|
Curated By: Aanchal Gupta, Program Coordinator, NaRCAD Tags: ADvice, Program Management, Training Academic detailing program managers oversee and coordinate all aspects of an AD program to ensure its success, impact, and strengthen the detailing team. They have a crucial role in achieving team goals. In this edition of AD-vice, we’ll look into how program management in AD contributes to team and program success.  Team Building and Support:
 Recruitment and Training:
 Interprofessional Collaboration:
Effective program management plays a crucial role in the success and support of academic detailing programs. We hope the insights shared in this edition of AD-vice will help in navigating and implementing strategies of team building, recruitment, training, and more. As always, our NaRCAD team is here to support you and your detailing programs! Best, The NaRCAD Team Have thoughts on our DETAILS Blog posts?
You can head on over to our Discussion Forum to continue the conversation! An interview with Nicole Green, BSP, RPh, ACPR, DPLA, Director of the Ambulatory Pharmacy Services Program at ThedaCare, a healthcare organization based in northeastern and central Wisconsin serving both rural and urban areas. By: Aanchal Gupta, Program Coordinator, NaRCAD Tags: Program Management, Detailing Visits, Opioid Safety  Aanchal: Hi Nicole, thank you so much for talking about your program with us today! You’re a pharmacy director at ThedaCare—tell us more about the academic detailing component of your programming. Nicole: During the past four years working at ThedaCare, I’ve been studying ways in which pharmacists could serve as academic detailers to support opioid stewardship initiatives in order to positively influence prescribing. I was able to collaborate with other physician leaders as well as executive leadership who supported the program, gather data on opioid prescribing, and work on a proposal for academic detailing. We created our first formalized detailing project, called the Ambulatory Pharmacy Services Program, in January 2021. We had four detailers kick off our program and we’ve now doubled our team with a total of eight detailers that have all been trained by NaRCAD. Our detailers are ambulatory pharmacists who are embedded in ThedaCare’s family medicine and internal medicine clinics, serving as both medication experts and pharmacy consultants for patients and providers.  Aanchal: It’s incredible how quickly your program grew! Can you tell us more about the areas you’ve been focusing on for academic detailing? Nicole: Opioid stewardship is our main focus area for our detailing initiative. Our detailers identify patients who are candidates for Naloxone and work with clinicians to provide education to patients and their family members. The detailers also assess patients who have been on opioids for a long time and determine if they still need to be on them or if tapering should be considered. The second focus area is comprehensive medication management services for our self-insured population. This includes having our detailers identify chronic disease management gaps and partner with our state employees to optimize care for patients to reduce cost and readmissions. Our last focus area is to support our new heart failure clinic. Patients are referred to this clinic if they’ve been discharged from the hospital with heart failure or if they’ve been referred by a cardiologist. On initial visits, patients see a cardiology provider followed by an ambulatory pharmacist. Our role is to review the patient’s chart and provide recommendations to the team, as well as education to the patients. Our goals are to decrease readmissions and improve guideline-directed medical therapy.  Aanchal: Wow - your team’s impact is tremendous. You previously mentioned that you were able to double your detailing team in less than a year. What characteristics do you believe are needed to have a strong detailing team? Nicole: Having in-depth knowledge about the clinical topic is extremely important. Detailing is also about building trust and strengthening the relationship with confidence. Detailers need to be confident, especially when they’re first starting out and are meeting with providers that they have yet to build a relationship with. Detailers also need to be prepared to respond confidently and in a way that will still engage the providers in an open conversation. Providers typically don't understand that ambulatory pharmacists’ jobs are to assist patients to meet medication-related goals. There have been assumptions about why we’re delivering this service or why we’re meeting with clinicians. Clinicians ask questions such as, “Is it because I’m being targeted?” or “Is it because of my prescribing practices?”  Aanchal: Agreed; at NaRCAD, we know that having both clinical expertise and confidence communicating is essential to detail successfully. We know what makes a successful detailer – now let’s talk about what qualities you believe make you successful as a leader. Nicole: The first quality that comes to mind is passion. I lead with energy and show my team how exciting this work can be. I think that's important because previously we didn’t have pharmacists embedded in primary care and patients didn’t have an option to book an appointment with a pharmacist for consultation. Our pharmacists are delivering a service that was not there before. They need to promote themselves and make others aware of how they can help. Also, I like to be a strong advocate for my team. I constantly raise my hand saying that we can help with different initiatives or that certain projects are right up our alley.
Finally, I encourage my team to be persistent. We can't take the first “no” from a clinician as rejection. It might mean, “not now,” “I don't understand,” or “I haven't been exposed to this.” It doesn’t mean that they never want to have a visit with an academic detailer or will never change their prescribing behavior. Aanchal: These are all core elements in building a strong team. Some situations can feel defeating and having a strong leader that has your back is so important. Lastly, what advice do you have for someone who is new to managing a team of detailers? Nicole: Prepare your detailers for the field with the most up-to-date clinical content so that they can interact with clinicians confidently. Also, provide your detailers with training opportunities and use resources like NaRCAD. If you have the capacity, take it one step further by adding practice role play sessions among peers and allow new detailers to observe other detailers in the field. When training, help the detailers step out of their comfort zone within a group of people that they know before they step out of their comfort zone with a stranger. Aanchal: Yes, having support and receiving feedback from peers is an important element of building a strong team. Thank you so much for sharing your perspectives with us, Nicole! We look forward to continuing to see your team grow and feature your work at our upcoming conference! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  BIOGRAPHY: Nicole Green completed her pharmacy education at the University of Saskatchewan, Canada followed by a hospital residency. She practiced for over a decade as a Clinical Coordinator primarily in the area of cardiology. She has completed year-long learnings through the AIMM (Alliance for Integrate Medication Management) collaborative as well as the ASHP PLA (Pharmacy Leadership Academy). She is the Director of Ambulatory Pharmacy with ThedaCare. She leads the comprehensive strategic plan to embed pharmacists within family and internal medicine clinics as providers and vital members of the primary care clinical team. She has served as an Executive panelist with GTMRx (Get the Medications Right) and the Institute for Advancing Health Value. Her program utilizes Academic Detailing as a means of building professional relationships, establishing credibility and influencing prescribing improvements. Much of her team’s work is related to Quality improvement initiatives in medication stewardship and safety as well as maximal performance in Pharmacy related ACO measures. Nicole has worked with the ThedaCare cardiology team to build a collaborative Heart Failure Clinic where patients see both a cardiology provider and am ambulatory pharmacist. An interview with Carla Mena, Capacity Building Manager at Hands United of the Latino Commission on AIDS. by Aanchal Gupta, NaRCAD Program Coordinator Tags: HIV/AIDS, Training, Program Management  Aanchal: Hi Carla, thank you so much for joining us today! We’re excited to delve into Capacity Building Assistance (CBA), as well as feature Hands United of the Latino Commission on AIDS on our blog. How did you get started in this line of work, and could you describe your current role as a capacity building manager? Carla: I worked at a Duke University hospital in North Carolina for 7 years as a bilingual research coordinator in both local and global studies. I have research experience in hepatitis C, HIV, immigration, LGBTQ+, childhood obesity prevention, neonatal vaccinations, reproductive health, and the intersection of these areas. I also did some leadership development work, as well as community organizing. I had the opportunity to connect with teams and individuals on how to work with underserved populations, and taught them about social determinants of health, cultural humility, and health equity. At Hands United, I began as a capacity building specialist, and have now transitioned to a capacity building manager. I make sure that we’re thinking within our funding guidelines while also highlighting the intersections of folks living with HIV or who may be at risk of acquiring or transmitting HIV. As a manager, there's the administrative side of supervision, following up on tasks, and so on. The other aspect of it is to continue to provide technical assistance (TA) to our jurisdictions. For example, if someone is interested in implementing an HIV self-testing program in a non-clinical setting, I can assist with that. I enjoy the fact that, although I'm not a specialist anymore, I still provide TA with the team. Both of our directors also provide TA, which I think is unique.  Aanchal: Wow, you have such an extensive background in public health and sounds like it has informed your current work! Tell us more about the Hands United program as well as the importance of capacity building assistance. Carla: The Hands United of the Latino Commission on AIDS is a capacity building technical assistance program (CBA). The CHANGE (customized, holistic, analytical, network-building, grassroots, evaluatory) model is an approach developed by the Latino Commission on AIDS. Hands United is one of the two programs available. It combines community-based organizations, health departments, or any other social service organizations to optimally plan, integrate, implement, and sustain prevention programming and services. CBA improves the performance of the HIV prevention workforce by building individual-level competencies and technical expertise while also strengthening organizational capacities. We serve 19 jurisdictions in the southern region of the United States including, Arkansas, Alabama, Delaware, D.C., Florida, Georgia, Kentucky, Maryland, Louisiana, Mississippi, North Carolina, South Carolina, Oklahoma, Tennessee, Texas, Virginia, and West Virginia. An organization will contact us about various topics related to HIV prevention such as recruitment for HIV testing, referrals for HIV medical care, referrals for PrEP, nPrEP, STIs, hepatitis C, or TB screening. Our role is to help them figure out what resources they need. Then we can support them with webinars or resources such as literature reviews, marketing samples, and successful stories.  Aanchal: Thanks for providing some context on the program and intervention. It’s always great to know that there are resources like this out there for organizations to utilize. Could you describe how CBA relates to academic detailing? Carla: Detailing is very fundamental for the work that we're doing because it teaches effective social and personable skills that organizations can take out in the field. Sometimes health departments reach out to us and say that they are not sure how to recruit for providers to refer or prescribe PrEP in primary care settings. These are times when we discuss academic detailing and how it can be useful for them. Although we’re not detailing, we’re able to provide information in a way that makes sense to those who need it. We ask them questions to better understand their program and help programs figure out exactly what they need. We ask questions like, “What is part of your package?” “What are the questions you're asking clinicians?” “What is your elevator pitch?” “Is there capacity and effort from the staff?” We might even say, “You need detailing, but you don’t have enough staff to be able to detail all the primary care providers in your county.” When this happens, we provide assistance on developing a recruitment plan that’s feasible for the requestor.  Aanchal: Those are all important questions for programs to consider as they brainstorm what it is that they need. Is there something that your program was able to accomplish during this past year that you’re proud of? Carla: We were able to work with your team at NaRCAD and host a training this past July. This was a highlight for us because we were able to have a good representation and engagement from the jurisdictions. A community was created through the participation of the trainees. We gained a lot of knowledge that we needed in order to provide TA or CBA services to our programs. Aanchal: That’s so nice to hear! Speaking of the training, I’d love to hear about your experience, particularly as you’re someone who was not planning to be a detailer. Carla: For me, it was a great training because all the training facilitators were so welcoming of feedback and even role played to include our specific experiences. They took time to understand our roles and built a sense of community. Additionally, it was very hands-on, and I enjoyed having the opportunity to role play a detailing visit. Walking in the detailer’s shoes helped me understand exactly what could be happening to them during a visit or where they may be challenged. Fusing my own lens with the lens of the detailer was very helpful.  Aanchal: I agree -- the trainings provide a practical space for trainees to share their unique experiences while practicing the communications techniques necessary to carry out a 1:1 detailing visit. Is there any advice you would give to someone who may be hesitant about attending an academic detailing training if they ‘re planning to be a program manager rather than a detailer? Carla: I would say, go for it! Although we may not be detailers, being able to walk through what a detailer does has made me a better CBA specialist and manager because I understand the processes through the eyes of the detailer. Watching webinars or reading resources on academic detailing was helpful and effective, but attending a training gave the opportunity to put it all into practice. Aanchal: That is great advice! Thank you so much, Carla, for speaking with us and it was a pleasure having you at our training. We look forward to working together in the future. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography: Carla is the Capacity Building Assistance Manager for Hands United at the Latino Commission on AIDS. Prior to joining the Hands United at the Latino Commission on AIDS team, Carla worked at Duke University Hospital, as a bilingual research coordinator working with studies that were both local and global. Carla has extensive research experience in several fields including hepatitis C, HIV, immigration, LGBTQ+, childhood obesity prevention, neonatal vaccinations, and sexual and reproductive health. In addition, she has experience training people and partnerships on how to work with under-represented and under-served populations in the US. Some of those trainings include exploring social determinants of health, cultural humility, and health equity. She graduated from Meredith College with a BS in biology. Carla is a certified Culture Facilitator, Diversity to Belonging Facilitator and Culture Assessor. Overview: Loren Regier, a NaRCAD Expert Training Facilitator, joins us to reflect on nearly 25 years of his AD career, his experiences in learning AD for the first time, and his role in being a mentor to a new generation of academic detailers. Loren is a hospital pharmacist by training and has served with the RxFiles Academic Detailing Program and the Centre for Effective Practice, both longstanding Canadian AD programs. by Winnie Ho, Program Coordinator Tags: Detailing Visits, International, Program Management, Sustainability, Training  Winnie: We’re delighted to hear more about your AD journey, especially about the ways in which you continue to be a leader and supporter of the AD journeys of many others. Can you tell us a little bit about how you got started in this field? Loren: I was a hospital pharmacist doing a lot of work related to clinical decision-making, public speaking, and education. The Director for our Saskatoon Health Region (SK, Canada) had come across academic detailing from a colleague in Vancouver, and was interested in piloting something similar to what is now the British Columbia Provincial AD (BC PAD) Service. Our region needed someone who would take on this project and build something from scratch. Only partly knowing what I was in for, I said “yes”. To train and learn more, I had the chance to shadow Terryn Naumann in June of 1997. Terryn was the pioneering solo detailer in North/West Vancouver. What was initially a 1-year project for us, became a 2-year, and then a 3-year project, eventually morphing into an ongoing AD service that expanded to cover our province of Saskatchewan.  