmatory HIV test and genotype testing result. We began to realize that the providers needed more support around this topic. Because our work is heavily data driven, we used the feedback we received from providers on the barriers they were experiencing around implementing iART to create our iART campaign and associated public health detailing action kit. The tools and resources in our detailing action kit highlight each component of iART, including HIV testing, payment options, genotype testing, and example clinic workflow. In the past, our program developed the public health detailing action kits and would hire consultants to do the detailing. For these campaigns, my colleague and I wanted to deliver the messages to the clinics ourselves and focus on relationship building. Anna: Having strong detailer-clinician relationships is an integral piece of a successful academic detailing program. How have you been able to build strong relationships with clinicians?  Julie Anne: We visited over 100 clinics that provide HIV services in New York City during our last detailing campaign, and we now have friendly relationships with these providers because of the trusting relationships we’ve built with them through our previous detailing work. Our team also attends regional group meetings for HIV providers to bring more awareness to our work and continue to build relationships and connections. We recently hosted a virtual launch event for our iART campaign and we had over 200 providers register. We provided an overview of COTA, our services, and e-Detailing. We wanted the providers to know exactly how we’ve pivoted during COVID-19, why this work is still important, and that we would reach out to them in the coming weeks for an e-Detailing visit. Being with the health department, we know where people are getting their care for HIV in New York City. We’d love to reach everyone who’s working with people who are impacted by HIV, including non-clinical providers. Since iART is an integrated care approach, both clinical and non-clinical providers are an integral part of the process. The first steps in the iART process begin with a positive HIV test which can happen in a non-clinical setting, such as a community-based organization. The next steps include looping in a medical provider with the addition of non-clinical support, such as benefit navigation, social work, and peer navigation. It can take multiple providers of different training and expertise to work together to achieve iART seamlessly.  Anna: Wow! You’re certainly connected to a lot of clinics and it doesn’t sound like you’ll have issues recruiting clinical or non-clinical providers for your upcoming e-Detailing visits. How has your team prepared for e-Detailing? Julie Anne: When the reality of the pandemic hit, the idea of transitioning our detailing program to a virtual platform was overwhelming. We did a deep dive into the existing literature to see how programs have done virtual detailing in the past. NaRCAD has also been an amazing resource to learn from and we continually check the website for new resources on e-Detailing. We then developed a Standard Operating Procedure (SOP) for our iART e-Detailing campaign. We worked as a team to create a step-by-step guidebook that includes our key messages, how to do a needs assessment, and how to address barriers that we expect might come up. We’re currently working on doing mock e-Detailing sessions with our colleagues and with providers who are iART champions in New York City. Our SOP will help guide us during these mock sessions and help prepare us for our field visits this fall. Anna: Creating a Standard Operating Procedure is a great idea and will be extremely beneficial to prepare for field visits. What are some challenges that you expect to face when you begin your e-Detailing work? Julie Anne: We’re expecting the usual technical problems like poor internet connection and access issues, but we’re working on strategies to overcome this. We also expect that providers will be experiencing burn out, so they may be hesitant to make some of the changes in their clinic to implement iART, such as establishing a new clinic workflow. However, the resources we’ve selected and created for our iART detailing action kit are a direct result of what providers reported that they needed during our last detailing campaign. We’re hopeful that the tools we’re providing will enable an easy transition for providers to adopt our key messages related to iART.  Anna: It’s remarkable that you’ve been able to create your e-Detailing campaign based on the specific needs of the providers in your community. How else is your team working towards sustainability? Julie Anne: iART is a sustainable practice because once providers understand the “why” and “how” to do it and the steps involved, there is no reason to go back to waiting to initiate a patient with HIV on ART. It’s important that people with HIV are given the opportunity to start ART immediately because it provides individual and public health benefits. iART is the new standard of care in New York, which encourages providers’ commitment to the practice, and the iART detailing kit will introduce tools and resources to increase the knowledge and confidence of providers to prescribe ART immediately. Additionally, COTA offers ongoing technical assistance at the request of the providers and full-day trainings on iART for new providers. We’re currently focused on our iART e-Detailing project, but it’s always an open-door relationship with providers. Right now, it’s iART, but providers can reach out to us about anything they’re struggling with and we’ll work with them to overcome the challenges they’re facing. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Julie Anne began working at the NYC Health Department in 2016 with the Bureau of Sexually Transmitted Infections in a research role. She transferred to the Bureau of HIV in 2017 where she focused on health policy work, and was promoted to her current role with the Clinical Operations team. She now manages the team that focuses on providing data-driven technical assistance to clinical and non-clinical HIV providers across New York City on HIV specific and supportive topics that address social determinants of health for people with HIV. Julie Anne is currently preparing to conduct e-detailing visits with NYC providers to support and strengthen practices for initiation of immediate antiretroviral treatment (iART) for people with HIV. An interview with Kelsey Bolton, Continuing Professional Development Consultant, Gundersen Health System by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Detailing Visits, COVID-19, CME, E-Detailing, Smoking Cessation, Substance Use  Anna: Hi, Kelsey! Thanks for taking the time to chat with us today. Can you tell us a bit about your academic detailing program in Wisconsin and your role? Kelsey: I’m a Continuing Professional Development Consultant in the Continuing Medical Education (CME) Department at Gundersen Health System. Gundersen Health System is a teaching hospital with a multitude of specialties that serves patients in Wisconsin, Minnesota, and Iowa. As part of my CME work, academic detailing stood out as an effective tool to disseminate our information and meet our clinicians’ educational needs. We started our detailing program last fall and have been focused on tobacco cessation. The detailing intervention is a spinoff of a performance improvement project we are working on for diabetes. I’m currently a one-woman show; I’m the program coordinator and the sole detailer. I detail physicians, NPs and PAs across the health system. Anna: Wow, it’s incredible that you’ve been able to build your detailing program from the ground up! Can you tell us what that’s been like? Kelsey: Academic detailing was a new concept to me prior to being introduced to it by my former manager, who sent me to the NaRCAD training in May 2019. Academic detailing is not a well-known concept in our hospital system. It was difficult to get past the gatekeepers and “enlighten” them about academic detailing. There are still misconceptions when I walk into a room for a meeting with a clinician – they often think that I’m a drug sales rep, that I’m an internal quality control person, or that I’m there for punitive reasons. I must quickly refute that and explain that I’m there to support and unburden them, not to make judgments about their work. Anna: Those misconceptions are quite common when starting a new academic detailing program. How are you able to “enlighten” the gatekeepers? Kelsey: It was bumpy at first and we tried a few different approaches, but I think we’ve finally been able to smooth it out. I have an advantage because I’m internal and I’m contacting clinicians from an internal email or phone number. I’ve also had our medical program coordinator, the doctor who is partnering with me to learn the clinical information, send out emails to gatekeepers prior to my detailing visits. Anna: Stakeholder buy-in is imperative when building a new detailing program.  Kelsey: Absolutely. Building relationships with key stakeholders has made all the difference. The medical program coordinator I work with, as well as other experts in the organization, helped me curate my detailing aid and key messages. I practiced my detailing sessions with these stakeholders before going out in the field. It was an easy way to build relationships and get them on board – it only took a 15-minute practice detailing session! I’m also fortunate enough to have support from senior leadership. They’ve been able to open doors by letting people throughout the organization know that they support the academic detailing work I’m doing. Anna: It sounds like both managing your academic detailing program and being in the field has helped you be successful in getting your program off the ground. What has it been like to grow and manage your AD program? Kelsey: It’s like herding cats! The detailing program is 25% of my workload, so completing all the administrative work plus the detailing visits is quite a commitment. By the end of this year, I will have detailed over 200 clinicians. “Marathon detailing” has put me in a groove. It has definitely been challenging, but I appreciate that I know the ins and outs of it now – both the administrative tasks and the field work. I feel prepared to help train others. I plan to start training one of my colleagues to become a detailer in the fall. Anna: When thinking about team expansion, it’s also important to think about the impact of COVID-19. How has COVID-19 impacted your program? Kelsey: We paused our detailing visits for about 3 months, and by the time we started talking about bringing them back, NaRCAD was putting out a lot of information about e-Detailing. Before COVID, I had barely done anything with video calling, but getting thrown into working from home, we jumped into a lot of video calls. I learned how to work virtually on the fly, which made it easier to adapt to e-Detailing. I did a few practice e-Detailing sessions with my colleagues and I’ve now successfully completed several visits virtually. The NaRCAD webinars were a lifesaver. We plan to continue e-Detailing until it’s safe to return to in-person visits. Anna: A lot of academic detailing programs had to adapt quickly to e-Detailing during the pandemic. What does the future look like for your program?  Kelsey: For the more near future, we are working on collecting data for the tobacco cessation campaign to eventually publish research on the efficacy of the academic detailing intervention. We’re going to pull patient data from the EMR, as well as look at the qualitative data from the evaluation surveys. This research will help inform our organization on the benefits of academic detailing as an educational intervention. We would also like to continue the program with other strategic initiatives like substance use disorder, social determinants of health, and cancer screening. I have a soft spot for topics similar to tobacco cessation that are sometimes discouraging to clinicians because they don’t feel like they can make a difference. I know that through detailing, I’m able to give them a fresh take on these topics, and reinvigorate them in providing the best care for their patients. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Kelsey Bolton is a Continuing Professional Development Consultant in the CME department at Gundersen Health System in La Crosse, WI and the program lead for its Academic Detailing program. She received her Bachelor of Arts degree in Communication Studies in 2015, Healthcare CPD Certificate in 2019, and is currently pursuing her Master’s in Organizational Leadership. She has completed over 100 detailing visits and is presently conducting a research project on the efficacy of tobacco cessation academic detailing. An interview with Mary Liz Doyle Tadduni, PhD, MBA, MSN, RN, Education Consultant, Independent Drug Information Service and Expert Training Consultant, National Resource Center for Academic Detailing by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Detailing Visits, E-Detailing, COVID-19  Anna: Hi, Mary Liz! We’re excited to learn more about what the pivot to e-Detailing has been like for you as an expert academic detailer for over 16 years and a NaRCAD training facilitator. Can you tell us briefly how your role as an academic detailer at Alosa Health has changed since the COVID-19 pandemic began? Mary Liz: The restrictions on in-person meetings has resulted in all of my detailing visits switching over to phone or video calls. The number of providers I’ve been detailing has also considerably decreased due to time constraints and office restrictions related to COVID-19. In terms of the topics I’ve been detailing on, our team has been maintaining focus on delivering our planned modules, but I do discuss the impact of COVID-19 quite a bit with providers. Our current topic for Pennsylvania’s Pharmaceutical Assistance Contract for the Elderly (PACE) is dementia, which is important as it relates to COVID-19. Patients with dementia who reside in nursing care facilities in Pennsylvania can’t see their loved ones due to restrictive visiting policies. Primary care providers are dealing with the challenges and consequences of this every day – and academic detailers can’t ignore it. Anna: It’s crucial that detailers understand the ways COVID-19 impacts the work of frontline care providers. Mary Liz: Absolutely. With COVID, healthcare delivery has changed dramatically and there’s been a large increase in telehealth visits. Many providers in Pennsylvania are working from home and not going into the office or seeing only a limited number of patients in the office setting. Even if they are seeing patients in person, the process of seeing a patient has changed. The offices sometimes have front desk staff working from home and require patients to wait in their cars before entering the building. Primary care providers are still trying to adjust to all of this. You need to consider what is really happening on the ground for providers during your detailing visits – it’s part of your needs assessment. The needs of the primary care provider right now differ greatly from the pre-COVID era.  Anna: Assessing a clinician’s individual needs is an integral piece of a traditional academic detailing visit. How have you been able to implement AD in its intended form when detailing virtually? Mary Liz: The original model of academic detailing with Dr. Jerry Avorn has always been 1:1, face-to-face encounters, but that doesn’t mean you can’t have a productive visit virtually. It’s just another venue to deliver the evidence. I really do believe that it’s better to be in person, but delivering the evidence, no matter what the platform, is better than having a provider not know what they need to deliver the best care. Anna: You’ve carried out this traditional, in-person model for over 16 years – what challenges have you faced when detailing providers virtually, especially during the pandemic? Mary Liz: Time has been a barrier due to the overall stress on the healthcare system. There are also more distractions when visits are done virtually because providers are taken out of a controlled office setting. A provider could be home with their kids, or even driving in a car during a visit. You never know where a provider will be during a virtual detailing visit. Some offices in my area also aren’t picking up their phones, so you can’t have conversations on the phone or "stop in" for a cold call. Having a scheduled in-person visit with a provider is much easier than trying to connect with a provider over Zoom. You add another step to your process when you have to work through technology glitches. Virtual platforms or telephone calls can also be difficult for providers who are visual learners. You need to be creative with the way you share materials. But there are many similarities to in-person visits; no visit is “one-size-fits-all”. You need to consider the provider, their situation, and their environment and decide what will be the best way to deliver the evidence.  Anna: You’re right! It’s never one-size-fits-all when it comes to academic detailing. This has become even more evident as programs around the world have pivoted to e-Detailing. Do you believe that virtual visits can be as effective as traditional, in-person visits? Mary Liz: I do. It may not be as personal as an environment, but if you have a relationship with the provider, it shouldn’t matter whether it’s in person or virtual. I would continue to detail virtually in the future if a provider requested it, but I do favor in-person visits – it’s what I’ve done for so many years and I’d rather see the providers face-to-face. You get even more out of a detailing visit when you have that interaction. Anna: There’s certainly something to be said about the impact of the original model’s focus on in-person, 1:1 interactivity; it’s what has been studied for many years as effective and impactful. In a time where being flexible is critical, what are some tips you would offer to detailers during this time? Mary Liz: It’s crucial that you’re attentive to the provider you’re detailing. Continue to focus on the needs assessment. While you need to communicate your key messages, if you aren’t doing a proper needs assessment, you aren’t operating under the guidelines of academic detailing, which is all about listening and being interested in how someone is practicing. This leads you to be able to provide the evidence in the most effective way. Also, remember to be patient with providers! They’re still adjusting to this new world and they may even have questions about the impact of COVID-19 on the future of healthcare, as well as on their place within the healthcare system. Mitigate that impact by offering providers community resources that will support them through the pandemic – if you do that, then you’re fully realizing the true purpose of academic detailing as a supportive service that’s customized to real-world challenges.  Biography. Dr. Mary Liz Doyle Tadduni’s background has included critical care and medical-surgical nursing, nursing administration, and hospital administration in major university teaching hospitals in the city of Philadelphia. Dr. Doyle Tadduni is a training facilitator at NaRCAD, and an academic detailer with the Independent Drug Information Service of the Alosa Foundation. Dr. Doyle Tadduni is a BSN graduate of DeSales University. She completed her MSN, with a concentration in Nursing Administration, from Widener University. Dr. Doyle Tadduni was awarded the MBA degree, with a concentration in Healthcare Management Services Administration, from Widener University where she was the recipient of the Healthcare Management Services Administration’s Student Excellence Award. Following her graduate work in both nursing and business, Dr. Doyle Tadduni completed her administrative residency at the Hospital of the University of Pennsylvania in Philadelphia. She completed her Ph.D. in Nursing from Widener University. Dr. Doyle Tadduni presented her doctoral research, “Terrorism Preparedness: Perceptions of Connectivity of Emergency Nurses of the Emergency Nurses Association,” at the 10th Annual Interdisciplinary Research Conference in Dublin, Ireland. Overcoming the Impossible: Pivoting to Meet the Needs of Family Physicians During COVID-196/10/2020 An interview with Lindsay Bevan, MScHQ candidate, Project Manager, Primary Care Academic Detailing Service, Centre for Effective Practice by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: COVID-19, Detailing Visits, E-Detailing, International, Program Management  Anna: Hi Lindsay! Thanks for chatting with us today about the exciting work happening at Centre for Effective Practice (CEP) in Canada. Can you tell us about your role and share some highlights from your team’s recent work? Lindsay: I’m the manager of the primary care academic detailing service at CEP. We have a provincial service, which started in March of 2018 that serves family physicians across Ontario. Prior to our current service, we have run services in long-term care to support appropriate prescribing as well as primary care to support diabetes management. Our current service is still growing, but we’ve served just over 880 family physicians to date. Our focus has mainly been around opioids and chronic pain. We were just about to launch a series of “visits” (campaign topics) on prescribing in older adults, but we quickly pivoted to meet the needs of family physicians and began working on a visit around managing primary care in the COVID-19 context.  Anna: It’s so important to understand and meet the needs of family physicians when it comes to academic detailing, especially during a tremendously stressful time. Can you tell us a little bit more about the COVID-19 visit and the process behind its launch? Lindsay: Our provincial government declared a state of emergency in Ontario on March 17th, so we knew COVID-19 would be top of mind for our physicians and that they’d need more information. We also knew that we’d have to deliver the visits virtually, which was a fairly new territory for us. We had to modify our usual content development and detailer “upskilling” (bringing detailers up to speed on the content, key messages, and evidence around the topic) processes in order to meet the demands of family physicians by getting them information around COVID-19 when they needed it. The content development process for our other visits typically takes six months, with the detailer upskilling taking the last month and a half of that six-month period. COVID-19 turned everything upside down and made us rethink what we assumed was impossible. Within two weeks of the declaration of emergency, we started pulling together content for our COVID-19 resource centre (clinical tool for this visit, which is also available to all primary care providers), one week later we started training our detailers and within a month, we were delivering virtual visits to family physicians.  Anna: It’s impressive how quickly your team was able to launch this visit. COVID-19 is different from other topics that your team has focused on because the information and guidelines are continuously changing. How has your program kept detailers up to date? Lindsay: The detailer upskilling process for other visits includes weekly webinars to review key messages and the surrounding evidence, and a two day in-person workshop where detailers get to practice their visit discussions with each other and family physicians prior to launching visits. We also use a content development team for our detailing tools and bring those tools to the detailers to review when they’re about 90% complete. We typically don’t edit or change those tools after visits have begun. For our COVID-19 visit however, the detailer upskilling weekly webinars and the content development for our ever-evolving online COVID-19 resource centre have been continuous, ongoing processes. Our detailers have also taken on a larger role within both processes. Each detailer has been responsible for searching for, appraising and synthesizing information on a specific sub-topic of COVID-19, and then submitting this information for inclusion in our resource centre as well as presenting it at our weekly webinars to their fellow detailers. Our detailers need to be up-to-date on the emerging and evolving evidence and jurisdictional guidance around COVID-19 because family physicians don’t have time to sort through all the information being made available to them daily during the outbreak. Anna: It’s critical to provide physicians with the most up-to-date information, especially in situations like the COVID-19 pandemic where they’re bombarded with new recommendations and guidelines from multiple sources on a daily basis. How many COVID-related visits has your detailing service provided to physicians during this time? Lindsay: We’ve had 95 initial visits to date and approximately 12% of those visits have been with physicians whom we’ve never detailed before. We’re just starting to reach back out to physicians to see if they would like a follow-up visit since evidence has evolved and challenges have changed since we first started. The initial conversations were focused on testing, assessing and managing patients with the virus, and we’re now seeing those conversations shift to focus on resuming primary care services within the COVID-19 context. The detailers have done an amazing job in transitioning their detailing conversations to ensure they’re always covering the emerging areas of interest and need for family physicians. We’ve seen little to no requests from physicians for detailing visits on anything but COVID-19 or on maintaining care in the context of COVID-19, which speaks to the impact this topic has had on family physicians.  