|
An Interview with Lutricia Woods, RN OVERVIEW: Bell County, Kentucky was one of 4 original sites selected for years 1 + 2 of a pilot program of the CDC (Centers for Disease Control and Prevention), NACCHO (the National Association of County and City Health Officials), and our team at NaRCAD (The National Resource Center for Academic Detailing). This exciting pilot program focused on community-level work with local public health departments to develop customized interventions to reduce opioid overdose and death. Six sites experiencing significant public health problems related to opioids were selected over the two years to be trained in academic detailing; those trained health professionals then conducted 1:1 field visits with front line clinicians to impact behavior around prescribing, treatment referrals, and patient care, all within a rural area. As year 2 comes to a close, we’re showcasing stories from the field. Tags: Detailing Visits, LOOPR, Opioid Safety, Rural AD Programs, Substance Use  NaRCAD: Hi Lutricia, thanks so much for taking the time to speak with us about your work as an academic detailer for the opioid crisis in your community. Can you talk to us about how the opioid crisis has presented itself in Bell County, Kentucky? Lutricia: There’s not a family in this community that hasn’t been touched by the opioid crisis in some way. Twenty years ago, I worked in hospitals as an RN discharging patients and providing them with their prescriptions as they prepared to go home. At the time, I was shocked at the rates of prescriptions of opioids with benzodiazepines, and patients thinking it was safe. From my perspective, in our community, the opioid crisis really began by doctors beginning to prescribe many opioids to their patients without education or an understanding of the dangers. Three years ago, I was working on a project at a middle school, and was surprised by the number of grandparents that were raising their grandchildren because their children were either in jail, or otherwise affected by opioid use disorder [OUD]. In Bell County, we also have so many people unable to find a job because they cannot pass a drug test, and once that happens, they return to use because of the stressors of not being able to find a job and pay their bills, and it becomes a challenging cycle to overcome. 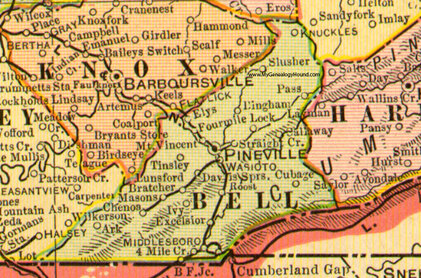 NaRCAD: Thanks for sharing your perspective, Lutricia—it can be true that some clinicians don’t see the impact of their role in prescribing opioids, and many times may believe that people who develop an opioid use disorder do so because of a moral failing, rather than seeing it as a medical issue. Did you think 1:1 outreach, provided directly to prescribing clinicians, would lend itself to improving patient health in response to the opioid crisis in this community? Lutricia: I desperately hoped it would. The opioid crisis is very personal to me, as it is to many people in our community. Years ago, my mom had 2 surgeries within 6 months. She had complications from one of those surgeries, and as a result, she was in the hospital for 6 weeks, during which time her care providers did not wean her off of the opioids she took immediately after the surgery. She returned home with prescriptions for opioids at a high dosage, and she developed opioid use disorder. My mother’s doctor, with whom I worked, reached out to have a conversation with me. He told me that I had to be the one to intervene with my mother because she continued requesting more opioids. I conveyed that I wanted her to discontinue taking them, and that he needed to assist us in finding a way to do this, as I felt his prescribing without discussing safety caused the initial issue. His response was that he wanted to “keep her happy.” My mother struggled for the rest of her life; she was able to completely wean off and discontinue using them, but it required a lot of counseling. As a result of this experience, I became a drug education coordinator, as I really wanted to do my part to mend the opioid crisis by providing drug education for every student in the county. And then, of course, I became an academic detailer for this project over the course of the past 2 years, which involves clinician education about safety and risk of opioid prescribing.  NaRCAD: Thank you for sharing that Lutricia; the opioid crisis is personal to so many of us. What would you say has been the most impactful piece of this academic detailing intervention as you went into the field and spoke with clinicians? Lutricia: The most impactful piece has been the ways in which we’re trying to hold clinicians accountable for their roles in the crisis, as well as leveraging their ability to improve things based on their relationships with their patients. For many of the doctors and nurses I met with, our conversations and educational resources have made them more thoughtful and intentional about their role. They seem to realize more that they have the power to decrease the number of prescriptions they write, the length of time for which they write them, and talk more with their patients about safety. NaRCAD: That’s fantastic. What about the most challenging part of this project—what’s been hardest about meeting with clinicians to talk about the opioid crisis in Bell County? Lutricia: Getting an appointment to go in and meet with these clinicians has been so frustrating and challenging. I always say that the receptionists in doctors’ offices are the most powerful people in the world. If you can’t get through them, you’re not going to get what you need, and it is the same with the patients. I couldn’t even get in to see my husband’s doctor, who we’ve known since we were kids. My husband had an appointment, so I resorted to going with him, and did a detailing visit on the spot with his doctor. This same doctor ended up changing practices, and it’s been a lot easier to get into that practice—all because of the office manager. Those relationships are important.  NaRCAD: Getting in the door is definitely a consistent challenge across many programs. We’ve heard from other detailers that practice makes perfect, and sometimes it’s easier to gain access when you actually show up and request a meeting in person. What else did you learn after being in the field? Lutricia: When I was “volun-told” that I would be attending a training, and doing “academic detailing”, I didn’t truly understand what it was or what the impact would be. I’m a big picture person, and I couldn’t see the big picture at all; I went into that training not knowing what to expect. It wasn’t until I actually started making visits that I could start to see the seeds we were planting to begin to have an impact. Share your thoughts on this piece in the comments section below, or learn more about the LOOPR project and other opioid safety academic detailing initiatives here and on our Detailing Directory.
0 Comments
Leave a Reply. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|