W: That’s incredibly fortuitous that you had Terryn to turn to for help! We’ve gotten to interview her before at DETAILS and know that she was a trailblazer for AD across Canada. Before I ask you about your experiences now as a mentor to others, I would love your reflections on your experiences as a mentee back in the days when you were learning AD as a new trainee with Terryn as your guide. L: There are both good days and difficult days to think back to – it involved a lot of hard work, but I was fortunate to have an awesome mandate and the opportunity to see another successful service in operation. Most importantly, I was able to see what a successful visit looked like. I joined Terryn for 7 visits over 2 days. After each visit, we reflected on how the visit went, what we liked, and if there was anything one might handle differently. The opportunity to shadow Terryn instilled in me the vision that academic detailing was about both relationship and service, and that clinicians could find both aspects valuable and enjoyable.  W: We do encourage a lot of new people starting AD for the first time to try and find someone to tag along with. You were especially lucky with Terryn because she had had a few years to build up her network and relationships in her community. L: Relationships are key in AD – and witnessing those relationships and the resulting AD conversations – was educational and inspiring. W: Is there a particularly strong piece of advice or a mentorship experience that sticks with you to this day? L: One of the things I recall is that she said, “One day, when you have a tough visit, I want you to call me, because I’m one of the only people who will understand what you’re going through.” Well, the day came when I had to call Terryn and we were able to debrief on a challenge I had faced. That was a critical moment that served to propel me forward with greater insight and confidence.  W: You bring up something important – our work is focused on creating safe learning spaces for providers in order to enact change. What we’ve been able to expand on are the connections between individual members of the detailing community. Luckily, the field has grown and new detailers have many more role models and teachers to learn from. Let’s also talk about this vulnerable moment, because it requires a lot of trust to go to someone when something goes wrong.  L: The mentorship process ideally involves deep, authentic discussions about being a detailer. Being a detailer involves constantly putting your best self forward. Trust allowed both of us to open up to each other with lots of safe space to discuss our different approaches and experiences. Trust is essential for effectively exploring differences of opinion, and how to turn challenges into opportunities. Without it, you don’t get to understand where someone is coming from or to truly grow and learn. In addition, I need to mention Frank May who also became valued mentor over the years. Frank helped pioneer academic detailing in Australia. His thoughtful conversations and leadership were instrumental in my growth in AD, as well as my eventual role in helping train and mentor new detailers.  W: I have definitely seen the large and small ways that mentorship has propagated through the AD community. In the process of learning and educating others in this field, we never truly stop being mentors or mentees – it’s not a binary. It’s a great lifelong process. Let’s flash forward to now: given your experiences, how have you continued to integrate mentorship into your current work? L: A big part of my role these days has been training, mentoring, and supporting others - both academic detailers and those who are moving into program leadership. It’s important to recognize that the world needs more people to do this kind of work and that we need to pass the baton. That involves coming alongside their journey, having good discussions, and being able to dig deep into those critical ingredients for success.  It has meant being transparent about my decisions and leadership so that my team can not only see how I’m thinking and processing things, but also provide their own input and ideas. Being a mentor to me means modeling the approach of learning together and working enthusiastically and collaboratively when pursuing opportunities. W: You’re in a capacity now where you’re training future leaders in AD. You provide an important link and opportunity to reflect on where AD has been, but also the space to give new AD folks a chance to figure out where AD may go next. The people you mentor now will likely go on to mentor others, just as Terryn and Frank did for you. What advice would you give to those who are seeking to be strong mentors?  L: People can sense if they are respected and valued. If they know you care and are interested in their growth, they will open up, share the important stuff, and work together to address the challenges of academic detailing. If you add some fun and enjoyment along the way, the process serves as a model of what will eventually happen between the detailer and those they detail. W: That’s wonderful advice, because one of the best things you can do for someone who is learning is to fully believe in their potential and strengths. They’re already a part of your team – they’re there for a reason.  L: Somebody once asked the coach for Bobby Orr, one of the greatest Canadian Hockey players of all time, “How do you coach Bobby Orr?” and the reply was, “You don’t coach Bobby Orr, you give him room to play the game.” There’s some truth in applying that to leadership and in AD. You need to appreciate where your team members excel and empower them. It means coming alongside, supporting their input, and also giving them the freedom to make their own mistakes and learn from them. Give people the support they need to do best. They’ll show you what they’re capable of. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  LoLoren Regier is a Pharmacist and Consultant Editor with RxFiles Academic Detailing Service in Saskatoon, SK, Canada. Loren has guided the development of this provincial academic detailing service since the first “ground breaking” pilot project began in 1997. Loren is active as a member of the Canadian Academic Detailing Collaboration and provides training and consultation to various programs and initiatives. Loren’s interests cover the practical application of evidence to practice and the ongoing development of multifaceted interventions that support academic detailing. Additionally, Loren serves as a faculty facilitator for NaRCAD’s Academic Detailing Techniques trainings. Loren is co-editor of the RxFiles Drug Comparison Charts – 10th Edition and a contributor/reviewer for Geri-RxFiles and the RxFiles – Bringing Evidence to Practicesection of Canadian Family Physician journal. Loren obtained his degree from the University of Saskatchewan, College of Pharmacy in 1988 which he followed with a hospital pharmacy residency. He serves as a lecturer, instructor and preceptor in the areas of evidence informed drug therapy decision making, educational outreach and chronic pain management in a wide variety of professional settings Overview: Harald Langaas speaks with NaRCAD about his experiences in co-founding Norway’s first national AD program, KUPP. KUPP, which loosely stands for “Knowledge-Based Updating Visits” in Norwegian, has been actively serving Norwegian General Practitioners (GPs) for several years. by: Winnie Ho, Program Coordinator Tags: Chronic Illness, Detailing Visits, Evaluation, International, Program Management  Winnie: Hi Harald, thank you for joining us all the way from Norway to talk about KUPP, the Norwegian Academic Detailing program! Can you tell us a little bit more about yourself and the work that KUPP does? Harald: I’m a pharmacist by training, with experience in working at hospital pharmacies and as a pharmacy manager in the private sector. My interest has always been in how to better provide independent information about the use of medicines to healthcare professionals to improve the quality of healthcare. I work for one of the four Regional Medicines Informational Centers in Norway, one for each of the four health regions. The Norwegian AD Program is strongly connected with those Centers, so my position is split between the regional center and as Director of KUPP, which operates at the national level. KUPP is a small organization – it’s myself and a consultant in clinical pharmacology handling the administration of AD.  W: I can absolutely see why AD fits a lot of your interests! Let’s talk about how KUPP got its start. You were part of the founding of a brand new AD program. What was that like, and what did you learn? H: My colleague Roar Dyrkorn had visited Australia, met the NaRCAD team in Boston, and was very inspired by AD. He saw it as an opportunity to improve the quality of prescribing in primary care and began lobbying to acquire funding for an AD program. Our first campaign in 2015 was put together within a month or two, focusing on NSAIDs (Non-steroidal anti-inflammatory drugs) for GPs. We were extremely fortunate to have Debra Rowett from Australia, who has been pioneering AD in Adelaide for many years, fly out to train our first detailers because we were still novices to this work. This campaign went quickly – maybe too quickly -- but we were able to implement it well, and we had success with the campaign. We’ve been continuing to detail ever since.  W: You also mentioned that Norway is divided into four health regions. Can you tell us a little bit more about these regions and the communities that you serve in each? H: The four jurisdictions, all funded and overseen by the government, are responsible for hospital services in that region. However, primary care services are overseen at the national level. In each region, KUPP has between 5-10 people that are trained as detailers and conduct visits in addition to working at the Regional Medicines Information Centers or at a Clinical Pharmacology department at a hospital. W: On average, how many clinicians does KUPP work with per year? H: There are about 5,000 total GPs in Norway, and we visit between 1,000-1,200 GPs a year, which is about 20%. We have limited resources while trying to reach as many providers as we can nationally. For the funding we have, we’re happy with our work, but of course, we are ambitious! We want to be able to visit everybody.  W: That’s a pretty sizable population that you reach, especially on limited resources! Can you provide some context about Norway’s healthcare system that help us better understand the context in which KUPP operates? H: In Norway, we have universal healthcare, which is fully funded by the government. It means that our healthcare system is quite homogenous across the country. The GPs that we focus on are mostly self-employed, but fully funded by the government. This does mean that when we make arrangements to schedule detailing visits, we have to contact GPs one at a time. They have no financial incentive to see us, and since we take up their time instead of them seeing a patient, they actually lose money by seeing us. This means that we have to ensure that a visit from us is useful and that it’s a valuable investment towards improving the treatment of their patients. We keep all visits to 30 minutes or less. Another important thing to mention is that patients are designated to their GPs. You can’t shop around for providers, so you have to see the same one each time or apply to change to another one. This means that a GP follows their patients for a long period of time, and have a lot of history with their patients.  W: That’s useful background information to know about. Since patients often stay with the same and only GP, how does that impact a GP’s insight into their patient population? H: Because of the long shared history, it means that when we are talking with clinicians, they know their patient pool very well. Even when a GP has taken over a practice, they will be very knowledgeable about who they are serving. W: I imagine that when detailing on chronic conditions, this is an advantage because a GP and a detailer can follow a patient population over time and offer continuous support! Now, we’ve been able to follow KUPP’s work for a while, especially with a lot of your recent presentations and research. How are things going with research and evaluation lately? H: It’s always been useful for us to evaluate and publish our results, especially when we approach the government for more funding. While we can’t do every campaign as a research project, I’ve been working on evaluating a campaign we did on diabetes and also a study on the impact of group visits vs. 1:1 detailing. We’re also working on a small qualitative evaluation of our virtual visits at the moment. It’s been exciting to be contacted by other research groups who want to work with us. It’s really inspiring for us to know there are groups who want to learn more about AD because of us, and that we’re being noticed and seen as a good research partner.  W: It’s always exciting to see where AD travels and how many borders it can cross. We always learn more because the AD community is constantly growing and innovating. As someone who has been at the forefront of establishing AD abroad, what are your hopes for the international AD community at large? H: I would sure hope to see more AD programs emerging in Europe. It would be very helpful to fully connect the AD initiatives that are ongoing around us, to build the same kind of network that North America has had between the United States and Canada. W: We hope to see more programs emerge too! Last question – any final words of advice for detailers and programs? H: The main advice would be to not give up. There will be resistance, and you will run into some troubles, but keep on working. If you believe in the method, and you believe in the work you do, it will pay off. The 1:1 approach is something that separates AD from other tactics, and makes it easier for both clinicians and funding organizations to see you as unique. This work is worth it. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Harald Langaas has been the director of a hospital-based medicines information centre (RELIS) in Trondheim, Norway since 2013. Together with colleagues at St. Olavs Hospital he started the first academic detailing program in Norway in 2015, and has been involved in AD work both as administrator and active detailer since then. Since 2018 he has been the director for KUPP – The Norwegian Academic Detailing Program. He is currently working on a PhD based on evaluation of academic detailing. Overview: Mary Moody joins us from the University of Illinois at Chicago (UIC) College of Pharmacy to discuss the passing of an 2019 act providing AD to Medicaid prescribers in Illinois state, and how AD programs with similar legislative aspirations can follow in UIC's footsteps in securing support and funding for their work. Written by: Winnie Ho, Program Coordinator Tags: CME, COVID-19, Health Policy, Opioid Safety, Program Management  Winnie: We’re very excited to have the opportunity to discuss with you regarding the efforts behind the passing of legislation in Illinois that helped cement the provision of AD services to Medicaid prescribers across the state! But before we get deeper into that, can you tell us a little bit more about yourself and your AD-related work? Mary: I’m an Associate Dean for Professional and Governmental Affairs at the UIC College of Pharmacy, in addition to a Clinical Associate Professor. I started in Drug Information and for years, was managing our Drug Information Center which supports healthcare professionals around the country. We’ve been working with the state for some time now, supporting the Medicaid prescriber population with the prior approval process. Within that timeframe, we started to look into AD to get a better understanding of how we could implement this for our providers.  W: That’s a background that certainly lends itself to promoting AD. Can you walk us through what this legislative act details? M: The bill outlines the development of a program to provide AD to Medicaid prescribing physicians. The bill also includes two specific components – one of which was an agreement to provide free CME which is available on our website, and the second of which was establishing a toll-free drug information phone number and e-mail for providers to reach out to us after their visit. We have trained drug information specialists who can answer any questions they have about medications. W: It’s important that this act received approval and support from the Illinois General Assembly. Can you talk to us about how this bill came to the floor and how it came to pass?  M: One of our legislators – Representative Theresa Mah – had attended the 2018 National Conference of State Legislators, which is an organization that acts as a percolator for new ideas about new laws. There, she learned about AD as there have been similar legislative acts established in other states, such as New York. She became really interested in bringing something similar to Illinois. In my role with Professional and Governmental Affairs, my responsibility is to keep track of proposed bills that are in the hopper, and when I saw that this bill was coming up, I was like wait, this is perfect! I set up a meeting with the representative to describe the vision and plans we had at UIC College of Pharmacy.  