|
An interview with Megan DeNubila, Provider Relations Manager, and Jessica Alward, Academic Detailer, from the Bureau of Infectious Disease Control with the state of New Hampshire. Their mission is to improve public health by promoting evidence-based practices in the areas of infection prevention, screening, testing, and management for HIV, TB, STD/STIs, and Hepatitis. by Winnie Ho, Program Coordinator Tags: Detailing Visits, HIV/AIDS, Rural AD Programs, Sexual Health, Stigma  Winnie: Thank you both again for joining us today! In one of our past technical assistance discussions together, we’ve gone into depth about some common clinician stigma and barriers. In particular, you shared with us that because New Hampshire was a lower incidence state for HIV, you would encounter clinicians who felt that that particular issue didn’t really fall within their patient population. It’s a common barrier we hear from many detailing programs, whether they address opioid use disorder (OUD) or infectious diseases. Can you go into more depth about your experiences with this phenomenon, and how you’ve addressed it? Megan: Providers are extremely busy, and they’re often expected to be an expert on so many topics. Our program helps bring providers filter through new information so they can start to bring it up with their patients. By walking them through the best practices, the recommendations, and local and state-specific data, we can show them that it’s something that is impacting their patient population. In addition, one of the things that stuck with me from the NaRCAD training we attended was that because there’s so much new information, providers would be expected to read up to 17 papers a day just to stay current. Something like HIV would be one of many things that providers are concerned with on a daily basis. Our job is to help bring the most relevant and evidence-based information to the surface for them and their patients.  Jess: Megan is completely right on this! I’m in provider offices a lot. What I hear is that they often feel like they're just treading water and not able to keep up with new information. What we try to do is bring that info to them in a way that doesn’t feel like just one more thing to squeeze into a day. When we talk to them about stigma, we don’t want to start there. We want to start with some easy and really useful information and tools that will make their job easier. By doing that work first, they feel like the precious time they are giving to us is worth it. After a couple visits, emails, or phone connections have happened, that's the time to bring up new approaches and topics. Winnie: I really appreciate that your lens on this barrier embodies a ‘How do we best support you?’ attitude. The goal of academic detailing is to navigate and close knowledge gaps in hopes of changing clinician behavior. Sharing knowledge and having difficult conversations is our best tools to address clinician stigma and discomfort. It’s not a battle against them and certainly the goal isn’t to shame clinicians. This is a collaborative operation to improve health outcomes.  Megan: Right, in the end, our mission is to close health inequities altogether. If I were a clinician and wasn't comfortable or familiar with best practices for preventing HIV, then I might feel a high level of hesitation trying to broach something like taking a sexual history from my patient. But if it’s something that I get more comfortable with, I’m more likely to bring it up and ask the right questions. Ultimately, we’re trying to build a relationship with the provider so they see us as a resource when a new practice, tool, or clinical guideline comes out. They can then use those tools and information to address stigma that a patient may be experiencing. Providers constantly have new information and guidelines thrown at them, and we would like to help make it easier for them to take that information and apply it in their daily work.  Jess: Whenever I address something uncomfortable with a provider, stigma or otherwise, I try to create an environment where we can work collaboratively on the issue and the provider feels as though I am a resource for them. I will say something like, ‘the last we talked, you mentioned this to me and it really got me thinking….” Or “I was talking with a colleague the other day about….” Then I will find a way to circle back around to the original topic. By approaching the topic in this manner allows them to feel we are a partner and have a shared goal. Winnie: I want to circle back to your team’s mission of addressing health inequities. Inequity is the core of why we discuss things like stigma and discomfort. We need to approach clinician stigma with a human approach, but we also need to address the very real impact that it can have on patient health outcomes.  Megan: In a mostly rural state like New Hampshire, healthcare access is limited to begin with, and clinician stigma could drive patients who need help to either forego care or have to travel very far to seek care that they are comfortable with. We know providers want the best outcomes for their patients, and through detailing, we want to help the providers achieve those outcomes. Looking at potential stigma is one of the keys to making sure we address health inequities. Winnie: A lot of these experiences about clinician stigma are anecdotal, but as you just outlined, they have a very real impact on health outcomes. From our previous call, we have discussed and imagined a tracking tool for these encounters with clinician stigma and barriers. What would you find useful about a tracking tool like this, and what would you hope to learn from the data?  Megan: A tracking tool would help us better understand and represent the stigmatic responses that are out there. It would help us focus our efforts to help a provider address stigma in their practice. Anecdotes are helpful, but it can be hard to grasp. We don’t want to make decisions by theorizing what patients are experiencing. As a small state program with limited resources, this would help us optimize our response and to make sure we’re heading in the right direction by seeing if stigmatic behaviors change. Winnie: It would be extremely exciting to see a tool like this become available and specialized for the hundreds of detailers who do this work. Megan: Yes, it’s a theoretical tool at the moment, but we were in discussions prior to COVID-19 about how to develop it. It would be amazing to see programs collaborate on something like this. I can only imagine how much further we’ll go with that as a resource. Biography. Megan DeNubila is the Provider Relations Manager for the Bureau of Infectious Disease Control, New Hampshire Division of Public Health Services. She has been leading the Public Health Education and Detailing team since August of 2018. Megan has over 8 years of public health experience in capacity building, coalition development, and community health. She earned her Master of Public Health degree from the Boston University School of Public Health with a concentration in Maternal and Child Health in 2016/2017 and her Bachelor of Arts degree in Health: Science, Society and Policy from Brandeis University in 2012.  