Anna: Wow – it’s amazing that your service has been able to detail so many physicians on COVID-19 while also recruiting new ones. Lindsay: Yes, overall, the visits have been well-received. We were a bit more cautious with our approach to promoting our COVID-19 visit and recruiting new family physicians. We didn’t want to add to the current noise at this time. Instead, we took a more passive but strategic approach, like adding a banner to our website where family physicians can quickly sign up for a visit, and having our partners share our visit and resource centre with their membership base. One of the neat things about this visit is that because we’re offering it virtually, we’re able to expand our geographical reach and provide our detailing service to more physicians.  Anna: Using a virtual platform certainly has its pros, especially within the world of academic detailing! What has your program’s experience been like with integrating e-Detailing into your service? Lindsay: The transition wasn’t unsurmountable for our detailers because they are quick learners, and we’ve had a lot of support through the resources offered by NaRCAD and our partnership with the Canadian Academic Detailing Collaboration (CADC). We also did internal virtual training sessions with our detailers where they were able to practice using all the features of the Zoom videoconferencing platform. Overall, it’s been a positive learning experience, and one that has furthered our team’s ability to be adaptable and enhanced our problem-solving skills. We do feel however that there’s been an impact on the detailer-physician relationship since we’ve transitioned to virtual detailing, especially for the 12% of family physicians who are new to our service. When a detailer is in a physician’s practice, they can see how busy a waiting room is or how stressed the staff appear to be. When family physicians join a virtual detailing visit, it’s much harder to gauge what kind of day they might be having and adjust the discussion accordingly. Furthermore, the act of going into a physician’s practice itself can create goodwill that helps establish and strengthen the detailer-physician relationship, and that opportunity is lost during virtual detailing.  Anna: That’s an excellent point. Observing the waiting room and interacting with office staff is also essential to a detailer’s needs assessment. Detailers lose this piece of a visit when the detailing is done virtually. Is virtual detailing something that CEP will continue doing once COVID-19 related restrictions are lifted? Lindsay: Our detailers and family physicians would like to return to in-person visits. There seems to be some conversations that lend themselves better to virtual communication, and others for which an in-person presence offers greater value and impact. When it comes to relationship building, in-person interactions still offer something special. We would also like to build off the momentum we’ve started with our virtual visits. We’re exploring the idea of offering virtual detailing to family physicians who would otherwise have their visit rescheduled due to extreme weather or to family physicians located where we don’t already have a detailer covering the area. We’ve all done what we thought was impossible in providing the majority of healthcare visits virtually. I hope that folks across the healthcare system will continue to use that momentum moving forward to increase access to care.  Biography. Lindsay Bevan works for the Centre for Effective Practice (CEP) where she collaborates with a team of amazing individuals to develop and implement evidence-based supports and services to help narrow the gap between best evidence and care in Ontario. As a project manager, she oversees the planning and implementation of the CEP’s primary care academic detailing service, which serves family physicians across Ontario. Prior to joining CEP, Lindsay worked at the University Health Network in the infection prevention and control unit, where she updated internal infection control policies and developed patient and provider educational material. Lindsay is currently completing her Master of Science in Healthcare Quality at Queen’s University. An interview with Megan DeNubila, Provider Relations Manager, and Jessica Alward, Academic Detailer, from the Bureau of Infectious Disease Control with the state of New Hampshire. Their mission is to improve public health by promoting evidence-based practices in the areas of infection prevention, screening, testing, and management for HIV, TB, STD/STIs, and Hepatitis. by Winnie Ho, Program Coordinator Tags: Detailing Visits, HIV/AIDS, Rural AD Programs, Sexual Health, Stigma  Winnie: Thank you both again for joining us today! In one of our past technical assistance discussions together, we’ve gone into depth about some common clinician stigma and barriers. In particular, you shared with us that because New Hampshire was a lower incidence state for HIV, you would encounter clinicians who felt that that particular issue didn’t really fall within their patient population. It’s a common barrier we hear from many detailing programs, whether they address opioid use disorder (OUD) or infectious diseases. Can you go into more depth about your experiences with this phenomenon, and how you’ve addressed it? Megan: Providers are extremely busy, and they’re often expected to be an expert on so many topics. Our program helps bring providers filter through new information so they can start to bring it up with their patients. By walking them through the best practices, the recommendations, and local and state-specific data, we can show them that it’s something that is impacting their patient population. In addition, one of the things that stuck with me from the NaRCAD training we attended was that because there’s so much new information, providers would be expected to read up to 17 papers a day just to stay current. Something like HIV would be one of many things that providers are concerned with on a daily basis. Our job is to help bring the most relevant and evidence-based information to the surface for them and their patients.  Jess: Megan is completely right on this! I’m in provider offices a lot. What I hear is that they often feel like they're just treading water and not able to keep up with new information. What we try to do is bring that info to them in a way that doesn’t feel like just one more thing to squeeze into a day. When we talk to them about stigma, we don’t want to start there. We want to start with some easy and really useful information and tools that will make their job easier. By doing that work first, they feel like the precious time they are giving to us is worth it. After a couple visits, emails, or phone connections have happened, that's the time to bring up new approaches and topics. Winnie: I really appreciate that your lens on this barrier embodies a ‘How do we best support you?’ attitude. The goal of academic detailing is to navigate and close knowledge gaps in hopes of changing clinician behavior. Sharing knowledge and having difficult conversations is our best tools to address clinician stigma and discomfort. It’s not a battle against them and certainly the goal isn’t to shame clinicians. This is a collaborative operation to improve health outcomes.  Megan: Right, in the end, our mission is to close health inequities altogether. If I were a clinician and wasn't comfortable or familiar with best practices for preventing HIV, then I might feel a high level of hesitation trying to broach something like taking a sexual history from my patient. But if it’s something that I get more comfortable with, I’m more likely to bring it up and ask the right questions. Ultimately, we’re trying to build a relationship with the provider so they see us as a resource when a new practice, tool, or clinical guideline comes out. They can then use those tools and information to address stigma that a patient may be experiencing. Providers constantly have new information and guidelines thrown at them, and we would like to help make it easier for them to take that information and apply it in their daily work.  Jess: Whenever I address something uncomfortable with a provider, stigma or otherwise, I try to create an environment where we can work collaboratively on the issue and the provider feels as though I am a resource for them. I will say something like, ‘the last we talked, you mentioned this to me and it really got me thinking….” Or “I was talking with a colleague the other day about….” Then I will find a way to circle back around to the original topic. By approaching the topic in this manner allows them to feel we are a partner and have a shared goal. Winnie: I want to circle back to your team’s mission of addressing health inequities. Inequity is the core of why we discuss things like stigma and discomfort. We need to approach clinician stigma with a human approach, but we also need to address the very real impact that it can have on patient health outcomes.  Megan: In a mostly rural state like New Hampshire, healthcare access is limited to begin with, and clinician stigma could drive patients who need help to either forego care or have to travel very far to seek care that they are comfortable with. We know providers want the best outcomes for their patients, and through detailing, we want to help the providers achieve those outcomes. Looking at potential stigma is one of the keys to making sure we address health inequities. Winnie: A lot of these experiences about clinician stigma are anecdotal, but as you just outlined, they have a very real impact on health outcomes. From our previous call, we have discussed and imagined a tracking tool for these encounters with clinician stigma and barriers. What would you find useful about a tracking tool like this, and what would you hope to learn from the data?  Megan: A tracking tool would help us better understand and represent the stigmatic responses that are out there. It would help us focus our efforts to help a provider address stigma in their practice. Anecdotes are helpful, but it can be hard to grasp. We don’t want to make decisions by theorizing what patients are experiencing. As a small state program with limited resources, this would help us optimize our response and to make sure we’re heading in the right direction by seeing if stigmatic behaviors change. Winnie: It would be extremely exciting to see a tool like this become available and specialized for the hundreds of detailers who do this work. Megan: Yes, it’s a theoretical tool at the moment, but we were in discussions prior to COVID-19 about how to develop it. It would be amazing to see programs collaborate on something like this. I can only imagine how much further we’ll go with that as a resource. Biography. Megan DeNubila is the Provider Relations Manager for the Bureau of Infectious Disease Control, New Hampshire Division of Public Health Services. She has been leading the Public Health Education and Detailing team since August of 2018. Megan has over 8 years of public health experience in capacity building, coalition development, and community health. She earned her Master of Public Health degree from the Boston University School of Public Health with a concentration in Maternal and Child Health in 2016/2017 and her Bachelor of Arts degree in Health: Science, Society and Policy from Brandeis University in 2012.  Biography. Jessica Alward has been with the State of New Hampshire Division of Public Health Services for almost two years and recently earned her MS in Homeland Security and Emergency Management. With a background in education and training, she works full time as an academic detailer all over the state. In her spare time she enjoys directing community theatre productions, running and hiking. She is married to Scott and mom to two grown sons. An interview with Nadejda Razi-Robertson, PhD, LCSW, Managing Director, Synergy Health Consulting and Andrew Suchocki , MD, MPH, Medical Director, Clackamas Health Centers by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: COVID-19, Detailing Visits, Opioid Safety, Rural AD Program, Stigma, Substance Use  Anna: Thank you Nadejda and Andrew for spending time with us today to discuss the impressive work being done in your leadership roles around practice transformation at Synergy Health Consulting. Can you tell us a little bit about Synergy and its impact on opioid safety-related care improvement? Nadejda: Our team works with health systems across the state of Oregon. Our first phase of work started several years ago when we were largely focused on helping systems implement the CDC guidelines around opioid safety. Our work has since evolved, and we’re now focused on helping clinicians develop medication-assisted treatment programs, integrate behavioral health into primary care, and address the opioid epidemic at the community level. We often use academic detailing as one of the many tools in our toolbox when we work with different health systems on opioid safety. We take the basic concepts, such as conducting a needs assessment and identifying clinician barriers, from the traditional model of a detailing visit, and implement them on a larger scale. Andrew: Many members of our team are practicing healthcare professionals in the field, which roots a lot of our work at Synergy. I take what I’m seeing on the ground as both an administrator and a provider at a busy clinical practice and incorporate those experiences into my work at Synergy.  