At this point, UIC had completed a pilot with AMITA Health to look at the benefits of AD in opioid prescribing through a CDC grant. Because of this prior experience, we were recommended to the state as a partner for this initiative. Eventually, Dr. Todd Lee and I were invited to present in front of the state House and Senate committees where we introduced AD and answered any questions the representatives had. It was ultimately passed through House and Senate unanimously. I felt pretty great about that.  W: I’m glad to hear that the legislators really prioritized this. For the world of AD, this is a major win, especially as other AD programs may be interested in replicating your success on the legislative floor. M: The legislative route is incredibly useful because it helps give me a higher level of comfort knowing that my budgeting for our AD work is likely to come on an annual basis. W: I’m curious about how you were able to introduce AD to a brand new audience and persuade all of them that this work was something they ought to prioritize.  M: Since there have been several places that have established the legislation including New York, North Carolina, Pennsylvania, Maine, Massachusetts, Vermont, and Washington D.C, we were able to establish that there was precedent and could show them previous models. We were able to demonstrate how this would benefit Illinois, especially in reaching our targets of improving prescribing, reducing emergency room visits, and reducing hospitalizations for our chronically ill. We discussed how there were a large number of individuals in our state who were Medicaid recipients that suffer from multiple chronic conditions, and that it was difficult for our prescribers to stay up to date with so much information coming at them. We wanted to provide the best evidence-based, non-biased information.  W: Your program kicked-off your work by focusing on the opioid overdose crisis. How was this chosen as a starting point? M: It’s a public health crisis that is an absolute priority in Illinois. UIC has been working on research in academic detailing and the impact on opioid prescribing. We could match our pitch for AD to this current issue, it helped our presentation to the committees a lot. W: When it comes to legislation, sometimes it can require many things to align. In this case, we’re trying to align healthcare interests, research, and the policy decision-making process. There’s always a lot of competing interests and AD is certainly not the only tool in the toolkit towards improving patient outcomes.  M: For anyone looking to intertwine AD with their state legislative process, you need to understand what your state’s priorities are. You can start by looking at state plans and guidelines for major health issues, just like the opioid crisis. No one is against making these health issues better for everyone, but you may need to do more research to understand where your program fits in and more importantly, who the movers and shakers in your governance are. W: Right, these connections are critical to building support. M: One of the things that can be frustrating is not knowing where to start. You can start by talking with local universities, your state and local public health officials. There’s state pharmacy and physician organizations who may have more experience with the legislative process. Look at where your opportunities to ask for help are. Ask people for their input. You don’t have to do this all on your own.  W: Is there anything else that’s useful to prepare before choosing the legislative route? M: Having done a pilot makes a huge difference, because it shows that it can work in some part of your state. It shows that you know what might work and what won’t work. It can be hard to get a pilot done without a lot of funding, but sometimes you’ve got to use a little sweat equity, bite the bullet, and just do it. It doesn’t have to be large. You can work with a local health department to identify physicians that they have good relationships with already, or a county medical society. Having data ready is really important. W: All of this is valuable insight, thank you Mary! Although COVID-19 has interrupted some of these AD plans, what is your hope for what passing this legislation will mean for AD in Illinois?  M: Our current legislation specifically mentions supporting Medicaid providers. The goal is to expand it to all prescribers across Illinois. COVID-19 has also taught us a lot, and changed a lot of opinions on telehealth. I think as people become more comfortable with this platform, it will change how we approach AD. We’re also looking at expanding beyond physician prescribers to include Nurse Practitioners and Physician Assistants. It’s harder to get access to them. It’s an uphill battle to get names and contact information, and to know who the right providers are. But it’s important because NPs and PAs account for a large portion of prescribers for this patient population. W: I think we’ll definitely see a ripple effect, and hopefully see AD take hold more broadly. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Mary Lynn Moody BSPharm, is the Associate Dean for Professional and Governmental Affairs and a Clinical Associate Professor in the Department of Pharmacy Practice at the University of Illinois Chicago (UIC) College of Pharmacy. Ms. Moody graduated from the University of Illinois Chicago and completed a PGY1 Residency at Northwestern Memorial Hospital in Chicago. Ms. Moody’s clinical practice was in Drug Information at UIC. She is also currently the Director of Continuing Education at the College. In January, 2020 Mary was involved in launching the Academic Detailing Program at the college. An interview with Liesa Jenkins, MA, the Executive Director of ONE Tennessee, an organization devoted to addressing the opioid overdose epidemic statewide. by Winnie Ho, Program Coordinator Tags: COVID 19, Detailing Visits, Opioid Safety, Program Management, Rural AD Programs, Substance Use  Winnie: Liesa, thank you so much for taking the time to speak with us today about your experiences at the helm of ONE Tennessee through the past year. Can you tell us a little bit more about yourself and the AD-related work that you do? Liesa: As the Executive Director of ONE Tennessee, I have overall responsibilities that include strategic planning, funding, communication, and staffing in addition to coordinating our AD program. I’m responsible for recruiting, training, and supporting our detailers to be as effective as possible. Our mission is to combat opioid misuse and overdose, and AD is just one of many projects and strategies we have to do that. W: You certainly wear many hats in your leadership role! Can you tell us about the experiences that have shaped how you approach leadership?  L: There were a very diverse set of experiences that influence how I’ve learned to lead. It’s also important to recognize that leadership comes in all forms. I was a foreign language teacher for 10 years, I had to learn the many different ways of communicating information to students from young teens to older adults. You learn to consider the way you present your information to help get all of your students to their goals. I was also a director of a non-profit and managed volunteers. Just like my students, you quickly learn that people have many different motivations. A good leader knows how to cater to those motivations and learns how to maximize the team they’re working with. It’s also important to always remember to express gratitude towards your team, and as often as possible, remind them of the impact that they’re making. W: You’ve discussed a lot of the soft skills and characteristics that good leaders have. What about some of the technical abilities that helped you be successful at managing an AD program?  L: Before coming to ONE Tennessee, I worked at both the federal and state-level in healthcare-related consulting work. It gave me exposure to federal and state-level funding procedures, as well as the decision-making process that goes on behind the scenes. You also learn about the regulations and guidelines that AD helps to keep clinicians aware of. W: It sounds like you’ve had a fantastic journey on your way to the position that you have now in leading an AD initiative. Can you tell us a little bit more about the different community organizations that support ONE Tennessee’s AD work? L: We have support from multiple organizations including the Tennessee Pharmacists Association, the Tennessee Hospital Association, and the Tennessee Primary Care Association. They’ve helped us recruit clinicians to serve as detailers and to participate in detailing sessions. We also have support from the East Tennessee State University’s College of Public Health and the Tennessee Department of Health supporting our data collection and program evaluation. We are thankful to other provider organizations including local community pharmacists and clinicians at Alliance Healthcare Services to assist us in development and distribution of materials  W: That’s quite a dynamic bunch! At the intersection of many different groups in the community all focused on preventing opioid-related overdose, how do you keep all these different stakeholders on the same page? L: Even when you speak the same common language, not everything is always communicated and understood as intended. I work with a talented team from diverse career backgrounds, including finance, legal, communications, and policy professionals. They don’t all speak the same exact “language” because of their professional backgrounds. The role I often play in group meetings is that of a facilitator. I'm comfortable asking the so-called “dumb questions” or constantly asking for explanations. As a leader, it’s my job to make sure there is clear understanding among the folks in the room who don’t work in that field. It’s important as a leader to not only communicate well, but to also make sure everyone on your team is communicating well enough so that everyone can understand and also be understood.  W: Intentional level setting is a hallmark of effective leadership and communication. It allows meetings and decisions to be productive, and it ensures that everyone’s goals are aligned. Otherwise, important details may get left behind or not fully developed. L: Exactly. It’s also important to know that with your team, you’re never alone. You don’t need to know everything to be a leader, but you need to surround yourself with people who can collectively make decisions based on good information. Surround yourself with people who know more than you do, and listen to them. W: You picked up this role in the middle of a pandemic and with your leadership, we were able to launch our first virtual training pilot with ONE Tennessee for about two dozen detailers. It was a huge undertaking! What would your advice be for someone who’s looking to tackle big projects in their role as the leader of an AD organization?  L: I would say first and foremost – the determination to fulfill our commitments was important to me. I knew what was in our contractual agreement with our funders, and didn’t want to start off our organization with a fail in this category! Secondly, create a timeline with the concrete things that need to be finished and the resources you need to help you monitor progress along the way. Finally, in the face of making new things happen – it can be daunting when there’s a big mission to accomplish. When there’s nothing on the drawing board yet, a leader is someone who volunteers to put up the first “strawman” plan. It doesn’t need to be perfect, but it gives everyone something to build off of; it’s always better to start with something, like the first brick in the foundation. W: We’ve talked a lot about how to bring a community together to support an AD intervention. Why is community involvement important to the success of an AD intervention?  L: Well, whether you’re talking about opioids or HIV or chronic illnesses, the reality is that no one individual or organization within a community can solve a public health problem alone. Even though AD is mostly about the relationship between the detailer and the clinicians they work with, it’s informed by many other people who care about improving health outcomes. In short, the program would not be able to operate without the leadership and support of these partners! In a state as large as Tennessee, with such wide differences among rural and urban, from the Appalachian region to the Mississippi Delta, racially diverse but largely homogeneous in some places, it is important that collaboration occur at local levels as well as at state levels—both among clinical colleagues in the same community who care for the same patients, and also with support from state-level organizations who can leverage resources that may not be available in the local community. While individuals and organizations may not agree on all points, it is usually possible to find at least one shared goal that can be worked on together. As an organization, we strive to identify and then mobilize to address those common goals. There are great things ahead for us all if we continue to work together. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  In her current role as Executive Director of ONE Tennessee, Liesa draws upon her experience as an educator, a non-profit administrator, a state-level director of community health programs and a consultant to state and federal officials, as she works to advance the organization's mission to combat the opioid epidemic through collaboration and sharing of information among health professionals and communities in Tennessee. In her professional roles at Kingsport Tomorrow, CareSpark, Deloitte Consulting and the Tennessee Department of Health, Liesa has helped to develop and implement a broad range of collaborative projects at local, regional, state and national levels to improve community health, broadband access, education and literacy, employment opportunities, cultural arts exchanges, global trade, environmental protection, neighborhood revitalization, youth development and civic leadership. Her skills in strategic planning, resource development, mentoring and community organizing have been recognized with awards, including being named a Paul Harris Fellow by Rotary International, a Health Care Hero by the Business Journal of Tri-Cities, and the Commissioner's Award of Excellence from the Tennessee Department of Health. Liesa received her B.A. in French from King University in Bristol, Tennessee and her M.A. from the University of Kentucky in Lexington, Kentucky. She also holds a Certificate of University Studies from the Université de Franche-Comté in Besançon, France, and is certified as a Project Management Professional by the Project Management Institute. Liesa is a native of Glade Spring, Virginia, where she is a seventh-generation resident on her family's farm, and enjoys spending time with her three sons and their families, as well as quilting, reading, and traveling. Overview: Dr. Nate Rickles, PharmD, PhB, BCPP, FAPhA is an associate professor pharmacy practice at the UConn School of Pharmacy with experience in developing AD programs, most recently for the CDC-funded CEDPP (Connecticut Early Detection and Prevention Program) project. Dr. Natalie Miccile, PharmD, MBA currently works as a retail pharmacy manager at ShopRite Pharmacy. She’s working with Nate to onboard pharmacies participating in the CEDPP program and working with the pharmacy students who are supporting the process of referring patients to screening, diagnostic, and prevention services. by: Winnie Ho, Program Coordinator Tags: Cancer, COVID-19, Detailing Visits, Health Disparities, Program Management  Winnie: We’ve been excited for a chance to speak with you both! Nate, you spoke on our Clinical Innovations in AD session at the NaRCAD2020 Conference, sharing your work to support underserved, and sometimes undocumented, women in accessing care. Thank you both for joining us today – can you tell us a little bit more about the program and the issues it addresses? Nate: CEDPP consists of two components: the Connecticut Breast and Cervical Cancer Early Detection Program (CBCCEDP) and the Well-integrated Screening and Evaluation for Women Across the Nation (WISEWOMAN). The services are offered free of charge with the goal of significantly increasing breast and cervical cancer services for medically underserved women. The Department of Public Health’s traditional outreach method of using clinical navigators at established WISEWOMAN sites could only reach a relatively small population. We received a CDC Innovation Grant to investigate the role that community pharmacies could play in increasing referrals to a free public health prevention program for vulnerable populations, as these pharmacies are accessible, front-line, and generally well-trusted in the community.  W: That’s an important goal to close this gap and to ensure more women can access the services they need. Why did your team feel that AD was a useful approach to address the lack of access to screening services? Nate: I’m very passionate about the notion that building relationships through 1:1 connections are going to be more powerful long-term in creating behavioral change. AD works so well because the techniques are very persuasive in dealing with common barriers like pharmacists believing there’s little time in their day, not enough staffing, or not the right financial incentive. Our project manager Peaches Udoma had sent out flyers and e-mails to local pantries and shelters, but we hadn’t received many referrals through this tactic. The predominant way we’re getting referrals is through 1:1 outreach with pharmacists and our students reaching out to the referred participants to connect them with services.  