Biography. Jessica Alward has been with the State of New Hampshire Division of Public Health Services for almost two years and recently earned her MS in Homeland Security and Emergency Management. With a background in education and training, she works full time as an academic detailer all over the state. In her spare time she enjoys directing community theatre productions, running and hiking. She is married to Scott and mom to two grown sons. An interview with Kristefer Stojanovski, MPH, PhD(c), Public Health Researcher and Evaluation Specialist, Capacity Building Assistance Program, San Francisco Department of Public Health by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Data, Evaluation, HIV/AIDS, PrEP, Sexual Health NaRCAD: Hi, Kristefer! Thanks for taking the time to chat with us today. Can you tell us a bit about your background and the work you’re currently doing as it relates to academic detailing?  Kristefer: Thanks for having me. I’m a public health researcher and an evaluation specialist with the Capacity Building Assistance Program at San Francisco Department of Public Health. I serve as a specialist and a technical assistance provider for the West region of the United States. My work is focused on data and evaluation of academic detailing programs that are working on topics like sexual health, HIV, and PrEP. My main goal is to help folks measure, or think about, what “success” may look like for an academic detailing program. NaRCAD: What data do you think is most important for academic detailers to track during their visits when measuring or thinking about success? Kristefer: I see evaluation data and detailing efforts as one complete package. Detailers should think about their data at a high level and focus on the information they’re collecting and how that information serves the overall goal of detailing, which is to improve knowledge, attitudes, intentions, and behaviors of providers and clinics. At the same time, detailers should think about how they can show that they’re achieving that goal. For example, it’s useful to track how many providers they’ve seen, how much time was spent with providers, what they talked about during the visit, the resources that were provided, how the providers plan to use those resources, if a follow-up visit was scheduled, and the purpose of that follow-up visit. It’s important to track a mix of quantitative and qualitative data, but the critical components that should be tracked are the outcomes and the process of detailing. NaRCAD: What about academic detailing programs? What data should they collect?  Kristefer: In a typical detailing program, detailers have a longitudinal, continuous outreach to providers. There’s an interesting conversation to be had about how we can use that temporal matrix as a tool and strategy for evaluation. I’m interested in how we can use the work academic detailers are doing – the actual visits themselves - as pieces of data over time. For example, if detailers are collecting some of the rich conversation that they’re having with providers or clinics, it’s fascinating to track those conversations over time and see how the detailing program is changing the knowledge, attitudes, intentions, and behaviors of those providers and clinics. There’s a lot of work that detailers are already doing that can be easily turned into data sources for both the detailing effort and the evaluation effort. I like to think about how we can make things as simple as possible. NaRCAD: Is there a specific platform that makes things simple and is best for collecting data for academic detailers and programs? Kristefer: That certainly becomes a little bit more individualistic when thinking about the needs, challenges, and abilities of each jurisdiction. Detailing is a conversational effort that is attempting to make concrete behavior change, so it becomes more convoluted when you think about how to track a conversation. Some jurisdictions might have a place to track conversations in their electronic health record, where others may not. At the most basic level, detailers can chart their conversations on one-page Word documents. The detailers I worked with charted their conversations with providers over time and eventually put it in one large PDF that could be easily uploaded into a qualitative data analysis software. You have to be creative when it comes to tracking this information. NaRCAD: How would you recommend that programs with limited resources go about data collection and evaluation?  Kristefer: A lot of times we say we want to have high-tech solutions when we don’t actually need them. For a resource constrained department, having that one-page Word document that allows detailers to chart their interactions is more than enough data. Charting for just five minutes after a detailing visit about everything that took place becomes a wealth of information. You can also use an Excel document to input data from provider surveys. There are many low-tech ways to track information and it’s important to be aware of the low hanging fruit in terms of data collection. You want to be able to easily collect data that serves the detailing efforts, the program, and the evaluation and improvement process. NaRCAD: That’s a great way to look at it. What are some best practices for using data for leadership buy-in? Kristefer: I can’t stress enough how important data is in getting leadership buy-in. Data is not only quantitative and qualitative, but also using the information gathered to tell a story. It would be a strong statement if someone was able to go to leadership with a story about how providers have changed their practices based on the detailing effort. Using concrete results and showing leadership that detailing is making a change is extremely helpful for buy-in. Being able to show crazy big outcomes with your data won’t happen, but sharing stories from providers and clinics about how detailing has helped them is quite moving. I’ve heard some amazing stories during my evaluation. For example, detailers helped providers at some clinics to provide patients with directly observed therapy for PrEP at the same time that they were providing them with medication-assisted treatment for opioid use disorder. It’s impressive that detailing at those sites was able to make the clinics think creatively and be able to provide PrEP to these patients. NaRCAD: That certainly is impressive! What has surprised you the most about the academic detailing data you’ve evaluated?  