Anna: It’s so important to build teams where members have varied expertise and professional training when working together on practice transformation. How have you incorporated academic detailing strategies into the work being done at Synergy, and how has it been received? Andrew: Some of the academic detailing work I’ve done has been with providers who need extra support from a peer, or from someone else working in the field. When it comes to opioids, chronic pain, and addictions in primary care, there’s a tremendous amount of stigma and information that was accurate at one time, but as we’ve shifted as a society, many primary care providers are yet to catch up. Stigma isn’t something that folks are actively choosing, it’s more of what they’ve been taught. Changing that culture of practice is much more difficult compared to asking prescribers to prescribe cholesterol-lowering therapy. There’s very little societal baggage when it comes to improving cholesterol than there is when it comes to destigmatizing addictions or chronic pain.  Nadejda: We use the same fundamental approach when working with systems, clinics, or individuals. We start with a needs assessment, provide a group training based on those needs, and follow that up with 1:1 academic detailing visits to address barriers, provide materials, and explore personal bias that may be getting in the way of providing treatment. I’m currently working to schedule a training for several providers in a rural county in Oregon. A number of those providers are X waivered (allowing them to prescribe medication therapy for patients with opioid use disorder), but they aren’t using their X waivers to prescribe buprenorphine. A needs assessment will provide me with a better understanding of what the challenges and barriers are, what is working well, and where there may be bias, stigma, or gaps in knowledge. We also use the needs assessment as a “listening session” that creates a sense of safety, fosters an experience that participants are being heard, and serves to “normalize” experiences across settings and practitioners. This process is also strategic in that it helps us understand where to focus our educational outreach and academic detailing efforts. The more we are doing this work, the more we are finding that this approach is effective in getting care teams, medical providers, and service providers across many sectors into increased “philosophical alignment” which is critical to effectively foster culture change around issues of pain, addiction, and trauma.  Anna: Bias, stigma, and gaps in knowledge around chronic pain and addiction are common, especially in primary care. We’ve found that many detailers have been successful in helping providers “catch up” to society and overcome personal bias through their detailing visits. Speaking of detailing visits, face-to-face visits have clearly been impacted by COVID-19. Can you tell us more about other ways that COVID-19 has impacted the work at Synergy? Nadejda: Again, we’ve gone back to the wisdom of the original academic detailing model. The needs of each setting have changed significantly, and we’ve been pivoting our work to meet those needs. Providers want to know how to best support their patients who are dealing with pain during this time. One thing we were able to provide early in the pandemic was a list of recommendations and resources around pain management for both providers and patients.  Andrew: We saw the need to adapt to massive changes related to COVID-19, and to do so essentially overnight. We’ve had questions about conducting urine drug screenings, initiating treatment over the phone, and maintaining the patient-clinician relationship. There’s also a shared vulnerability among providers and patients when visits are conducted virtually. Our patients have had requests for increased medication use, which is understandable because they’re not able to do activities that they’ve typically been able to do to keep themselves resilient. That conversation is a difficult one - in some ways it is easier because you don’t have to see someone in person, but it also makes for a very ineffective conversation because you’re not able to demonstrate your humanity through body language. Our team is struggling to wrap our head around this as we try to provide leadership and guide clinicians who are looking to us, or our state, for collective ideas around this field and how we practice.  Anna: COVID-19 has certainly impacted the way we think about responding to changing needs for those who are trying to manage their pain. Can you tell us about some of the other major changes you’ve seen in pain management over the past few years? Andrew: The biggest thing I’ve seen is insurance expansion. We’ve known for years what you need to have effective pain management and how important it is to shift the idea of living with pain and accepting pain versus eliminating pain. We’ve seen Medicaid expansion and expansion of benefits, especially in the Northwest, that has given patients access to modalities that are effective for safer pain management. Historically, things we knew that worked like, gym memberships, physical therapy, occupational therapy, mindfulness, and chronic pain groups, were never paid for or weren’t available. As society has changed how it believes pain should be managed, we’ve started to see the insurance side supporting these modalities more. There’s also been heavy reporting on the opioid crisis in the media that has led patients to understand that opioids have risks. Nadejda: We’ve continued to grow and learn as a team over the past several years. Our entry point into communication around chronic pain and pain management has continued to be centered around assessing if patients and their care teams have an understanding about how pain works. We want to make sure that clinicians have the proper training and are up-to-date on evidence and resources. Andrew: We’ve known some of this information about pain management and how pain works for a while, but it takes many years to take what we know from as a research perspective and translate it into practice. One of our roles at Synergy is to accelerate that. We’re seeing our evolution as a group mimic and reflect the experience we’re having as a culture as we start to dial in to the most effective ways to manage pain.  Anna: As Synergy continues to respond to changing societal needs around pain management, what insights can you share about the impact of academic detailing to date? Andrew: One thing I’ve learned about academic detailing is that it’s only as effective as your intervention across an entire system. I’ve realized that any work that I’m doing is irrelevant unless I’m addressing the entire system and the culture. If the front desk staff isn’t on board, if the medical assistant isn’t a believer, if the nurse doesn’t understand addiction, if the CEO doesn’t understand that the health system is already treating these patients, there will be challenges that will be harder to overcome. Nadejda: Because academic detailing has been an arm of a larger change approach we’re using, it’s hard to measure its effects. We don’t have data to show that only detailing has moved the needle around these topics in these ways. Sometimes I see academic detailing as the “cherry on top” after there’s a lot of work that’s been done in prepping a system. I’ve recently been doing practice facilitation work with providers and clinics just to understand the barriers in a system—there’s an art to the change process in the pain management space. Academic detailing comes in after you’ve truly understood what the barriers are. After you understand the barriers, you can bring in nuggets of evidence and information in a way that the system is ready to receive.  Biography. Nadejda Razi-Robertson is the Managing Director of Synergy Health Consulting, as well as Synergy’s project lead for the Oregon Health Authority’s Prescription Drug Overdose Prevention Project. Nadejda is a practice facilitator within health systems around the State of Oregon and provides technical assistance to clinics that are focusing QI efforts around safe opiate prescribing, MAT program development, and behavioral health integration. Over the past twelve years, she has worked in private practice with a specialty in trauma treatment, as a behavioral health provider in two Federally Qualified Health Centers (FQHCs), and as a consultant with Oregon’s Coordinated Care Organizations (CCOs) and the Oregon Health Authority supporting efforts in addressing the opioid epidemic throughout the state of Oregon.  Biography. Dr. Andrew Suchocki is a family physician with additional training in Preventive Medicine. He has worked in underserved medicine with a focus on chronic pain and addiction for ten years, and has been a medical director at an FQHC in the Portland, Oregon region for the past five. Andrew provides educational outreach and consultation in the areas of system change in primary care around opiate prescribing, MAT system design and capacity growth, coordinated specialty care, and reducing risk. Dr. Suchocki is an Oregon Opioid Prescribing Guidelines Task Force member and Oregon Medical Board consultant. He provides technical support and academic detailing for the Oregon Psychiatric Assistance Line (OPAL) which provides immediate referral sources for primary care. Dr. Suchocki also provides strategic planning, creation of innovative clinical decision support tools, physician mentoring, and health system process mapping for Yamhill County Health and Human Services, Community Corrections and Specialty Behavioral Health. He is a regular presenter at national and international pain related conferences. An interview with Elisabeth Fowlie Mock, MD, MPH from the Maine Independent Clinical Information Service (MICIS). by Winnie Ho, Program Coordinator Tags: Detailing Visits, Opioid Safety, Stigma, Substance Use  Winnie: We appreciate you taking the time to speak with us today about the work that MICIS (Maine Independent Clinical Information Service) has done supporting evidence-based prescribing since 2008, and safer opioid prescribing since 2016. Can you tell us a little bit more about MICIS? Elisabeth: We’re a small program created by legislation in the state of Maine, housed within the Maine Medical Association. We serve over 8600 prescribers including physicians, pharmacists, nurse practitioners, and physician assistants across the entire state. Our two detailers are contracted to work about 5 hours a week each, which includes all of our administrative and detailing time. Winnie: That’s an amazing feat to be serving such a large population with a small team. How have you built and maintained all of those relationships?  Elisabeth: We have always used more of a general educational outreach approach than the traditional one-on-one academic detailing model. We have limited resources with our contract, and the only way to reach that number of prescribers is to do small groups or lectures. Winnie: We understand that there are many programs who adapt the original model of detailing to allow for more than one provider at a time to participate. While it’s a common workaround solution to having limited resources and a long list of providers to detail, it can be more difficult to discuss challenging topics, especially something like opioids and related stigma. How have you been able to navigate those challenges?  Elisabeth: When we detail in our groups, we focus on small group discussions. One method I use involves flashcards with myths or biases about Opioid Use Disorder (OUD) and Medication-Assisted Treatment (MAT), and asking two or three of the attendees to discuss that amongst themselves. We have also used a language sheet that guides providers in what to say. We have people talk about the language commonly used in practice, and how that can affect the care that’s provided. I think just like any other place, we encounter people who have all of the biases that you’ve heard of when it comes to opioid use disorder – that it’s not a disease, that buprenorphine and methadone are just trading one drug for another. Winnie: There must be a lot to unpack when discussing the root of where these beliefs come from. It’s a core component of what we hope to achieve through academic detailing – an honest dialogue that leads to positive clinical practice outcomes.  