Winnie: Can you tell us more about how your intervention navigated the pharmacists’ barriers you described? Natalie: We had a lot of interest from pharmacists, especially when they learned about the impact they could have. However, for a full month, we weren’t seeing results. When I checked in, we learned that they were genuinely overburdened with their workflow, which wasn’t surprising. We had to think about who else in the office could do it – and it turned out to be the pharmacy technicians. They were often at the point of sale and would be more likely to know if patients were uninsured or underinsured. We began detailing the pharmacy technicians directly instead. Many of them were bilingual, which helped in distributing the right flyers to the right women. We worked with the pharmacy technicians on communicating the benefits our programs offered, with attention to utilizing accessible language and avoiding unnecessarily complicated healthcare terms. We learned that emphasizing key things like free gym memberships or free nutritional services provided was very useful in getting women to agree to be referred. Addressing the language barrier and slight language changes was key to us finally getting referrals. However, when COVID-19 hit, we had to reassess since we started getting zero referrals again. It made sense as few people want to wait around in a public space, and pharmacies also became overwhelmed. Our team pivoted to reaching out directly over the phone after receiving lists of potential contacts from the pharmacies. We wanted to show our partners that we could be resilient in this time and to not let this program fall through.  Winnie: Pivoting your intervention to have team members directly contact the women you were trying to refer instead of through the pharmacy technicians must have required your team to make adjustments to accommodate language needs. How did your team tailor the AD intervention to address language barriers? Nate: We noticed that we had many of the women we reached out to who spoke Spanish as a native language, and quickly realized we were probably losing a lot of patients because of the language barrier. We onboarded a pharmacy student, Isabella Hernandez, who, in addition to being a very dynamic, charismatic, and outgoing person, also spoke Spanish. Once Natalie onboarded her and shared the main concepts around the screening and referral, Isabella was quickly able to pull in over 80 referrals; we didn’t have even half or a third of that through our prior efforts. We’ve been closely tailoring our work since, with flyers in Spanish, Portuguese, and in Arabic. We have also Arabic speakers to communicate with Arabic-speaking patients, and we have the capacity to expand into other languages.  Natalie: I originally worked with the lists of contacts we received and tried to engage directly. However, because we recognized our bilingual pharmacy students were able to better engage with these women, my role now is to oversee our callers, get their referrals, and help touch base with site navigators to ensure referrals are being processed, and how we can improve our screening process. We’re prioritizing language accessibility because our first encounters are first impressions. Our patients matter, and we want to make things as smooth as possible for them. We’re even at a point where Isabella is running trainings with our other callers, so she can give them hints on how to be more flexible in the conversation to fit our clients’ needs. Winnie: This is a really outstanding demonstration of flexibility and tailoring a program to address barriers to practice change. We hope that other programs continue to follow your example of integrating best practices to communicate with patients from diverse communities! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Nathaniel ("Nate") Rickles is an Associate Professor in the Department of Pharmacy Practice at the University of Connecticut School of Pharmacy. He received his B.S. in psychology and chemistry from Dickinson College, Pharm.D. from the University of the Sciences in Philadelphia, M.S. and Ph.D. in the Social and Administrative Sciences from the University of Wisconsin-Madison. Dr. Rickles also completed a psychiatric pharmacy practice residency and is board certified in this area. He was inducted as a Fellow of the American Pharmacists Association. His primary research interests are to develop, implement, and evaluate intervention programs that improve pharmacist communication with patients and/or other team members and subsequently to improve medication adherence and patient safety. Primary teaching interests involve courses on communication skills, mental health, health behavior change, cross-cultural health care, and research methods. Dr. Rickles is an active researcher with several grants and publications involving enhancing the role of pharmacists in changing patient and provider behaviors.  Natalie Miccile received her PharmD from the University of Connecticut School of Pharmacy in Storrs, CT and MBA from the University of Connecticut School of Business in Hartford, CT. Her MBA concentrations include Digital Marketing and Strategy and Investment Analysis. She works as a consultant for UConn School of Pharmacy on research initiatives that involve enhancing the role of pharmacists in the community setting and is pharmacy manager at Shop Rite Pharmacy in Milford, CT. Dr. Miccile is MTM certified and an active member of the Connecticut Pharmacists Association. This interview features Carla Foster, MPH, who leads the conceptualization, implementation, and evaluation of Public Health Detailing as an Epidemiologist within the Bureau of Alcohol and Drug Use Prevention, Care and Treatment (BADUPCT) at the New York City Department of Health and Mental Hygiene (NYC DOHMH). She is currently activated for the COVID-19 emergency response as Lead Analyst managing the Reporting Unit within the Integrated Data Team of DOHMH’s Incident Command System. By Winnie Ho, Program Coordinator Tags: Data, Detailing Visits, Evidence-Based Medicine, Health Disparities, Program Management, Stigma, Substance Use, Training  Winnie: Hi Carla! You’ve certainly had a lot on your plate with so many diverse campaigns. Can you walk us through the conceptualization process for your detailing campaigns, and how your team came to choose cocaine use as your current detailing topic? Carla: We can start with some data on this. In 2018, more New Yorkers died from drug overdose than from homicide, suicide, and motor vehicle crashes combined. Cocaine – in both crack and powder forms – has played an increasingly prominent role in this crisis. The mortality rate from overdose deaths involving cocaine more than doubled between 2014 to 2018, amounting to 52% of all drug overdose deaths in NYC. Some of the associated risks are serious - increased exposure risk to fentanyl, cardiovascular disease events and death.  W: That’s stunning data. Especially in the midst of the opioid crisis, it’s important that we don’t lose sight of other substance use issues going on right now. I’d love to learn a little more about the challenges and lessons that your team has learned by detailing on cocaine use. C: First, we have to be aware that fentanyl, a powerful opioid 50 to 100 times stronger than morphine may be found in many substances, including cocaine. We’re very concerned about fentanyl and cocaine because people who use cocaine do not have tolerance to opioids and are at even higher risk for overdose. It’s also important to address the perception of who is most impacted by high mortality rates. There’s this idea that cocaine use is more prominent in younger populations, but our data show that it’s actually impacting an older population more than many might expect. In particular, residents age 55-84 in the Bronx Borough have experienced the largest increase in cocaine overdose death rates in New York City from 2014 to 2018.  That’s why it’s critical for us to raise awareness in an effort to mitigate misconceptions and stigma around risky use and those who may have a substance use disorder (SUD). In addition to shame, there are still very real potential socioeconomic and legal consequences from disclosing substance use, which can deter folks from even seeking help. We take into account the unjust consequences of policies applied unevenly according to race, and how this impacts implicit biases in terms of which patients are thought to use substances, which types of substances they might use and even more critically, which type of treatment, if any, they are offered. Implicit biases combine with the effects of systemic racism to compound these consequences. It’s important to note that it’s not race that drives poor health outcomes, but racism.  W: Challenging stigma is one of the most powerful ways that detailing campaigns can combat the damage done by the War on Drugs, because stigma can make the difference of whether or not people receive dignified care. With a campaign so focused on addressing stigma and with a topic this important, how do you prepare your detailers for this task? C: We devote a significant amount of time towards training our detailing reps – a week-long training, 8 hours a day. We spend a large amount of that time talking in detail about stigma as related to cocaine use. It’s critical to us that our detailers are comfortable and knowledgeable when speaking about this topic, because it sets the tone for the providers who then set the tone for their patients. We ensure that our representatives are prepared to respond to a wide range of questions or comments, because this builds the provider-detailer relationship and enhances the value of the detailing visit. We’ve found during our follow-up visits that this support has led to high provider engagement with the campaign and providers reporting incorporation of the key recommendations into their daily practice, which is the aim of our public health detailing campaigns.  W: How have providers responded when detailed on a topic that carries so much stigma? C: The good news is that we’ve found NYC healthcare providers to not only be receptive to our work on substance use, but they’re eager to partner with us to support their patients once they learn about the severity of the issue. Our team provides statistics that relate to the provider’s specific neighborhoods and specialty, giving them real-time pictures of what’s happening with the patients they see. We know that it’s still a difficult topic to bring up, so we help address this with our action kit resources on stigmatic language and counter-top brochures that signal to patients that the provider’s office is a safe place to discuss these issues.  W: It gives me tremendous hope to hear about that there’s been enthusiastic response from providers. It means that things are changing. Let’s also talk a bit about program sustainability. Your team has worked extensively on campaigns across multiple topics. What have you learned from implementing past campaigns? C: Each public health detailing campaign is different, but we’ve learned some key strategies that support the growth and success of subsequent campaigns: 
Our overall goal is to do everything we possibly can to improve the health of our fellow New Yorkers. I like to remind our detailers of this James Baldwin quote that informs our public health detailing mission: “Not everything that is faced can be changed, but nothing can be changed until it is faced.” Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Carla Foster, MPH is an Epidemiologist at the New York City Department of Health and Mental Hygiene (NYC DOHMH). Her research focuses on the implementation and evaluation of public health detailing campaigns across New York City with the aim of reducing overdose mortality. Prior to joining the NYC DOHMH, she led development of clinical practice guidelines at the American Urological Association. She received dual Bachelor of Arts degrees in Africana Studies and Neuroscience from Wellesley College. Carla also obtained her Master of Public Health Degree in Epidemiology from Columbia University. By: Winnie Ho, Program Coordinator 2020 was a year of many hard-earned lessons. We’re so fortunate to have an AD community that’s committed to sharing best practices, tips, and experiences. This communal knowledge base is what makes us stronger and allows us to all grow together. Here’s a collection of the great advice some of our DETAILS Best Practice Blog and Discussion Forum guests have given us this past year: Tags: Detailing Visits, Evaluation, Program Management Planning and Team Building: "The most critical thing is to allow enough time for the planning process – ideally, 18 months before you’re looking to launch. This allows you to gather resources, make partnerships internally and externally. If you can reach out to colleagues in the field, learn about what are good mistakes to avoid. It’ll save you a lot of time!" -Carla Foster, NYC Dept. of Health and Mental Hygiene (NYC DOHMH) "My best tip would be to create a standard operating procedure (SOP) or some type of guidebook for your visits. Our team developed a SOP which discusses how to conduct a needs assessment, conversational tips, how to weave in key messages, and how to address barriers. Developing the SOP really allowed me to understand the intricacies that need to be addressed before launching the campaign. It works as such a good practice guide, and you can always refer back to it whenever you need it." -Julie Anne Bell, NYC Dept. of Health and Mental Hygiene (NYC DOHMH) "One thing I’ve learned about AD is that it’s only as effective as your intervention across an entire system. Any work that I’m doing is irrelevant unless I’m addressing the culture of the entire system. If the front desk staff isn’t on board, or the clinical staff isn’t a believer, or the CEO doesn’t understand – there will be challenges that will be harder to overcome." -Andrew Suchocki, Clackamas County, Oregon, Medical Director  "Building relationships with key stakeholders has made all the difference. They’ve helped me curate my detailing aids and key messages, and have even allowed me to practice my detailing sessions with them." -Kelsey Bolton, Gundersen Health System, Wisconsin "A strong team is an important part of a detailing campaign. Strong teamwork means supporting each other through tough detailing sessions, communicating well, and keeping a positive attitude. During virtual times, turning the camera on during staff meetings can also help keep the team spirit alive!" -Marlys LeBras, RxFiles Academic Detailing Service in Saskatchewan, Canada Gaining Access: "There are numerous external pressures when it comes to AD, but the most important part is keeping the human aspect in check when reaching out to providers. We can get bogged down into the guide posts, the bench posts, or the numbers – but the COVID-19 era reminds us that it’s all about empathy." -Tara Hensle, University of Illinois at Chicago/Illinois ADVANCE "You may find it helpful to create an e-Detailing materials packet and see if you can grab some time with providers over a virtual platform. It can be a helpful foot-in-the-door for future in-person detailing!" -Jess Alward, New Hampshire Division of Public Health, Dept. of Health and Human Services "Lunch time is still the best time for visits. They were the most popular when I did it, and they’re still the most popular now, as my team tells me." -Terryn Naumann, British Columbia Provincial Academic Detailing (BC PAD) Service Conducting Field Visits: "There’s a lot of listening that happens in AD. You might spend all this time learning about the topic before you meet the providers, but if you take the time to really listen to them, you might learn more than you came with. There is so much to learn from all the incredible people you meet in AD." -Debra Rowett, Drug and Therapeutics Information Service (DATIS) in South Australia "The big thing I’ve learned through networking with detailers is to be flexible and be prepared for any situation, especially in the virtual environment. You might have one idea of how your session will go, and it could go in the opposite direction, which is part of the charm of detailing. Also, practice mock detailing with your colleagues!" -Vishal Kinkhabwala, Michigan Dept. of Health and Human Services "It’s important to have several different ways of presenting information to providers and to use varied approaches to barriers or objections that come up. I typically focus on emotional connection, financial concerns, and the evidence behind the key messages I’m delivering." -Brandon Mizroch, Louisiana Dept. of Health  "No visit is ‘one-size-fits-all’. You need to consider the provider, their situation, and their environment and decide what will be the best way to deliver the evidence. It’s critical that you’re attentive to the provider you’re detailing and that you continue to focus on the needs assessment at all times." -Mary Liz Doyle-Tadduni, Alosa Health in Pennsylvania "I was delivering an in-person visit, and the skeptical questions about AD from the provider kept coming. I tried not to be defensive, but I answered everything I could. Eventually, the provider allowed me to get to the topic, and that changed everything! By the end of the visit, the opposition took an about-turn. I gained a professional friend and ally and ended up seeing this person with virtually every topic over the next 20 years. Never write someone off because of some seemingly extreme pushback – you just never know!" -Loren Regier, Centre for Effective Practice (CEP) and Canadian Academic Detailing Collaboration (CADC) "Confidence is key. You can study and practice everything with your team, but at some point you have to get out there and just do it! You have something valuable to offer and a few opportunities a year to capitalize on that value. A strong relationship can overcome a difference in clinical background or even a rough start. It just takes enough of your effort to show that you’re really there to be of service. Remember, you wouldn’t have been hired in this role if you weren’t qualified!" -Amanda Kennedy, Vermont Academic Detailing Program  "When addressing stigma, it’s important to note that tough conversations can produce some cognitive dissonance in people. All providers are human. They care about their patients. What helps is not overwhelming them with data, but repeated snippets of information over time to help reinforce the message." -Elisabeth Mock, Maine Independent Clinical Information Service (MICIS) "Don’t be afraid to ask for a specific behavior change and remember to follow up to make sure that change occurs. The ‘ask’ can be hard for detailers, so I always tell them to frame it as, “based on what you’ve heard today, what is one thing you’d do differently?” -Tony de Melo, Alosa Health in New England Data Collection & Evaluation: "We encourage providers to complete a post-visit survey. We ask them to share their level of agreement that they were given new/different information, and they intend to implement practice changes as a result of AD conversations." -Jacki Travers, Pharmacy Management Consultants in Oklahoma "It’s important to track a mix of quantitative and qualitative data, and the critical components that should be tracked are the outcomes and the process of detailing. Data is absolutely critical for getting leadership buy-in, especially if it can tell a story." -Kristefer Stojanovski, San Francisco Dept. of Public Health "Once you’ve identified the problem you’re addressing and done the work to understand it, jump in! AD works!" -Jennifer Pruskowski, University of Pittsburgh Medical Center  Thank you to the AD community for your resilience, compassion, and incredible work through a tumultuous year. We hope the AD community continues to share its pearls of wisdom with us through the new year. We are excited by all the progress made in 2020, and look forward to a brighter 2021 with you all. Best, The NaRCAD Team Evidence into Value and Action: Reflections on 30 Years of AD in South Australia (Part Two)10/5/2020