Elisabeth: Exactly. I think it’s important to understand that, for example, with chronic pain prescribing, there are a lot of people who are reluctant to embrace evidence from the past five years that shows no benefit from opioids, and more significant evidence of harm. It’s been interesting to see how people have been stuck on what they learned twenty years ago, and to see them reject the newer information. Winnie: It’s incredibly important that detailers remember in navigating tough conversations about stigma that there is a shared goal of promoting patient health. No provider undergoes training and hard work with the intention of harming patients.  Elisabeth: I think these tough conversations can produce some cognitive dissonance in people. Basically, if I, as a physician myself, agree with the premise that what I did fifteen years ago actually contributed to OUD in my patients, and if I admit that, then I also have to carry a burden that it was my fault. It’s a hard jump for people who made it their life’s work to care for people. Winnie: It’s absolutely a human response. What have you found to be an effective way of addressing the problems caused by stigma, while also addressing the fact that providers are human? Elisabeth: People don’t want to be overwhelmed by data, but repeated snippets of data over time can help you reinforce the message, which is what we do with academic detailing. I think of myself in my work as a physician – I started on opioid education projects more than half a decade ago. It wasn’t my top choice, but I became more and more educated about the crisis and heard the information in multiple ways. It really changed my way of thinking to the point of realizing I needed to be part of the solution. I received my X-Waiver back in 2016 and started prescribing buprenorphine.  Winnie: That’s a wonderful reflection on how repeated messaging helped change your mindset as a provider. It’s important to understand that people can change, no matter what holds them back. Elisabeth: I think that as academic detailers, we might not always recognize the impact right away. We might not get the immediate positive feedback from a clinician after an interaction, but especially if you’re lucky enough to grow relationships with the people you detail over time, you can see the change. I think that’s the most effective and rewarding part of detailing. I prescribe buprenorphine because I can teach about it, but I also do it because it’s important. This work gives us an opportunity to be leaders for people who don’t always have a voice, and because of stigma, aren’t being listened to. Most of our patients with OUD are on the margins and struggle even during stable economic times. Especially right now with the COVID-19 pandemic, the rest of the country may not be worrying about how we’re going to safely maintain our patients on buprenorphine, but we need to worry about it.
An interview with Terryn Naumann BSc(Pharm), PharmD the Director of Academic Detailing and Optimal Use at the British Columbia Ministry of Health by Winnie Ho, NaRCAD Program Coordinator. Overview: Terryn previously spoke about her experiences on a virtual detailing panel at the NaRCAD2019 conference. You can watch the video recording here. Tags: Detailing Visits, E-Detailing, International  NaRCAD: Terryn, thank you so much for speaking with us today about your experiences with detailing in the province of British Columbia. The BC Provincial Academic Detailing (PAD) Service certainly has a lot of ground to cover. Tell us about the program goals and geography. Terryn: For reference, British Columbia is geographically larger than Texas, but the population of British Columbia is only about 5 million people. We provide our detailing services to family practice physicians, nurse practitioners, and a few other healthcare professionals. Our detailers each do more than 175 visits per year, and collectively, they see about 2000 providers per topic, which includes about a third or so, of all the family physicians in BC. We have 12 detailers in total, half of whom are working in less densely populated areas. For example, the northern end of the province is mostly small communities with only 3-4 providers in each town. One year, one of the detailers drove over 17,000 km (10,563mi) for her visits alone!  NaRCAD: That’s an incredible amount of work that your detailers have been up to! And you yourself have been active in AD for a long time. What was your experience then like? Terryn: I started in 1993 with the program that would one day expand to become the PAD service, and I detailed for about 7 years. I came back to academic detailing in 2008 as the coordinator of the provincial program. When I started in 1993, I had just graduated with my PharmD. I had read about AD and was excited to try something new. You have to realize, at the time, technology wasn’t that advanced... I didn’t even have an e-mail address when I first started. You couldn’t just send people a note and say “When would you like to meet?” It wasn’t simple to access people. NaRCAD: How would you describe how AD has changed since you started?  Terryn: When I started, I was the first academic detailer in Canada. There were about 70 physicians that I would go out to visit for each of the topics I put together after having the content reviewed by a local physician specialist from within our own community. One of the things that has changed is the breadth of resources and the growth of the AD community. There are so many more people involved, content is more thoroughly researched, and the literature is more readily accessible through technology. NaRCAD: Technology has certainly changed the way the world works, and it’s something that detailing programs are turning to more and more to tackle the challenges you’ve mentioned, such as trying to serve a large and scattered population with a limited team. We’ve seen the increased use of tele-communications to do detailing. What has your experience been with virtual detailing, also commonly called ‘e-detailing’?  Terryn: One of the things we value about AD is that truly interactive, face-to-face encounter and that ability to individualize sessions to the provider’s learning needs. Virtual detailing uses a different methodology altogether. I think there are advantages to virtual detailing, but sometimes I think that it’s not as simple as moving AD to a web platform. I worry about the personal elements you can lose, even when using a web platform where you can see each other. My detailers often end up making slides of the original materials, which sometimes turns the session into more of a presentation. NaRCAD: Can you elaborate further on the nuances you’ve seen with this new approach? Terryn: We started with something we called Technology-Enabled AD (TEAD) which was a limited study done to compare the efficacy of TEAD versus a traditional face-to-face visit. They found that there was an effective knowledge exchange during both types of sessions, but the time it took for TEAD was far shorter. However, when we added TEAD as an optional feature for our providers, we ran into multiple challenges, such as detailers and providers not being familiar enough with the technology. The large majority of our providers choose to meet in person when they have that option.  That said, virtual detailing has been useful considering BC’s terrain and rough winters. Some regions have winter 8 months of the year and travel is limited for safety reasons. We have used virtual detailing, but find that we need detailers that are tech-savvy and can guide providers through accessing the platform easily. The key is maintaining the interactivity component and having the session not become a presentation. If we can embrace virtual detailing as its own, unique skillset, we may be able to take advantage of all of its benefits. I think that we’re also at a changing point in technology – the next generation of providers (and detailers) will have grown up with and be more comfortable using technology. NaRCAD: There will be a lot of growth in detailing as we are able to incorporate more options into how we reach providers, with the emphasis being on building a strong relationship. Terryn: The goal of AD has always been to have a clinician who values a discussion about the evidence, and then is able to incorporate the evidence into their own practice and drug therapy decision making. E-detailing is just another modality for doing that. We found that virtual detailing is most effective after establishing a prior relationship with the provider during a face-to-face visit. We received fantastic feedback from one provider who felt the virtual detailing session that he participated in from the comfort and privacy of his home allowed him to ask questions he might otherwise have avoided asking in a group setting. If we can use technology to build relationships like that, then ultimately isn’t that what we want? I would say that it is.  Biography. Terryn Naumann is the Director of Academic Detailing and Optimal Use at British Columbia’s Ministry of Health’s Pharmaceutical Services Division. She earned her pharmacy degrees from the University of British Columbia and completed a hospital pharmacy residency at St. Paul’s Hospital in Vancouver. Terryn began her career in academic detailing in 1993 when she worked at Lions Gate Hospital in North Vancouver as the clinical pharmacist for the Community Drug Utilization Program – the first academic detailing program in Canada. Since 2008, Terryn has led BC’s Provincial Academic Detailing (PAD) Service, a team of 12 academic detailing pharmacists who conduct over 2000 academic detailing/small group learning sessions each year. She is a member of the Canadian Academic Detailing Collaboration, having served as chairperson and secretary. She has also been a facilitator at several of the Centre for Effective Practice’s Basic Academic Detailing workshops. Wearing Multiple Hats at Alosa Health: Detailing Clinicians, Managing Programs, and Training Staff1/22/2020 An interview with Tony de Melo, RPh, Director of Clinical Education Programs, Alosa Health by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Detailing Visits, Opioid Safety, Program Management, Training  NaRCAD: Tony, thanks for chatting with us today about your role at Alosa Health! What’s been the most exciting part of the work that Alosa has done this year? Tony: Our partnership with Aetna, a managed health care company and health care insurer. We’ve been working with them to provide educational outreach to providers on chronic pain, acute pain, and opioid use disorder (OUD); supporting them in managing pain using non-opioid drug options; appropriately dosing opioids when they need to be used; tapering down patients who are on existing high doses of opioids; and helping to identify patients that may have opioid use disorder. We’re now working in Pennsylvania, Virginia, West Virginia, Ohio, Illinois and Maine. NaRCAD: That collaboration does sound exciting! Now, let’s talk a little about your role at Alosa. You actively detail, you manage academic detailers in the field, and you lead trainings at Alosa. Which aspect of your role is your favorite, and why? Tony: When I’m training and managing detailers, I see myself more as a coach than a trainer. I’ve always liked educating and teaching—I enjoy helping others develop their skills and seeing them improve. Training folks and coaching them in the field is rewarding to me because I feel that I’m impacting what they’re doing in their own communities. It brings me happiness to see others succeed. NaRCAD: As a coach, how do you know when your work has been impactful? Tony: When I work with detailers in the field, I can see firsthand that they are able to be impactful with the providers because they are bringing about behavior change with their message delivery and confidence. We can also measure how impactful our work is by reviewing our Salesforce data. I can see from the detailer’s visit notes when providers have agreed to a behavior change, and this is a true measure of our work being impactful.  NaRCAD: With success comes challenges. What are some of the major challenges you see academic detailers face in training and in the field? Tony: The major challenge is teaching detailers to have a conversation with clinicians rather than a lecture. Making the visit more conversational doesn’t often come as naturally as presenting the information in a lecture format, but the conversation must be about understanding where the provider is now, what their needs might be, and how to deliver content to make behavior change. In the field, the major challenge is access to providers. Many health systems have regulations and restrictions for those who want to meet with providers, because representatives in the pharma industry have bombarded and overloaded providers throughout the years. As a result, we’re often seen as an outside influence or an outside visitor, so we aren’t always given the opportunity to meet with a provider. NaRCAD: With these challenges in mind, how do you instill confidence in academic detailers as a trainer and as a manager? Tony: We spend a lot of time practicing and providing feedback during trainings. We practice individually, with partners, and with outside folks who are playing the role of providers. Practicing multiple situations, multiple times, over multiple days, builds confidence. We also videotape the trainees so that they can see what they’re doing well and what they can improve upon. As a manager in the field, it’s quite similar. I usually sit down with each detailer after a visit and discuss what worked well and what they could do differently in their next visit, so that each visit becomes a learning opportunity. Providing feedback and being a mirror for the detailers helps them to build confidence and skills as time goes on. I also offer the detailers my perspective; having spent time doing this myself and observing others, I can share the tricks, skills, and wording I’ve heard throughout my time with the detailers.  NaRCAD: Those are all great ways to build confidence among detailers. What’s one piece of advice that you would give to academic detailers? Tony: Don’t be afraid to ask for a specific behavior change, and remember to follow up to make sure that the behavior change occurs. One thing that I find to be hard for academic detailers is the “ask”, where detailers are asking for commitment or behavior change from a provider at the end of the visit. I always tell detailers to frame it as, “based on what you’ve heard today, what is one thing you’d do differently?” Follow-up then ensures that providers are committed to change and holds them accountable for what they said they would do. NaRCAD: That’s extremely helpful advice for detailers. What’s the best thing a program manager could do to maintain high levels of engagement among detailers? Tony: As a manager who’s coaching or guiding others, it’s important to build trust between yourself and the folks you’re coaching or managing. It can be lonely when you’re in the field detailing by yourself, so managers need to have touchpoints with their detailers. Building trust and having your detailers know you’re all working together helps them stay self-motivated; it makes them want to go out into the field and do a good job because they know someone is backing them up. NaRCAD: Thank you for taking the time to chat with us today. We value your unique perspective on detailing, managing, and training!  Biography. Tony de Melo manages field staff and leads academic detailer trainings at Alosa Health. He attended Massachusetts College of Pharmacy and Health Sciences in Boston, where he received a BS in Pharmacy with a minor in Business Administration. This business interest led him to work for several pharmaceutical companies as a sales representative, account manager, training manager, district/regional manager, associate director of managed markets training, head of sales training, and development & marketing product manager. He has also worked for smaller businesses that were looking to grow their sales and marketing programs. Throughout his career, Tony has successfully sold, marketed, trained, led, designed, developed and executed solutions to meet business objectives.  An interview with Rachel Lemons, Project Manager, ONE Tennessee by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Opioid Safety, Project Management NaRCAD: Thank you for taking the time to speak with us today—we’re excited to hear about you and your team! Can you tell us a bit about ONE Tennessee and how your organization first became involved with academic detailing? Rachel: ONE Tennessee is a state-wide nonprofit healthcare collaborative who is focused on fighting the opioid epidemic. We were founded as an outcome of a summit hosted by the Tennessee Department of Health called “Turning the Tide.” The summit joined together healthcare professionals and stakeholders to discuss best practices for tackling the epidemic. Academic detailing was highlighted as a best practice during the summit and it was collectively decided that it would become one of our initial projects. ONE Tennessee brought the academic detailing pilot program to life through the opioid crisis funding the Department of Health received from the Centers for Disease Control and Prevention. NaRCAD: We’re glad to know that the strategy of AD was highlighted! You’re now managing a program of detailers focused on opioid safety across the state of Tennessee—tell us what that’s like. Rachel: Exciting! Once our detailers were trained by your team, my role was very much supportive in nature. I helped our detailers to identify clinicians in their communities, and troubleshoot any issues. We were fortunate enough to be able to recruit a passionate group of pharmacists for our pilot, and that made my job easier from a clinical standpoint, since they’re the subject matter experts on opioid prescribing. They‘re on the front line of the epidemic, and they fit the perfect mold for engaging with clinicians to build a strong and trusting relationship. NaRCAD: You recently completed the pilot stage of your program. What would you say are some of the biggest lessons you’ve learned so far about building an academic detailing program? Rachel: Getting in the door was one of the biggest barriers our detailers faced. From a programmatic standpoint, I think ONE Tennessee could have done a little more foundational work for our detailers, like speaking with our stakeholders and educating them on academic detailing as it relates to the opioid initiative—that would have really helped our detailers gain access to clinicians. We also learned that time was a barrier for our detailers. Our initial grant period was only one year, and things moved very quickly. We recruited full-time community pharmacists, so having the bandwidth to prepare and complete academic detailing visits was often difficult, especially if there was limited employer support.  NaRCAD: Those are all familiar challenges across many of the programs we support. How did you maintain strong relationships with your detailers and support them in the work that they were doing in the field? Rachel: I always had an open line of communication with our detailers. We had standing monthly webinars, but it was difficult to find a time that worked for everyone because they were full-time pharmacists. Our detailers were scattered across the state and were mostly in rural areas, so I was not able to meet with them in person; however, I was available via email, phone call, and text message. I learned early on that I had to meet detailers where they were. Some detailers did not have time to check email, so it was easier to do a quick call at lunch or early in the morning before their day got started. It really depended on the needs of the detailer, but I always maintained an open line of communication. NaRCAD: That’s a great model, and regular communication helps detailers feel a sense of community through a project. Other supports are often more concrete, like tools and resources. What are some that you've found to be critical to program success, and why? Rachel: I think first and foremost, our partners, specifically NaRCAD, the Tennessee Pharmacists Association, the Tennessee Hospital Association, the Tennessee Nurses Association, the Tennessee Medical Association, and the Tennessee Department of Health, were a tremendous resource that made our program incredibly successful. Google’s platform (Google Drive, Google Sheets, and Google Docs) was also critical to our success, as it allowed us to share data and updates in real time. We did not have access to specific evaluation tools because we are a young organization and our grant period was only one year. Our shared space online helped me to stay organized and capture information from our detailers all in one place, and it was free!  NaRCAD: These are all great reflections for AD program managers to learn from. Based on the successes and challenges of this pilot, where do you see your program in a year? Rachel: I see us continuing our current model with our inaugural group of academic detailing community pharmacists while working towards designing, developing, and implementing a “train -the -trainer” model in partnership with your team. I also see us having discussions with large and small hospital systems to customize plans to fit their unique needs related to opioid safety. Most importantly, we want to continue to support the state and our other healthcare stakeholders who are with us on this journey. NaRCAD: We’re happy to help support that vision. Any other important advice/tip that you’d give to other young programs? Rachel: Patience. You must have an understanding that there are going to be pitfalls, but if you have the support and the right people involved, your program is going to succeed. Also, don’t try to reinvent the wheel if you don’t have to. There are so many other programs out there — reach out to people and have conversations! NaRCAD: Rachel, thank you so much for sharing your experiences with us. We're excited to see the impact of your program into the future.  Biography. Rachel Lemons found passion for public service early on in life. She is committed to assisting those with the greatest need in her community. She’s working to effect change socially and through public policy. She is a graduate of East Tennessee State University, where she received her Bachelor of Science in Public Health. Her involvement with Tennessee’s Opioid Epidemic began with the Department of Health, where she was exposed to the State’s rapid response in this fight which lead her to joining ONE Tennessee as a Project Manager. She continues to build her career with a practical and wide ranging set of experiences in order to gain a global perspective on health issues facing communities today. Rachel is an active member in the Junior League of Nashville, Tennessee Public Health Association and currently serves as the Board Intern at Cheekwood Estate & Gardens in Nashville. OVERVIEW: Boone County, West Virginia was one of 4 original site selected for years 1 + 2 of a pilot program of the CDC (Centers for Disease Control and Prevention), NACCHO (the National Association of County and City Health Officials), and our team at NaRCAD (The National Resource Center for Academic Detailing). This exciting pilot program focused on community-level work with local public health departments to develop customized interventions to reduce opioid overdose and death. Six sites experiencing significant public health problems related to opioids were selected over the two years to be trained in academic detailing; those trained health professionals then conducted 1:1 field visits with front line clinicians to impact behavior around prescribing, treatment referrals, and patient care, all within a rural area. As year 2 comes to a close, we’re showcasing stories from the field. Tags: Detailing Visits, LOOPR, Opioid Safety, Program Management, Rural AD Programs  Via NaRCAD, NACCHO, & the CDC’s pilot project, “LOOPR”, we were able to connect with high-burden counties across the U.S. whose rates of high prescribing and high fatal and non-fatal overdoses identified them as a county in need of support. NaRCAD worked on the implementation of an academic detailing initiative over the course of 2017-2019 with Boone County, located in rural West Virginia. Boone County ranks as the 22nd most vulnerable county across all counties in the United States, with the highest drug overdose mortality rate of all counties in West Virginia. Due to these and other data, Boone was identified as a key county in which to test the implementation of an academic detailing program, in which trained detailers would speak to clinicians and pharmacists about safer prescribing of opioids, checking the state’s prescription drug monitoring program to avoid dangerous co-prescribing of opioids and benzodiazepines, and to try and provide treatment, non-opioid therapy, and resources to patients in need.  