An interview with Debra Rowett, BPharm, Adv Prac Pharm, FPS, the Director of the Drug and Therapeutics Information Service (DATIS) in Adelaide, Australia. Debra joins Winnie Ho, NaRCAD Program Coordinator in a two-part conversation about a 30-year career of pioneering academic detailing in Australia and reflects on the past, the present, and the future of the field. In Part Two, we discuss the evolution of academic detailing as the world of healthcare changes. You can read Part One here. Tags: Detailing Visits, Evidence-Based Medicine, International, Medications, Program Management  Winnie: You wear so many hats when it comes to AD. How have those roles changed over your time with DATIS? Debra: Before I was Director of DATIS, my role was primarily around developing our detailing materials, and evaluating the evidence and our program. I was always interested in the synthesis of evidence and turning that into value for clinicians. I was a clinical pharmacist who was working with people across many disciplines, and there was a growing body of evidence, but translating that into practice was always a challenge.  W: I think you touch on a fundamental aspect of AD – that we turn evidence into value, and that we translate all this research into action. It’s very critical that AD continues to provide that independent, trusted, unbiased source of information to ensure evidence is disseminated responsibly and utilized properly. D: I would agree with that, very much. We live in an information-dense era and much of the information is synthesized and aggregated at the population-level, but clinicians are responsible for decisions at the individual patient level. I think AD is about bringing evidence to the point at which clinical decision making is made. W: I’m curious about your experience with evaluating evidence for AD materials. It’s clearly a difficult, but super important aspect of AD. You have all these clinicians who are trying their best to make the best possible decision for their patient – and AD comes in, and in many ways, helps share in that responsibility.  D: Evaluating evidence is also about recognizing what we don’t know in the evidence. When reviewing the evidence for an AD program, we look for where there are gaps in the evidence, where there’s controversies, and differences in opinion about the evidence. No matter how well done, you make choices along that entire process about what to include, what to exclude – and even with the synthesized evidence, there is still human judgement about how to use it. W: Right, and that human judgement also needs to focus on how that evidence came to be and how it was produced. D: Absolutely. As we know evidence-based medicine is not just about the randomized controlled trials and published evidence, it’s about the intersection of published evidence, clinical judgement, and the patient’s specific needs, goals, and circumstances. The real opportunity for AD is that you can personalize this information for the provider to work with.  W: It’s extraordinarily rewarding work, and it’s a constant process in grappling with the things we don’t know. As someone who has been in this work for a long time and has had to adapt a long-standing AD program to changing guidelines and medical evidence, you’ve likely seen some big shifts in the medical consensus. Take opioids for example – the consensus around the safety of its use has had a dramatic change over the years. How have you adapted when the evidence base can sometimes change quickly within a few years? D: It’s important that we come to providers with a balanced view, and that we acknowledge with them that there is uncertainty, that there is complexity, and that it isn’t easy to make these decisions with their patients. There’s a lot of things that we don’t know. If you come with too much certainty, you lose credibility because translating evidence into routine clinical practice is complex. Every time a medicine is prescribed for and used by a patient, we’re forecasting how the future will proceed - the exact benefits and harms that a patient will experience are uncertain.  People are living longer and with multimorbidity which presents new medical challenges. We’re seeing more people living with issues like musculoskeletal problems, hypertension, diabetes, renal problems, atrial fibrillation, and surviving their myocardial infarctions. The number of medications that patients take now compared to 30 years ago have increased. There are individual guidelines for each condition, that don’t necessarily take the other comorbidities into account. The drugs used to treat one issue may lead to treatment conflicts for another condition and needs to be taken into consideration. It’s not just in one area of practice that has changed too, or just our demographics – we’re seeing fewer solo General Practitioners and more team-based practice in Australia. AD needs to take all of that into account when considering how to detail, and also who to detail.  W: Can you explain what you mean by “who to detail”? D: It’s important to understand who the decision-maker is and what the decision you’re trying to address is – for some of our AD programs it might involve other health professionals; it’s not always the doctor. W: Right, and this whole of office approach looks at all the players involved in the continuum of care, and acknowledges that they may play a role in how clinical decisions are ultimately made.  D: Yes, and I think this is why AD is even more important now than it was when we first started. It allows us to bridge individual condition silos, and helps providers navigate multimorbidity. Healthcare is never a one-size fits all, even for an individual. Their circumstances and treatment goals can change over the course of their lives. AD can personalize the information and tailor it to the needs of the clinician. AD can also be the conduit between population level evidence and its translation into clinical decision making - that is one of its greatest strengths. W: NaRCAD has been lucky to see overarching growth of AD programs everywhere, along with all of its exciting new innovations and evolutions. Any final thoughts on AD before we hear from you at our upcoming conference? D: One of the things I try and impart when teaching the method of AD is to value the knowledge of the person you are detailing. There is a lot of listening that occurs in successful AD if you are truly to meet the needs of the provider you are visiting. If you keep at the very heart of what you do, respect for learning together and hold true to the principles of academic detailing, you will meet incredible people everywhere you go. It makes for a wonderful career. (Part Two of Two) Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Debra Rowett, BPharm, Adv Prac Pharm, FPS, has led an academic detailing team for over 20 years and is a member of the team which designed, developed and delivered the “Best Practice in Educational Visiting” training for academic detailers in Australia. Debra has worked closely with NPS Medicinewise since their inception and has provided consultancies to other national and international academic detailing programmes. Debra is an experienced academic detailer with expertise in designing, developing, training, implementing and evaluating academic detailing programmes. Debra has served as the President of the Australian Pharmacy Council and is currently the Vice President of the Council of Pharmacy Schools. Debra has worked extensively in the area of quality use of medicines, inter-professional practice, policy and health workforce development in Australia. Debra is a member of the national Drug Utilisation Sub-Committee of the Australian Pharmaceutical Benefits Advisory Committee (PBAC). An interview with Debra Rowett, BPharm, Adv Prac Pharm, FPS, the Director of the Drug and Therapeutics Information Service (DATIS) in Adelaide, Australia. Debra joins Winnie Ho, NaRCAD Program Coordinator in a two-part conversation about a 30-year career of pioneering academic detailing in Australia and reflects on the past, the present, and the future of the field. In Part One, we introduce you to DATIS and academic detailing in the Australian context. Stay tuned for Part Two! Tags: Data, Evidence-Based Medicine, International, Program Management 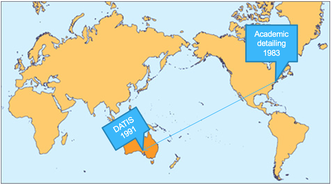 Winnie: We’re so glad to have a chance to chat with you about your long career in AD, Debra! Debra: This is a great part of the job, talking to other people in the AD community. It really is a great privilege to be working with academic detailing organizations in different countries. I’ve loved getting to meet and learn from so many different people. W: I would agree! I’m sure you have some great stories of what it’s like to work internationally in this field. D: One of the things that it has really highlighted is the nuance of language. At a training workshop in the U.S early in my career, I was saying how we would meet with doctors in their "surgery", and how important it was to meet them in their surgeries close to where they make decisions. The workshop participants really politely said to me, but isn’t surgery a really bad time to detail? Oh! Surgery – I meant their office.  W: We really would have quite a different communication model if we had detailers visiting providers mid-surgical operation! This does gives us a good starting point into discussing how Australian AD is unique. Besides the context of the word "surgery", what else would our non-Australian colleagues need to know about Australia to understand the context of what you do with the Drug and Therapeutics Information Service (DATIS)? D: I have been involved with DATIS since its formation in 1991. I was a clinical pharmacist at the Repatriation General Hospital, a teaching hospital, when Jerry Avorn’s paper was published. His work on how AD could influence clinical decision making really resonated with us in Adelaide. One of the big things to know about Australia is that we have a National Medicines Policy, which aims to improve positive health outcomes for all Australians through access to and quality use of medicines. DATIS was one of the first programs funded through the Quality Use of Medicines initiative, and in 1998 NPS MedicineWise (formerly the National Prescribing Service) was funded.  W: Australia is enormous - it must be a challenge to cover. What is the geographical coverage of your AD program? D: South Australia has a population of about 1.4 million people and a vast geographic reach – the furthest of my AD visits is about 800km (500 miles) away from where we are! We work to provide AD to over 85% of all family physicians in South Australia, so about 1,300 General Practitioners (GPs) each year. We provide AD services to aged care, primary care and hospital providers. We also work in partnership with NPS MedicineWise who have implemented AD at the national level. W: That’s certainly an enormous coverage zone, especially for those core 12 people! How has this work manifested in South Australia?  D: At the heart of our program is service, and we build our program to emphasize that. There are three aspects of DATIS: service delivery of detailing visits, training of detailers, and research. We have a core team of 12 people who carry this work out alongside our colleagues who join us for various projects. Because of our multiple different contracts, the clinicians we provide services to can see us for multiple reasons in a year. Between visits, providers will ring us with clinical questions about therapeutic issues that have arisen in their practice. We have also developed interprofessional communication training to support interprofessional practice with a focus on pharmacists and physicians. Our AD programs usually seek to address a therapeutic area or clinical issue however a recent AD program we developed with our hospital pharmacy colleagues was to support pharmacist preceptors implement a performance outcome framework based on entrustable professional activities for interns and undergraduate pharmacy students. W: It's incredible that DATIS has such a focus on this three-pronged approach, because it continues to help push our understanding of best practices in AD through implementation, study, and training others to carry on the work. Can you tell us a little more about the foundation that DATIS is built upon?  D: Behavior change theory and implementation science has informed our work from the outset in 1991, including the development of the training program which was designed in collaboration with psychologists and experienced GP medical educators. Social marketing frameworks, an adult learning approach, the concept of cognitive biases, clinical reasoning all recognize the many interacting and complex influences on behavior. We try to learn from these and apply to the design and implementation of AD. We also use pharmacopidemiology methods to understand evidence to practice gaps and for evaluation. As AD evolves and changes, something I really emphasize is staying true to the principles of AD – this is a rigorous process. W: We’re seeing innovations all over the world and across so many clinical topics. Are there any unique innovations that you feel differentiates Australia AD from other AD programs?  D: One innovation that we're exploring is applying the principles of AD to patient behavior change interventions. As part of person-centered care, it is important for patients to understand their medicines, and to be involved and empowered in shared decision making. We haven’t called this work AD, but have applied the principles of AD in this research. Complex clinical decisions need to be made each and every day by providers, and it's a privilege to be able to bring providers the best available evidence through academic detailing services, part of the power of AD is the adaptability and personalization to providers along the continuum of care. We are seeing the world of healthcare change, and we have so much to learn as it does. (Part One of Two) Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Debra Rowett,BPharm, Adv Prac Pharm, FPS, has led an academic detailing team for over 20 years and is a member of the team which designed, developed and delivered the “Best Practice in Educational Visiting” training for academic detailers in Australia. Debra has worked closely with NPS Medicinewise since their inception and has provided consultancies to other national and international academic detailing programmes. Debra is an experienced academic detailer with expertise in designing, developing, training, implementing and evaluating academic detailing programmes. Debra has served as the President of the Australian Pharmacy Council and is currently the Vice President of the Council of Pharmacy Schools. Debra has worked extensively in the area of quality use of medicines, inter-professional practice, policy and health workforce development in Australia. Debra is a member of the national Drug Utilisation Sub-Committee of the Australian Pharmaceutical Benefits Advisory Committee (PBAC). An interview with Tara Hensle, a research coordinator with the University of Illinois - Chicago, School of Pharmacy (UIC) and Illinois ADVANCE (Academic Detailing Visits And New Evidence CEnter). by Winnie Ho, Program Coordinator Tags: COVID-19, E-Detailing, Opioid Safety, Program Management, Substance Use  Winnie: Hi Tara! It’s been a crazy year so far, hasn’t it? We want to check in with you and the University of Illinois, Chicago (UIC) team about your experiences in navigating the pandemic. Can you tell us a little more about yourself and your role in the ADVANCE academic detailing team? Tara: I was hired about 7 months ago as the research coordinator, and it’s been one heck of a 7-month run. The majority of my work is focused on implementation, so I do all the scheduling and outreach to hospitals to talk to providers. I develop and establish relationships with office managers and providers, and I assign detailers to visits.  W: Our team at NaRCAD has been lucky to have worked with the UIC and ADVANCE team for a while through our trainings and your presentations at our conferences and our webinar series, and we’re excited about the research intervention that had been planned. Can you tell us a little bit more about the mission? T: Our intervention is a CDC-sponsored, three pronged approach that’s built off a pilot program that we started in 2018 for Chicago-land providers. We have a team of about 30 detailers who are now trying to cover as much of the state as possible. We wanted to follow-up with providers to get a sense of whether or not the ‘dosage’ of AD made a difference, but we also wanted to expand the providers we worked with, and to introduce updated topics like the new features of the Illinois PMP or opioid alternatives. The third prong is creating a toolkit to give programs a blueprint and resources of what was effective for us. We would love to make the “how to” of AD more accessible to other groups.  W: Compared to other programs, you have quite a large and robust team at UIC. It must have been difficult for the pandemic to hit right in the middle getting your program launched. T: It really impacted our recruitment as we had called providers from the end of January through early March 2020. There are a lot of things going on right now. Even a small ask, such as 15 minutes of their day, can feel like a big ask for providers. W: Right, and interventions are very carefully laid out and planned ahead of time. COVID-19 has disrupted everything – especially those on the frontlines who are both detailing and being detailed. Can you tell us a little bit more about how else the impact on your original plans for the intervention?  T: We had been so focused on ramping up that by the time we hit mid-March, we had many people on deck reaching out to providers. We started hearing “No, we can’t do this right now” or “this is a really bad time” often. Once the stay-at-home order came through, we stopped contacting offices for about 2 months. We had to sort out so many protocols and even our IRB to make amends for virtual visits. What we’ve found since we’ve resumed virtual visits in May is that there’s a lot of variability – some offices have capacity because they aren’t seeing many patients, while others have providers that have been transferred to hospitals and have no idea when they’ll be available. We’re also talking about layoffs and burn-out and low morale.  W: There are many of considerations on how best to proceed safely right now. One is looking at the impact on the critical work you’ve done on opioid safety. Unfortunately, the pandemic has only exacerbated the overdose epidemic. What progress has been made on your opioid initiative? T: One of the ways our team has shifted has been moving to virtual visits. We knew that these would have its own difficulties, such as concerns about “no-shows”. But our team is relatively tech-savvy, and now my job is making sure they’re all familiar with how to troubleshoot the technological pieces of virtual visits. There are a lot of tech issues that can interrupt a visit. So we do mock detailing and have the detailers practice with each other, where we introduce certain needs and obstacles, maybe even a tech problem for instance, we role play a provider not turning on the webcam, or not being able to see your screen. Practice to strengthen adaptability and resilience become important in ensuring the detailers are prepared. W: There’s definitely no time like right now to test detailing skill and ability to think on your feet! As a research coordinator, what do you think you’ve learned in the past few months? T: How to be flexible! There are all sorts of external pressures right now to keep our project on track, but the most important part is keeping the human aspect in check. Having some insight and empathy for providers is important to understand what they’re going through. We can get bogged down into the guide posts, the bench posts, or the numbers – but this era reminds us that it’s all about empathy. W: At the end of the day, we want better for our patients, for our communities, and for health outcomes everywhere, right? T: Absolutely! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Tara Hensle is a research project coordinator at the University of Illinois – Chicago for a CDC-funded research study investigating the effectiveness of academic detailing for opioid prescribing. She received her Bachelor of Science in Behavioral Science and Speech Pathology at Purdue University, and has worked in a variety of healthcare research settings before coming to UIC. Since working on this project, she is inspired by academic detailing’s simplicity, versatility, and the variety of topics to which it could be applied. An interview with Marlys LeBras, PharmD, a clinical pharmacist with RxFiles Academic Detailing Program. by Winnie Ho, Program Coordinator Tags: COVID-19, E-Detailing, International, Program Management  Winnie: Thank you for speaking with us today Marlys! Can you tell us a little bit about your work with the RxFiles Academic Detailing team? Marlys: Absolutely! I’ve been with RxFiles for just over 4 years as an Information Support Pharmacist doing both frontline academic detailing as well as co-leading various academic detailing training sessions, with the most recent being this past April. Our program covers Saskatchewan, Canada, but our website, app, and book are used outside of the province and Canada as well.  W: RxFiles is definitely one of the larger and more established programs we’ve had the honor of partnering with through the years. Can you tell me how maintaining the daily operations of your program have been impacted by COVID-19? M: One of the bigger things that’s changed for our team has been moving our academic detailing training sessions online for our team of 12 detailers. We had to shorten our two-day in-person training, and shifted to hosting shorter sessions and offering more pre-training day and post-training day webinars to cover all of the content, including “how-to virtually detail”.  W: No matter how well virtual substitutions are planned, it’s not the same as being together. We’re all really missing our colleagues, and it’s heightening a sense of isolation. How do you think your team has adjusted to moving the training online? M: I think our team adjusted quite well to the training adaptations. We were able to give them enough notice about the shift. What came out from training days is that our team members really do miss being in-person and having that social interaction – even the chit-chat in between sessions. For in-person trainings, we typically have time for a team-building activity in the evening where people catch up. We’ve been trying to incorporate more games and fun into our virtual training to have that social aspect. Personally, I really miss debriefing with colleagues in-person after detailing visits.  W: It seems like keeping the team connected is a big part of your team culture. How has your team stayed connected through the pandemic? M: We typically do a roundtable at the mid-point of a detailing topic. We typically go around and share a little bit about our detailing experiences. Pre-COVID, no one wanted to turn on their cameras. It was never a requirement, but now everyone is turning them on. It’s been really nice just seeing people’s faces. Also, one of the things that’s been nice about going virtual is that we are able to open up staff meetings and invite more detailers to participate with us. We would have never been able to do that as easily in person.  W: We’ve seen opportunities like these spring up as teams need to be particularly innovative under tough circumstances that prevent in-person connection. Speaking of teams, dream teams don’t come out of nowhere. A lot of work goes into creating and maintaining a strong, positive, and connected team. At NaRCAD, we talk a lot about what makes a good detailer, but what are some of the hallmarks of a strong detailing team? M: Team work is a really interesting thing to dive into. I reflected on this question, and think that a strong detailing team supports one another. That support can be helping each other out in the detailing session itself (e.g. co-detailing), or through communicating with each other about the providers we serve and in between detailing sessions (e.g. a prescriber moved from one detailing area to another). We want the team to be successful in moving towards our goals together. Another thing that COVID brought to my attention is that a strong detailing team also has a positive attitude. I really feel that during our transitions, everyone has been really positive and embraced the changes.  W: You’ve shared a lot of examples of how your team regularly communicates at various points during a detailing campaign, which shows a culture of checking in and making sure no detailer is left out. Can you speak a little about how that culture’s been built up at RxFiles and how you maintain it? M: I think Loren Regier, who is in charge of Projects, Transitions and Training, has been such an asset in the development of our program, has really emphasized checking in. He really showed us the value of that, and not only does he talk about it, he has made it very easy for someone to approach him and talk about how the detail went, both the successes and challenges. W: Having access to mentorship, and making sure a team-based approach is emphasized by leadership is key. It’s clear that the RxFiles team is doing well in adapting to these challenges faced by so many detailing teams. Maintaining positivity and seeing challenges as opportunities for growth is something that’s critical for teams to continue to have an impact. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Marlys LeBras is a clinical pharmacist with the RxFiles Academic Detailing Program at the University of Saskatchewan. She completed her Bachelor of Science in Pharmacy at the University of Saskatchewan, her Hospital Residency with the former Regina Qu’appelle Health Region, and her post-graduate Doctor of Pharmacy (PharmD) degree at the University of British Columbia. Overcoming the Impossible: Pivoting to Meet the Needs of Family Physicians During COVID-196/10/2020
An interview with Lindsay Bevan, MScHQ candidate, Project Manager, Primary Care Academic Detailing Service, Centre for Effective Practice by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: COVID-19, Detailing Visits, E-Detailing, International, Program Management  Anna: Hi Lindsay! Thanks for chatting with us today about the exciting work happening at Centre for Effective Practice (CEP) in Canada. Can you tell us about your role and share some highlights from your team’s recent work? Lindsay: I’m the manager of the primary care academic detailing service at CEP. We have a provincial service, which started in March of 2018 that serves family physicians across Ontario. Prior to our current service, we have run services in long-term care to support appropriate prescribing as well as primary care to support diabetes management. Our current service is still growing, but we’ve served just over 880 family physicians to date. Our focus has mainly been around opioids and chronic pain. We were just about to launch a series of “visits” (campaign topics) on prescribing in older adults, but we quickly pivoted to meet the needs of family physicians and began working on a visit around managing primary care in the COVID-19 context.  Anna: It’s so important to understand and meet the needs of family physicians when it comes to academic detailing, especially during a tremendously stressful time. Can you tell us a little bit more about the COVID-19 visit and the process behind its launch? Lindsay: Our provincial government declared a state of emergency in Ontario on March 17th, so we knew COVID-19 would be top of mind for our physicians and that they’d need more information. We also knew that we’d have to deliver the visits virtually, which was a fairly new territory for us. We had to modify our usual content development and detailer “upskilling” (bringing detailers up to speed on the content, key messages, and evidence around the topic) processes in order to meet the demands of family physicians by getting them information around COVID-19 when they needed it. The content development process for our other visits typically takes six months, with the detailer upskilling taking the last month and a half of that six-month period. COVID-19 turned everything upside down and made us rethink what we assumed was impossible. Within two weeks of the declaration of emergency, we started pulling together content for our COVID-19 resource centre (clinical tool for this visit, which is also available to all primary care providers), one week later we started training our detailers and within a month, we were delivering virtual visits to family physicians.  Anna: It’s impressive how quickly your team was able to launch this visit. COVID-19 is different from other topics that your team has focused on because the information and guidelines are continuously changing. How has your program kept detailers up to date? Lindsay: The detailer upskilling process for other visits includes weekly webinars to review key messages and the surrounding evidence, and a two day in-person workshop where detailers get to practice their visit discussions with each other and family physicians prior to launching visits. We also use a content development team for our detailing tools and bring those tools to the detailers to review when they’re about 90% complete. We typically don’t edit or change those tools after visits have begun. For our COVID-19 visit however, the detailer upskilling weekly webinars and the content development for our ever-evolving online COVID-19 resource centre have been continuous, ongoing processes. Our detailers have also taken on a larger role within both processes. Each detailer has been responsible for searching for, appraising and synthesizing information on a specific sub-topic of COVID-19, and then submitting this information for inclusion in our resource centre as well as presenting it at our weekly webinars to their fellow detailers. Our detailers need to be up-to-date on the emerging and evolving evidence and jurisdictional guidance around COVID-19 because family physicians don’t have time to sort through all the information being made available to them daily during the outbreak. Anna: It’s critical to provide physicians with the most up-to-date information, especially in situations like the COVID-19 pandemic where they’re bombarded with new recommendations and guidelines from multiple sources on a daily basis. How many COVID-related visits has your detailing service provided to physicians during this time? Lindsay: We’ve had 95 initial visits to date and approximately 12% of those visits have been with physicians whom we’ve never detailed before. We’re just starting to reach back out to physicians to see if they would like a follow-up visit since evidence has evolved and challenges have changed since we first started. The initial conversations were focused on testing, assessing and managing patients with the virus, and we’re now seeing those conversations shift to focus on resuming primary care services within the COVID-19 context. The detailers have done an amazing job in transitioning their detailing conversations to ensure they’re always covering the emerging areas of interest and need for family physicians. We’ve seen little to no requests from physicians for detailing visits on anything but COVID-19 or on maintaining care in the context of COVID-19, which speaks to the impact this topic has had on family physicians.  Anna: Wow – it’s amazing that your service has been able to detail so many physicians on COVID-19 while also recruiting new ones. Lindsay: Yes, overall, the visits have been well-received. We were a bit more cautious with our approach to promoting our COVID-19 visit and recruiting new family physicians. We didn’t want to add to the current noise at this time. Instead, we took a more passive but strategic approach, like adding a banner to our website where family physicians can quickly sign up for a visit, and having our partners share our visit and resource centre with their membership base. One of the neat things about this visit is that because we’re offering it virtually, we’re able to expand our geographical reach and provide our detailing service to more physicians.  