One of the most unique approaches across all 5 sites of the LOOPR Project was carried out in Boone, with the team of 5 detailers being hand-selected from the nearby University of Charleston West Virginia’s School of Pharmacy. Four of these five recruited detailers were students in training to become pharmacists; one detailer works at the university as a professor of pharmacy. Selecting pharmacy students and faculty allowed for many positive approaches to the project, as well as creating unforeseen challenges. Programs considering hiring student detailers can often rely on the flexibility of students’ schedules, as well as an enthusiasm and energy for learning that may exist in smaller quantities later in one’s career, when full-time roles in healthcare take priority. While many career-established clinicians may have little room in their schedules to squeeze in 1:1 sessions with fellow clinicians, students may have more of an ability to shift their schedules, especially if they are not yet carrying out residency.  a reflections from Boone County’s Detailing Team, it’s clear that best practices in detailing should also consider the vast amounts of new information that students are absorbing early in their learning careers, and that learning clinical content may take longer to grasp. In addition, the comfort level with new clinical information may lead to less confidence in discussing best practices, especially with clinicians whose careers are much more established. Finding the right balance of tenacity, communications savvy, more time to ramp up to comfort in delivering and leading 1:1 sessions, an additional amount of technical assistance provided at more frequent intervals, and additional practice time or shadowing time with a mentor, can all benefit student detailers who are training to join a clinical outreach education team in a high burden area. With these elements in place, a student detailer may be poised for success—however, other considerations include the fact that students may have new projects, graduation pending, or life events which may end up limiting their ability to dedicate consistent time to a project rolled out over many months.  Other reflections from the Boone County AD Team included looking carefully at the social climate in which AD interventions of this nature may be implemented. While no county is free of potential clinician-level or community-level stigma, particularly around issues such as opioid use disorder, Boone’s AD team shared a particularly challenging setting within which the local community was not as supportive of evidence-based harm reduction initiatives as would be beneficial. One detailer’s suggestion to raise the visibility of and advocacy for harm reduction included considering a public health campaign prior to a detailing campaign, to ensure that subsequent roll-out of detailing is more sustainable and met with an openness from clinicians to consider behavior change. NaRCAD’s work with the public health department in Boone County, in partnership with the students and faculty of University of Charleston, West Virginia, provided the kinds of insights critical to learning from a pilot project of this nature. As with many pilot studies, any information gathered can illustrate a clearer picture of the landscape within which public health initiatives can be implemented, so that future projects may have a greater impact. With many thanks to the student and faculty team of Boone County’s Academic Detailing Project team, we and our partners are grateful to have learned so much over the past two years. An Interview with Lutricia Woods, RN OVERVIEW: Bell County, Kentucky was one of 4 original sites selected for years 1 + 2 of a pilot program of the CDC (Centers for Disease Control and Prevention), NACCHO (the National Association of County and City Health Officials), and our team at NaRCAD (The National Resource Center for Academic Detailing). This exciting pilot program focused on community-level work with local public health departments to develop customized interventions to reduce opioid overdose and death. Six sites experiencing significant public health problems related to opioids were selected over the two years to be trained in academic detailing; those trained health professionals then conducted 1:1 field visits with front line clinicians to impact behavior around prescribing, treatment referrals, and patient care, all within a rural area. As year 2 comes to a close, we’re showcasing stories from the field. Tags: Detailing Visits, LOOPR, Opioid Safety, Rural AD Programs, Substance Use  NaRCAD: Hi Lutricia, thanks so much for taking the time to speak with us about your work as an academic detailer for the opioid crisis in your community. Can you talk to us about how the opioid crisis has presented itself in Bell County, Kentucky? Lutricia: There’s not a family in this community that hasn’t been touched by the opioid crisis in some way. Twenty years ago, I worked in hospitals as an RN discharging patients and providing them with their prescriptions as they prepared to go home. At the time, I was shocked at the rates of prescriptions of opioids with benzodiazepines, and patients thinking it was safe. From my perspective, in our community, the opioid crisis really began by doctors beginning to prescribe many opioids to their patients without education or an understanding of the dangers. Three years ago, I was working on a project at a middle school, and was surprised by the number of grandparents that were raising their grandchildren because their children were either in jail, or otherwise affected by opioid use disorder [OUD]. In Bell County, we also have so many people unable to find a job because they cannot pass a drug test, and once that happens, they return to use because of the stressors of not being able to find a job and pay their bills, and it becomes a challenging cycle to overcome.  NaRCAD: Thanks for sharing your perspective, Lutricia—it can be true that some clinicians don’t see the impact of their role in prescribing opioids, and many times may believe that people who develop an opioid use disorder do so because of a moral failing, rather than seeing it as a medical issue. Did you think 1:1 outreach, provided directly to prescribing clinicians, would lend itself to improving patient health in response to the opioid crisis in this community? Lutricia: I desperately hoped it would. The opioid crisis is very personal to me, as it is to many people in our community. Years ago, my mom had 2 surgeries within 6 months. She had complications from one of those surgeries, and as a result, she was in the hospital for 6 weeks, during which time her care providers did not wean her off of the opioids she took immediately after the surgery. She returned home with prescriptions for opioids at a high dosage, and she developed opioid use disorder. My mother’s doctor, with whom I worked, reached out to have a conversation with me. He told me that I had to be the one to intervene with my mother because she continued requesting more opioids. I conveyed that I wanted her to discontinue taking them, and that he needed to assist us in finding a way to do this, as I felt his prescribing without discussing safety caused the initial issue. His response was that he wanted to “keep her happy.” My mother struggled for the rest of her life; she was able to completely wean off and discontinue using them, but it required a lot of counseling. As a result of this experience, I became a drug education coordinator, as I really wanted to do my part to mend the opioid crisis by providing drug education for every student in the county. And then, of course, I became an academic detailer for this project over the course of the past 2 years, which involves clinician education about safety and risk of opioid prescribing.  NaRCAD: Thank you for sharing that Lutricia; the opioid crisis is personal to so many of us. What would you say has been the most impactful piece of this academic detailing intervention as you went into the field and spoke with clinicians? Lutricia: The most impactful piece has been the ways in which we’re trying to hold clinicians accountable for their roles in the crisis, as well as leveraging their ability to improve things based on their relationships with their patients. For many of the doctors and nurses I met with, our conversations and educational resources have made them more thoughtful and intentional about their role. They seem to realize more that they have the power to decrease the number of prescriptions they write, the length of time for which they write them, and talk more with their patients about safety. NaRCAD: That’s fantastic. What about the most challenging part of this project—what’s been hardest about meeting with clinicians to talk about the opioid crisis in Bell County? Lutricia: Getting an appointment to go in and meet with these clinicians has been so frustrating and challenging. I always say that the receptionists in doctors’ offices are the most powerful people in the world. If you can’t get through them, you’re not going to get what you need, and it is the same with the patients. I couldn’t even get in to see my husband’s doctor, who we’ve known since we were kids. My husband had an appointment, so I resorted to going with him, and did a detailing visit on the spot with his doctor. This same doctor ended up changing practices, and it’s been a lot easier to get into that practice—all because of the office manager. Those relationships are important.  NaRCAD: Getting in the door is definitely a consistent challenge across many programs. We’ve heard from other detailers that practice makes perfect, and sometimes it’s easier to gain access when you actually show up and request a meeting in person. What else did you learn after being in the field? Lutricia: When I was “volun-told” that I would be attending a training, and doing “academic detailing”, I didn’t truly understand what it was or what the impact would be. I’m a big picture person, and I couldn’t see the big picture at all; I went into that training not knowing what to expect. It wasn’t until I actually started making visits that I could start to see the seeds we were planting to begin to have an impact. Share your thoughts on this piece in the comments section below, or learn more about the LOOPR project and other opioid safety academic detailing initiatives here and on our Detailing Directory. Guest Blog Interview: David O’Riordan, MPharm, MPH, PhD Senior Pharmacovigilance Officer Pharmaceutical Care Research Group University College Cork, Ireland Tags: Detailer Visits, International, Training  NaRCAD: Thanks for speaking with us, David! Tell us a bit about your professional background in healthcare, and how you became involved in academic detailing. David: I am a pharmacist by training, and a couple years ago I decided to carry out a PhD in Clinical Pharmacy at the University College Cork. As part of the PhD, I completed a systematic review examining how pharmacists can be utilized to optimize prescribing in primary care, including through academic detailing. After finding NaRCAD’s resources through a Google search, I registered for the NaRCAD conference in Boston. Dr. Fischer, Dr. Avorn, and all the other attendees at the conference were very encouraging. I left the conference determined and enthused to lead an academic detailing intervention back home. Dr. Avorn and Dr. Fisher put me in touch with Eimir Hurley, a PhD scholar in Ireland, who formerly worked in academic detailing at Alosa Health, and who ended up being a great help in executing the intervention.  NaRCAD: That’s terrific—it sounds like you had a great team at your disposal to begin this work. Can you tell us a little about the unique characteristics of the Irish health system? David: Ireland has a public and private health system. Public patients are more likely to wait longer for appointments. Private insurance is a substantial cost to individuals, though. The health care system is quite fractured unless you’re a private patient. Pharmaceutical drug representatives are also allowed to visit primary health practices here. NaRCAD: In April, you published a study titled “Pharmacist-led academic detailing intervention in primary care: a mixed methods feasibility study” in the International Journal of Clinical Pharmacy. Why did you choose urinary incontinence as a clinical topic? David: As this was a feasibility study, I decided to use one topic as part of the intervention. I organized a meeting with a group of general practitioners (physicians) who would be involved in the academic detailing intervention. The topic of urinary incontinence was chosen by the physicians because they highlighted that it was a topic not discussed regularly among themselves, and currently their only source of information is provided by pharmaceutical drug representatives.  