Anna: Using a virtual platform certainly has its pros, especially within the world of academic detailing! What has your program’s experience been like with integrating e-Detailing into your service? Lindsay: The transition wasn’t unsurmountable for our detailers because they are quick learners, and we’ve had a lot of support through the resources offered by NaRCAD and our partnership with the Canadian Academic Detailing Collaboration (CADC). We also did internal virtual training sessions with our detailers where they were able to practice using all the features of the Zoom videoconferencing platform. Overall, it’s been a positive learning experience, and one that has furthered our team’s ability to be adaptable and enhanced our problem-solving skills. We do feel however that there’s been an impact on the detailer-physician relationship since we’ve transitioned to virtual detailing, especially for the 12% of family physicians who are new to our service. When a detailer is in a physician’s practice, they can see how busy a waiting room is or how stressed the staff appear to be. When family physicians join a virtual detailing visit, it’s much harder to gauge what kind of day they might be having and adjust the discussion accordingly. Furthermore, the act of going into a physician’s practice itself can create goodwill that helps establish and strengthen the detailer-physician relationship, and that opportunity is lost during virtual detailing.  Anna: That’s an excellent point. Observing the waiting room and interacting with office staff is also essential to a detailer’s needs assessment. Detailers lose this piece of a visit when the detailing is done virtually. Is virtual detailing something that CEP will continue doing once COVID-19 related restrictions are lifted? Lindsay: Our detailers and family physicians would like to return to in-person visits. There seems to be some conversations that lend themselves better to virtual communication, and others for which an in-person presence offers greater value and impact. When it comes to relationship building, in-person interactions still offer something special. We would also like to build off the momentum we’ve started with our virtual visits. We’re exploring the idea of offering virtual detailing to family physicians who would otherwise have their visit rescheduled due to extreme weather or to family physicians located where we don’t already have a detailer covering the area. We’ve all done what we thought was impossible in providing the majority of healthcare visits virtually. I hope that folks across the healthcare system will continue to use that momentum moving forward to increase access to care.  Biography. Lindsay Bevan works for the Centre for Effective Practice (CEP) where she collaborates with a team of amazing individuals to develop and implement evidence-based supports and services to help narrow the gap between best evidence and care in Ontario. As a project manager, she oversees the planning and implementation of the CEP’s primary care academic detailing service, which serves family physicians across Ontario. Prior to joining CEP, Lindsay worked at the University Health Network in the infection prevention and control unit, where she updated internal infection control policies and developed patient and provider educational material. Lindsay is currently completing her Master of Science in Healthcare Quality at Queen’s University. Wearing Multiple Hats at Alosa Health: Detailing Clinicians, Managing Programs, and Training Staff1/22/2020 An interview with Tony de Melo, RPh, Director of Clinical Education Programs, Alosa Health by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Detailing Visits, Opioid Safety, Program Management, Training  NaRCAD: Tony, thanks for chatting with us today about your role at Alosa Health! What’s been the most exciting part of the work that Alosa has done this year? Tony: Our partnership with Aetna, a managed health care company and health care insurer. We’ve been working with them to provide educational outreach to providers on chronic pain, acute pain, and opioid use disorder (OUD); supporting them in managing pain using non-opioid drug options; appropriately dosing opioids when they need to be used; tapering down patients who are on existing high doses of opioids; and helping to identify patients that may have opioid use disorder. We’re now working in Pennsylvania, Virginia, West Virginia, Ohio, Illinois and Maine. NaRCAD: That collaboration does sound exciting! Now, let’s talk a little about your role at Alosa. You actively detail, you manage academic detailers in the field, and you lead trainings at Alosa. Which aspect of your role is your favorite, and why? Tony: When I’m training and managing detailers, I see myself more as a coach than a trainer. I’ve always liked educating and teaching—I enjoy helping others develop their skills and seeing them improve. Training folks and coaching them in the field is rewarding to me because I feel that I’m impacting what they’re doing in their own communities. It brings me happiness to see others succeed. NaRCAD: As a coach, how do you know when your work has been impactful? Tony: When I work with detailers in the field, I can see firsthand that they are able to be impactful with the providers because they are bringing about behavior change with their message delivery and confidence. We can also measure how impactful our work is by reviewing our Salesforce data. I can see from the detailer’s visit notes when providers have agreed to a behavior change, and this is a true measure of our work being impactful.  NaRCAD: With success comes challenges. What are some of the major challenges you see academic detailers face in training and in the field? Tony: The major challenge is teaching detailers to have a conversation with clinicians rather than a lecture. Making the visit more conversational doesn’t often come as naturally as presenting the information in a lecture format, but the conversation must be about understanding where the provider is now, what their needs might be, and how to deliver content to make behavior change. In the field, the major challenge is access to providers. Many health systems have regulations and restrictions for those who want to meet with providers, because representatives in the pharma industry have bombarded and overloaded providers throughout the years. As a result, we’re often seen as an outside influence or an outside visitor, so we aren’t always given the opportunity to meet with a provider. NaRCAD: With these challenges in mind, how do you instill confidence in academic detailers as a trainer and as a manager? Tony: We spend a lot of time practicing and providing feedback during trainings. We practice individually, with partners, and with outside folks who are playing the role of providers. Practicing multiple situations, multiple times, over multiple days, builds confidence. We also videotape the trainees so that they can see what they’re doing well and what they can improve upon. As a manager in the field, it’s quite similar. I usually sit down with each detailer after a visit and discuss what worked well and what they could do differently in their next visit, so that each visit becomes a learning opportunity. Providing feedback and being a mirror for the detailers helps them to build confidence and skills as time goes on. I also offer the detailers my perspective; having spent time doing this myself and observing others, I can share the tricks, skills, and wording I’ve heard throughout my time with the detailers.  NaRCAD: Those are all great ways to build confidence among detailers. What’s one piece of advice that you would give to academic detailers? Tony: Don’t be afraid to ask for a specific behavior change, and remember to follow up to make sure that the behavior change occurs. One thing that I find to be hard for academic detailers is the “ask”, where detailers are asking for commitment or behavior change from a provider at the end of the visit. I always tell detailers to frame it as, “based on what you’ve heard today, what is one thing you’d do differently?” Follow-up then ensures that providers are committed to change and holds them accountable for what they said they would do. NaRCAD: That’s extremely helpful advice for detailers. What’s the best thing a program manager could do to maintain high levels of engagement among detailers? Tony: As a manager who’s coaching or guiding others, it’s important to build trust between yourself and the folks you’re coaching or managing. It can be lonely when you’re in the field detailing by yourself, so managers need to have touchpoints with their detailers. Building trust and having your detailers know you’re all working together helps them stay self-motivated; it makes them want to go out into the field and do a good job because they know someone is backing them up. NaRCAD: Thank you for taking the time to chat with us today. We value your unique perspective on detailing, managing, and training!  Biography. Tony de Melo manages field staff and leads academic detailer trainings at Alosa Health. He attended Massachusetts College of Pharmacy and Health Sciences in Boston, where he received a BS in Pharmacy with a minor in Business Administration. This business interest led him to work for several pharmaceutical companies as a sales representative, account manager, training manager, district/regional manager, associate director of managed markets training, head of sales training, and development & marketing product manager. He has also worked for smaller businesses that were looking to grow their sales and marketing programs. Throughout his career, Tony has successfully sold, marketed, trained, led, designed, developed and executed solutions to meet business objectives. An interview with Jennifer Pruskowski, PharmD, BCPS, BCGP, CPE, a palliative care pharmacist at University of Pittsburgh, School of Pharmacy by Winnie Ho, Program Coordinator Overview: This intervention is taking place in the University of Pittsburgh Medical Center (UPMC) Senior Communities in Pittsburgh, Pennsylvania. Dr. Pruskowski's work is funded by The Beckwith Institute. Tags: Deprescribing, Elderly Care, Medications, Program Management  NaRCAD: Hi Jennifer, thank you for taking the time to speak with us today! You are breaking new ground on a deprescribing academic detailing project in Pittsburgh. What role does deprescribing play in improving health outcomes in nursing homes? Jennifer: Deprescribing is the identification and discontinuation of potentially unnecessary or inappropriate medications. What I really love about deprescribing is that it’s really patient-centered. For example, one medication class might be appropriate for one patient, but maybe not for the next. Within the UPMC Senior Communities, I have developed, implemented, and evaluated a clinical pharmacy-driven deprescribing initiative named the DE-PHARM Project, which stands for the "Discussion to Ensure the Patient-centered, Health-focused, Prognosis-appropriate and Rational Medication regimen". Say that 5 times fast! This project allows pharmacists within the nursing home setting to review medication regimens and conduct conversations with nursing home residents, their families, and their caregivers. Deprescribing allows us to rebalance the equation when there may be medication overload, and helps us to reduce the burden on our patients.  NaRCAD: What are unique factors when approaching deprescribing work in nursing homes? Jennifer: While a lot of patients outside of the nursing home are complex, the nursing home population is one of the most obvious and at-need, due to their reduced functional status and their need for additional services. Nursing home residents also tend to receive their care, essentially, from one provider. So, it’s very conducive for deprescribing, and it allows us as an academic detailing program to overcome one of the main barriers to deprescribing, which is tracking down and contacting potentially numerous prescribers. NaRCAD: That's a pretty common barrier, to track down and identify the multiple providers that are supporting the patient.  Jennifer: Absolutely. The other thing to consider is that there are already regulations in place within a nursing home setting that encourages deprescribing. Every nursing home that receives Medicare or Medicaid has certain regulations to follow, which is basically all of them. For example, since the mid 2000’s, there’s been verbiage around ‘gradual dose reduction’ for anti-psychotics, and then in the last 5 to 7 years, this was expanded to antimicrobials as well to try to curb growing antibiotic resistance. Nursing homes are built for deprescribing, in the sense that these medications are continuously monitored and every quarter, they need to justify to CMS why someone is on a medication at a certain dose. However, what gets challenging is integrating care goals, functional status, patient perspectives, and evidence-based literature into deprescribing. Nursing home settings often times have a comfort-focused treatment plan. The medications that I tend to focus on when encouraging deprescribing may not be the same as other detailers. For example, many detailers are working on opioid-related campaigns. Opioids are crucial for deprescribing, but if you think of a patient who is closer to the end of life, opioids are typically not what we target because the medication tends to align with their treatment plan and goals. NaRCAD: That’s a really interesting and complicated situation. What are some of the other challenges you’re facing with approaching deprescribing in nursing homes?  Jennifer: One of the big challenges is that no studies have been done about the initiation of certain medications in nursing home residents. Most clinical trials are also done in healthier, younger adults. We don’t have the most literature to guide a lot of what we do, and it’s critical because our prescribing goals are going to be different for the nursing home population as compared to the general population. NaRCAD: This can often be a challenge when initiating an academic detailing campaign in a field that may not have as many other detailers. One of the foundations of academic detailing is the dissemination of evidence based information, but as you mention, there are not as many resources and studies in the work you’re about to partake in. As you and your team begin to initiate your program, how do you plan on approaching this paradox? Jennifer: So, the first thing that we’re doing is determining the medication that we’re going to target. We’re taking a look at prescribing cultures within the nursing homes that we’re targeting, and our working group is looking at what medication regimens are potentially inappropriate, or deprescribing eligible. There is an evidence-based algorithm that we utilize for our intervention based on what medication class we will target from deprescribing.org, run by Barb Farrell, a friend and colleague of mine in the Canadian Deprescribing Research Network. So for some medications, such as proton pump inhibitors or histamine blockers, there are resources that have been created. However, as we do the groundwork for our program, we could potentially find ourselves targeting a medication class that doesn’t have a lot of evidence-based literature around it, and then that will be both the challenging and fun part of developing verbiage and guidelines around that.  NaRCAD: Someone’s always got to do it first! It can be difficult getting programs started, and we are very lucky to have a growing population of people who are interested in integrating academic detailing into their programs. As you’re reflecting and planning for the future, what would be important for someone else in your shoes to know about starting a new program? Jennifer: The most important part is really thinking through the needs assessment. We know that there is a problem, and now it’s about identifying the specific issues and critically thinking through a solution. We will really need to understand the prescribing behaviors that exist in our nursing homes. Much of the prescribing culture there is based off inertia, extrapolation, and people doing their best to adapt important regimens from information that doesn’t directly address their unique situations with nursing home residents. We are trying to see if, for example, our providers are prescribing certain medications because they see this problem a lot in other populations they work with, or if they are working off of knowledge that has not been updated in many, many years. These would be two very different academic detailing interventions. NaRCAD: And finally, as we begin a brand-new decade in 2020, what would you say to anyone else looking to consider academic detailing? Jennifer: Jump in! Academic detailing is a proven intervention to effectively disseminate evidence-based literature. I would say that as much as academic detailing can feel like a one way street – as a detailer coming to give a provider information – it really is more of a two-way street than people think. I think in the small amount of time that I’ve done this, I feel like I’ve actually gotten more information from our prescribers than I feel like I’m giving to them at the end of the day. NaRCAD: A fantastic note to end on. Thank you so much for taking the time to speak to us, and we wish you and your team continued success in 2020!  Biography. Dr. Pruskowski received her PharmD from Wilkes University in Wilkes Barre, Pennsylvania. She then completed a Post-Graduate Year One Pharmacy Practice and Post-Graduate Year Two Geriatric Residency from the Williams Jennings Bryan Dorn Veterans Affairs Medical Center in Columbia, South Carolina, as well as an Interprofessional Palliative Care Fellowship at the James J. Peters Veterans Affairs Medical Center in Bronx, New York. Dr. Pruskowski is a Board Certified Pharmacotherapy Specialist, a Certified Geriatric Pharmacist, and a Certified Pain Educator, and has received specialized training in pain management from the American Society of Consultant Pharmacists and the American Society of Health-System Pharmacists. Her clinical practice site is the University of Pittsburgh Medical Center (UPMC) Palliative Supportive Institute (PSI) as the Palliative Care Clinical Pharmacy Specialist.  An interview with Rachel Lemons, Project Manager, ONE Tennessee by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Opioid Safety, Project Management NaRCAD: Thank you for taking the time to speak with us today—we’re excited to hear about you and your team! Can you tell us a bit about ONE Tennessee and how your organization first became involved with academic detailing? Rachel: ONE Tennessee is a state-wide nonprofit healthcare collaborative who is focused on fighting the opioid epidemic. We were founded as an outcome of a summit hosted by the Tennessee Department of Health called “Turning the Tide.” The summit joined together healthcare professionals and stakeholders to discuss best practices for tackling the epidemic. Academic detailing was highlighted as a best practice during the summit and it was collectively decided that it would become one of our initial projects. ONE Tennessee brought the academic detailing pilot program to life through the opioid crisis funding the Department of Health received from the Centers for Disease Control and Prevention. NaRCAD: We’re glad to know that the strategy of AD was highlighted! You’re now managing a program of detailers focused on opioid safety across the state of Tennessee—tell us what that’s like. Rachel: Exciting! Once our detailers were trained by your team, my role was very much supportive in nature. I helped our detailers to identify clinicians in their communities, and troubleshoot any issues. We were fortunate enough to be able to recruit a passionate group of pharmacists for our pilot, and that made my job easier from a clinical standpoint, since they’re the subject matter experts on opioid prescribing. They‘re on the front line of the epidemic, and they fit the perfect mold for engaging with clinicians to build a strong and trusting relationship. NaRCAD: You recently completed the pilot stage of your program. What would you say are some of the biggest lessons you’ve learned so far about building an academic detailing program? Rachel: Getting in the door was one of the biggest barriers our detailers faced. From a programmatic standpoint, I think ONE Tennessee could have done a little more foundational work for our detailers, like speaking with our stakeholders and educating them on academic detailing as it relates to the opioid initiative—that would have really helped our detailers gain access to clinicians. We also learned that time was a barrier for our detailers. Our initial grant period was only one year, and things moved very quickly. We recruited full-time community pharmacists, so having the bandwidth to prepare and complete academic detailing visits was often difficult, especially if there was limited employer support.  NaRCAD: Those are all familiar challenges across many of the programs we support. How did you maintain strong relationships with your detailers and support them in the work that they were doing in the field? Rachel: I always had an open line of communication with our detailers. We had standing monthly webinars, but it was difficult to find a time that worked for everyone because they were full-time pharmacists. Our detailers were scattered across the state and were mostly in rural areas, so I was not able to meet with them in person; however, I was available via email, phone call, and text message. I learned early on that I had to meet detailers where they were. Some detailers did not have time to check email, so it was easier to do a quick call at lunch or early in the morning before their day got started. It really depended on the needs of the detailer, but I always maintained an open line of communication. NaRCAD: That’s a great model, and regular communication helps detailers feel a sense of community through a project. Other supports are often more concrete, like tools and resources. What are some that you've found to be critical to program success, and why? Rachel: I think first and foremost, our partners, specifically NaRCAD, the Tennessee Pharmacists Association, the Tennessee Hospital Association, the Tennessee Nurses Association, the Tennessee Medical Association, and the Tennessee Department of Health, were a tremendous resource that made our program incredibly successful. Google’s platform (Google Drive, Google Sheets, and Google Docs) was also critical to our success, as it allowed us to share data and updates in real time. We did not have access to specific evaluation tools because we are a young organization and our grant period was only one year. Our shared space online helped me to stay organized and capture information from our detailers all in one place, and it was free!  NaRCAD: These are all great reflections for AD program managers to learn from. Based on the successes and challenges of this pilot, where do you see your program in a year? Rachel: I see us continuing our current model with our inaugural group of academic detailing community pharmacists while working towards designing, developing, and implementing a “train -the -trainer” model in partnership with your team. I also see us having discussions with large and small hospital systems to customize plans to fit their unique needs related to opioid safety. Most importantly, we want to continue to support the state and our other healthcare stakeholders who are with us on this journey. NaRCAD: We’re happy to help support that vision. Any other important advice/tip that you’d give to other young programs? Rachel: Patience. You must have an understanding that there are going to be pitfalls, but if you have the support and the right people involved, your program is going to succeed. Also, don’t try to reinvent the wheel if you don’t have to. There are so many other programs out there — reach out to people and have conversations! NaRCAD: Rachel, thank you so much for sharing your experiences with us. We're excited to see the impact of your program into the future.  Biography. Rachel Lemons found passion for public service early on in life. She is committed to assisting those with the greatest need in her community. She’s working to effect change socially and through public policy. She is a graduate of East Tennessee State University, where she received her Bachelor of Science in Public Health. Her involvement with Tennessee’s Opioid Epidemic began with the Department of Health, where she was exposed to the State’s rapid response in this fight which lead her to joining ONE Tennessee as a Project Manager. She continues to build her career with a practical and wide ranging set of experiences in order to gain a global perspective on health issues facing communities today. Rachel is an active member in the Junior League of Nashville, Tennessee Public Health Association and currently serves as the Board Intern at Cheekwood Estate & Gardens in Nashville.  Copyright Gifford Productions https://giffordproductions.com/ Copyright Gifford Productions https://giffordproductions.com/ Please refer to our Conference Hub page through narcad.org for all conference related videos and slides, which are available as of December 2nd, 2019. by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Conference, E-Detailing, Jerry Avorn, Program Management Our team at NaRCAD was proud to host the 7th International Conference on Academic Detailing on November 7th and 8th, 2019 in Boston to a sold-out crowd of health professionals engaged in clinical outreach education. With this year’s theme emphasizing collaboration and innovation, our Director, Dr. Mike Fischer, kicked off Day 1 of NaRCAD2019 by reflecting on the past decade of NaRCAD’s work, while also discussing our exciting plans for the future, and highlighting the importance of enhancing connection between attendees to support their work ahead. Dr. Melissa Christopher, National Director for the Veteran Affairs (VA) Academic Detailing Services, was next to take the stage as the Day 1 Keynote Speaker. She provided the audience with an overview of the current work by the Department of Veterans Affairs National Academic Detailing Service and how it supports a High Reliability Organization culture. She also spoke of the future of academic detailing at the VA, which includes expanding their reach with virtual detailing (“e-detailing”) and advancing their electronic health records through ordering safety alerts and real-time PDMP data.  Copyright Gifford Productions https://giffordproductions.com/ Copyright Gifford Productions https://giffordproductions.com/ Other day 1 highlights included an expert panel presenting on the successes and challenges of implementing e-detailing within their programs, sharing stories and insights about when, why, and how to connect virtually with providers. Our small group breakout sessions explored the fundamentals of academic detailing, with sessions focused on the basics of an academic detailing visit, how to identify and apply the most reliable sources of evidence-based research, and how to successfully lead an academic detailing program. Day 1 also included our annual “lightning round” of Field Presentations, a session that highlights aspects of recent academic detailing interventions. Topics included the use of academic detailing to improve maternal and neonatal health through safer opioid prescribing, the effects of academic detailing on pediatric antipsychotic prescribing in the Medicaid population, and increasing access to Nalaxone in New York City through academic detailing. The afternoon also included a talk on Aetna’s opioid strategy and ongoing initiatives, with a focus on leveraging provider and system relationships to incentivize physician engagement and catalyze behavior change.  Copyright Gifford Productions https://giffordproductions.com/ Copyright Gifford Productions https://giffordproductions.com/ Dr. Jerry Avorn, Co-Director of NaRCAD, ended the Day 1 presentations with his Annual Academic Detailing Talk, addressing the importance of moving beyond the silos that exist in most healthcare settings, and how academic detailing can encourage the integration and collaboration of roles and initiatives to create synergy. That collaboration and synergy was illustrated during our evening’s Networking Reception, where we launched our new Mentor Match Program to great success, pairing those just starting out in the field with mentors who are part of more established programs. Day 2 provided similar opportunity for exploration and dialogue about program expansion. We kicked off with Keynote Speaker Tupper Bean, Executive Director from the Centre for Effective Practice (CEP). He discussed CEP’s journey to sustainability as an independent, not-for-profit organization, and reminded the audience that sustainability is a parallel process, not an “add-on”. To further explore sustainability, our Day 2 Plenary highlighted capacity-building strategies, best practices, and opportunities for expansion in clinical outreach education programming.  Day 2 Field Presentations provided opportunities to learn about more active AD programs, including topics such as identifying barriers to opioid prescribing through academic detailing, a team-based model and approach to AD, and a new AD campaign exploring cannabis as an alternative tool for patients experiencing pain. Our afternoon wrapped up with workshops focused on relationship-building for program sustainability, understanding stigma when supporting patients with opioid use disorder (OUD), and building AD campaign materials with limited resources. We’re grateful to all those who attended, and beyond the 2 days of connection at the conference, we at NaRCAD are committed to creating continuous opportunities for connection, support, and collaboration among all of you who make up our incredible network. Keep an eye out for our Annual Community survey, which we’ll send you in early December to find out what you need as you make an even greater impact in 2020! -The NaRCAD Team OVERVIEW: Boone County, West Virginia was one of 4 original site selected for years 1 + 2 of a pilot program of the CDC (Centers for Disease Control and Prevention), NACCHO (the National Association of County and City Health Officials), and our team at NaRCAD (The National Resource Center for Academic Detailing). This exciting pilot program focused on community-level work with local public health departments to develop customized interventions to reduce opioid overdose and death. Six sites experiencing significant public health problems related to opioids were selected over the two years to be trained in academic detailing; those trained health professionals then conducted 1:1 field visits with front line clinicians to impact behavior around prescribing, treatment referrals, and patient care, all within a rural area. As year 2 comes to a close, we’re showcasing stories from the field. Tags: Detailing Visits, LOOPR, Opioid Safety, Program Management, Rural AD Programs  Via NaRCAD, NACCHO, & the CDC’s pilot project, “LOOPR”, we were able to connect with high-burden counties across the U.S. whose rates of high prescribing and high fatal and non-fatal overdoses identified them as a county in need of support. NaRCAD worked on the implementation of an academic detailing initiative over the course of 2017-2019 with Boone County, located in rural West Virginia. Boone County ranks as the 22nd most vulnerable county across all counties in the United States, with the highest drug overdose mortality rate of all counties in West Virginia. Due to these and other data, Boone was identified as a key county in which to test the implementation of an academic detailing program, in which trained detailers would speak to clinicians and pharmacists about safer prescribing of opioids, checking the state’s prescription drug monitoring program to avoid dangerous co-prescribing of opioids and benzodiazepines, and to try and provide treatment, non-opioid therapy, and resources to patients in need.  One of the most unique approaches across all 5 sites of the LOOPR Project was carried out in Boone, with the team of 5 detailers being hand-selected from the nearby University of Charleston West Virginia’s School of Pharmacy. Four of these five recruited detailers were students in training to become pharmacists; one detailer works at the university as a professor of pharmacy. Selecting pharmacy students and faculty allowed for many positive approaches to the project, as well as creating unforeseen challenges. Programs considering hiring student detailers can often rely on the flexibility of students’ schedules, as well as an enthusiasm and energy for learning that may exist in smaller quantities later in one’s career, when full-time roles in healthcare take priority. While many career-established clinicians may have little room in their schedules to squeeze in 1:1 sessions with fellow clinicians, students may have more of an ability to shift their schedules, especially if they are not yet carrying out residency.  a reflections from Boone County’s Detailing Team, it’s clear that best practices in detailing should also consider the vast amounts of new information that students are absorbing early in their learning careers, and that learning clinical content may take longer to grasp. In addition, the comfort level with new clinical information may lead to less confidence in discussing best practices, especially with clinicians whose careers are much more established. Finding the right balance of tenacity, communications savvy, more time to ramp up to comfort in delivering and leading 1:1 sessions, an additional amount of technical assistance provided at more frequent intervals, and additional practice time or shadowing time with a mentor, can all benefit student detailers who are training to join a clinical outreach education team in a high burden area. With these elements in place, a student detailer may be poised for success—however, other considerations include the fact that students may have new projects, graduation pending, or life events which may end up limiting their ability to dedicate consistent time to a project rolled out over many months.  Other reflections from the Boone County AD Team included looking carefully at the social climate in which AD interventions of this nature may be implemented. While no county is free of potential clinician-level or community-level stigma, particularly around issues such as opioid use disorder, Boone’s AD team shared a particularly challenging setting within which the local community was not as supportive of evidence-based harm reduction initiatives as would be beneficial. One detailer’s suggestion to raise the visibility of and advocacy for harm reduction included considering a public health campaign prior to a detailing campaign, to ensure that subsequent roll-out of detailing is more sustainable and met with an openness from clinicians to consider behavior change. NaRCAD’s work with the public health department in Boone County, in partnership with the students and faculty of University of Charleston, West Virginia, provided the kinds of insights critical to learning from a pilot project of this nature. As with many pilot studies, any information gathered can illustrate a clearer picture of the landscape within which public health initiatives can be implemented, so that future projects may have a greater impact. With many thanks to the student and faculty team of Boone County’s Academic Detailing Project team, we and our partners are grateful to have learned so much over the past two years. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|