NaRCAD: What barriers to success did you come across in your feasibility study? David: For this project, I was the only academic detailer. I started detailing after going to the two-day Basics Academic Detailing Training in Boston in May 2016. In some cases, during the roll out of the intervention I found it difficult to get past the practice manager, but luckily I had learned strategies on getting in the door in Boston that were useful in my effort. On a few occasions, the practice managers didn’t follow through on connecting me with the physicians. I got around this by utilizing physicians I knew in other practices to gain access to their practice. A lot of it came down to how well you know the physicians. I was lucky that they trusted me when I spoke to them. When I did get to meet with physicians, they all seemed very enthusiastic. NaRCAD: Can you talk a bit more about how receptive physicians were to academic detailing? David: Absolutely! This was a mixed methods study, so my colleague Eimir Hurley carried out focus groups after my detailing sessions to evaluate the feasibility of the intervention. Eimir conducted the focus groups on my behalf to reduce bias. The physicians liked that I wasn’t from a pharmaceutical company and that the sessions only lasted 10-15 minutes. They liked that local physicians had chosen the topic, and I wasn’t coming with my own agenda. NaRCAD: How are you or others going to use your feasibility study results to implement across the country? David: I am currently not involved in academic detailing, but I hope to be again in the future. If someone from another part of Ireland read my paper, they would recognize that physicians are very willing to take part in academic detailing. From my experience physicians didn’t feel threatened and really enjoyed the interaction. They liked the interactive style of the visits, and the way that that the evidence was delivered. My study provides a platform for other researchers to detail to a wider group of physicians in Ireland. NaRCAD: Anything else? David: I am very grateful for the NaRCAD team for providing the academic detailing training. I knew literally nothing about academic detailing, and through meeting their team members Sarah Ball, Amanda Kennedy, Mary Liz Doyle-Tadduni, and others, I felt encouraged to go back and detail. I was the only person from Ireland at the training, and the NaRCAD team gave me some useful feedback. I really enjoyed academic detailing, and I was especially proud when my paper was published. I discovered there is an appetite for this educational intervention in Ireland.  Biography David O’Riordan, MPharm, MPH, PhD Senior Pharmacovigilance Officer Pharmaceutical Care Research Group University College Cork, Ireland David holds a Masters in Pharmacy (MPharm), Masters in Public Health (MPH), Post Graduate Certificate in Teaching and Learning in Higher Education (PG Cert) and a PhD in Clinical Pharmacy. He has extensive experience as a community pharmacist. He previously worked as a Lecturer in Clinical Pharmacy in University College Cork (UCC). While there, he contributed to and assisted in the delivery of research-led teaching at undergraduate and postgraduate level. He also supervised on a number of research projects. He was a clinical trials pharmacist involved in the Thyroid Hormone Replacement for Subclinical Hypo-Thyroidism Trial (TRUST). This was a randomised placebo controlled clinical trial comparing levothyroxine to placebo in community dwelling older adults (≥65 years) with subclinical hypothyroidism (SCH). He is also a tutor on the Irish Pharmacy Union (IPU) Academy. This educational initiative was developed by the IPU to support pharmacist engagement with Continuous Professional Development (CPD). He is currently the Senior Pharmacovigilance Officer at the HRB-Clinical Research Facility, UCC.  Tags: Detailing Visits, Stigma As we reflect on the two major public health topics we’ve been focusing on as we’ve traveled to public health departments across the United States, we’re learning that the public health detailers we’ve been training are discussing much more than just evidence with the clinicians they’re meeting. When we train new health educators on the methods of interactive, 1:1 education, we’re asked most often to customize our curriculum to cover two of the most highly stigmatized topics today: the opioid crisis, and HIV prevention. As the topic of stigma has come up at every straining we’ve implemented this year, our training team has added dedicated time to our trainings to discuss ways to address clinician stigma that arises during 1:1 detailing visits. So, what, exactly, is stigma? It’s defined as “a mark of shame or discredit,” and appears in numerous ways, including through labeling, stereotyping, discrimination, and social inclusion. One of the biggest myths about stigma is that some people carry it, and some people don’t. However, stigma is not binary, and we all possess the ability to stigmatize another group that we perceive to be an ‘outsider’ group. Historically, stigma has appeared mainly in the form of social inclusion, with those identified as ‘others’ being treated as societal outcasts. The interactive approach of AD is well-suited to address clinician stigma by creating a space in which the detailer can ask the kinds of needs assessment questions that can identify the source of these stigmatizing perspectives. When a 1:1 visit is facilitated by a skilled clinical outreach educator who is curious about clinicians’ experiences and genuinely wants to help implement sustainable change, many clinicians feel comfortable in sharing beliefs, identifying patterns, and building relationships based on trust and service. Our language and beliefs will continue to evolve as we continue to learn, encourage one another, and be empathic. We can do this by holding each other accountable in a non-punitive way, pairing our best intentions with education to use inclusive, supportive language, and committing to holding one another accountable by identifying moments when we witness stigma, in order to correct, reflect, and move forward. We’ve seen the potential for change; the medical community’s understanding of substance use disorder and HIV prevention has improved significantly over the past few decades. Outside of our training settings, where else can we start? We’d very much like to hear from you, our community members, about how you’ve experienced or witnessed stigmatizing behavior as it has occurred within the healthcare setting. If you’re an outreach educator, tell us about a time you’ve seen stigma arise from a clinician’s perspective, and what you thought was behind it. If you’re a patient or a provider, talk to us about ways in which you’ve experienced or carried stigma. Keeping a dialogue open and encouraging sharing is one of many steps towards a connected medical community that embraces its patients, clinicians, educators, and supporters with compassion, clarity, and support.
Thanks for reading, and please share your thoughts and experiences in the comments section below! The NaRCAD Team Building a Team to Improve Local Vaccination Rates: Strategies to get your "Foot in the Door”5/2/2019 Featuring: Kimberly C. McKeirnan, PharmD, BCACP Director of the Center for Pharmacy Practice Research, Washington State University College of Pharmacy and Pharmaceutical Sciences Tags: Detailing Visits, Program Management, Vaccinations  As a pharmacist, I spend a lot of time teaching. I teach patients how to take their medications, how to choose over-the-counter products, and how to identify whether or not to treat minor ailments at home, in the pharmacy, or by seeking care from a physician. I also get to teach other health care providers when one of the medications they prescribe to a patient will interact with the patient’s other medications or cause side effects that will be problematic. After teaching informally in the pharmacy since 2005 and more formally as a Clinical Assistant Professor for the College of Pharmacy and Pharmaceutical Sciences at Washington State University since 2013, my transition to become an academic detailer was natural.  In 2014 I teamed up with an interprofessional group of colleagues to apply for grant funding to improve the low pneumococcal immunization rates in our local rural areas. Our project proposed utilizing academic detailing to teach healthcare providers about pneumococcal immunizations and the importance of immunizing patients. The CDC Advisory Committee on Immunization Practices (ACIP) released a recommendation to vaccinate all patients 65 and older with the new PCV-13 pneumonia vaccine in combination with the longstanding PPSV23 vaccine as part of a two-dose series. Having two pneumococcal vaccines with a complicated vaccination schedule has been challenging for providers. I often hear the questions from my colleagues: “Why are there two, do we really need two?”, “Which one do I give first?”, “When do I give the second one?”, and “What if I give them too close together, do they still work?” Additionally, during a needs assessment of our area we found that many rural pharmacies in our area do not vaccinate at all or only stock certain vaccines because they don’t want to cause competition with the local physicians. We were successfully funded with an Independent Grant for Pfizer’s Learning and Change from Pfizer in 2015. During the first phase of the project, we attended the NaRCAD training program in 2015. The NaRCAD training provided a solid foundation for the framework of our project.  However, once we started talking to local providers about coming in to provide academic detailing, we ran into a major barrier. Getting our “foot in the door” with local providers was harder than we expected. It became clear that our team would need to expand to include more healthcare providers and that we would need to focus our efforts on convincing local medical clinics and pharmacies to invite us in to detail their teams. We expanded our team to include two pharmacists, one nurse, two physicians, two student pharmacists, one student nurse, two medical students, and on biomedical data analysis student. Our team physicians were able to identify physician champions and convince local medical practitioners that our detailing would be helpful for the medical team. They conveyed the message that we weren’t trying to rearrange things – just offer support the clinics. Four pharmacies and two medical clinics invited us to provide detailing.  For the medical clinic visits, we were able to give 15-minute presentations during staff meetings at each location. Attendees included hospital administrators, practitioners, pharmacy staff, nurses, medical assistants, and front end office staff. We appreciated the opportunity to reach so many disciplines at once since immunizations can be recommended by several different health disciplines and at several points during an office visit or hospitalization. Our detailing visits were so well received that we were asked to come back to one of the medical clinics to provide a more in-depth educational program to all of the nursing staff. The second clinic invited us back to meet with hospital leadership to discuss specific points where interventions could be implemented, such as using an EHR alert, putting up signs, or simply asking patients if they were interested in receiving an immunization. We identified several clinical pearls for teams that are considering getting into academic detailing:
McKeirnan KC, Colorafi KJ, Panther SG, Potyk D, McCarthy J. Teaching the Healthcare Team about Pneumococcal Vaccination Practices for Older Adults through Academic Detailing. The Senior Care Pharmacist. Accepted March 2019, in press.  Biography Kimberly C. McKeirnan, PharmD, BCACP Director, Center for Pharmacy Practice Research, Washington State University College of Pharmacy and Pharmaceutical Sciences Kimberly C. McKeirnan, PharmD, BCACP, is a Clinical Assistant Professor in the Department of Pharmacotherapy at the Washington State University College of Pharmacy and Pharmaceutical Sciences. Dr. McKeirnan graduated with her Doctor of Pharmacy degree from WSU in 2008 and joined the faculty at WSU in 2013 after five years in community pharmacy practice. She is the Director of the newly developed Center for Pharmacy Practice Research at WSU and enjoys teaching student pharmacists about patient care and research. Dr. McKeirnan is passionate about research involving community pharmacy, public health, and improving patient access to quality care services. Dr. McKeirnan has received grants for improving immunization rates in rural areas, developing a model for implementing chronic disease-state management services in rural community pharmacies, and developing a pharmacy technician immunization training program. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|