Kristefer: I can’t help but to think that pharmaceutical companies spend millions of dollars and resources on this model and they certainly wouldn’t have been doing this for decades if it didn’t work. We’re almost a little late to the game as public health practitioners, but through my experience evaluating some of this work and reading other evaluations, I’ve been shocked by how much providers truly value detailers. It’s fascinating to see how these health systems and departments are viewed as trusted partners by providers and clinics and how detailing has served as a role to improve that partnership and collaboration. Providers have often said how crucial this information has been in getting access to Department of Public Health resources they didn’t even know existed, which is pretty sad. Seeing public health and the medical system working side by side in this kind of way has been breathtaking.  Biography. Kristefer Stojanovski is a PhD Candidate in the Department of Health Behavior & Health Education, School of Public Health at the University of Michigan. Kristefer has been doing community-based mixed methods research since 2010. His research explores the social and structural determinants to sexual health and HIV outcomes among key populations in the U.S. and in Southeastern Europe. Kristefer’s work interrogates how stigma drives HIV risk and infection using complex systems theory, structural equation, agent-based and multilevel modeling. Kristefer also translates his research into policy and decision-making. He is an evaluation specialist with the Capacity Building Assistance program with the San Francisco Department of Public Health. An interview with Brandon Mizroch, MD, MBBS, Provider Network Supervisor, Louisiana Department of Health by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Hepatitis C, HIV/AIDS, PrEP, Rural AD Programs, Sexual Health, Stigma, Training  Dr. Mizroch participating in a NaRCAD training Dr. Mizroch participating in a NaRCAD training NaRCAD: Thanks for chatting with us today, Brandon! We’re excited to be catching up with you. Can you tell us about your program at the Louisiana Department of Health and the work you’re currently doing? Brandon: Absolutely. I was hired to do work around PrEP and PEP, detailing providers across the state of Louisiana, in 2017. Since then, my role has expanded and I promote education for providers about syphilis, congenital syphilis, and Hepatitis C. Our department now has 3 detailers, including myself. Louisiana became the first state in the country to undergo an incredibly revolutionary Hepatitis C Elimination Plan, which has caused my detailing focus to shift. There’s been huge advancements in the drugs that treat Hepatitis C, but they’ve been inaccessible to much of the population due to cost. We negotiated a fixed rate price for Hepatitis C treatment and can now treat 100% of the population, compared to the 3% of the population we could treat previously. There’s been a big push to identify and train providers who’ve never previously treated patients with Hepatitis C. I’ve been leading the charge by getting the word out, running symposiums, and working with the marketing team that’s creating our statewide campaign.  NaRCAD: Wow, that sounds like innovative and exciting work. Can you explain your program’s approach a bit more? Brandon: I try to blend a few different approaches together. I attended the NaRCAD training during my first year as a detailer. NaRCAD built the foundation of detailing for me. I always use the NaRCAD methodology to get my foot in the door and identify providers who can be champions within their practices. I find it much easier to follow up and do longer didactic sessions about complex clinical topics when I use the techniques of academic detailing during my first face-to-face visits with providers. I connect with about 20 providers in this 1:1 model each month. I also work with residency programs, hospital systems, and present at Grand Rounds to expand my reach. There’ve even been instances where I’ve attended dinners for physicians that are hosted by pharmaceutical companies to network and identify new clinics that would benefit from detailing. NaRCAD: We’re happy to see that you’re blending academic detailing with other approaches. Do you provide follow-up to providers after your visits? Brandon: Follow-up is incredibly important, no matter what approach is being used. I like to send an email after each visit that includes digital resources for both providers and patients. I also offer providers the ability to call, text, or email me because of the apprehension that exists around topics where the knowledge base is still growing. Maintaining relationships with providers also ensures that we have a strong provider network that we can continue to educate on other clinical topics down the road.  NaRCAD: Building a connection with providers is imperative, especially as you move into different clinical topics. Your program spans the entire state. Do you find that there’s a difference when you provide clinical outreach education in rural vs. urban communities? Brandon: Yes, there’s certainly a difference. The providers in urban areas tend to have a higher knowledge base when it comes to PrEP and syphilis, perhaps due to marketing efforts or higher patient loads. This makes starting the conversation a bit easier. Additionally, urban communities have access to navigators, who help with non-medical aspects, like transportation issues, lack of health insurance, and long commute times that all prevent folks from getting the treatment they need. Providers in urban areas are also busier and easily distracted during 1:1 visits, which can make detailing a bit difficult. On the other hand, rural communities are quite the opposite. Providers tend to have more time in their schedules and are excited to sit down with somebody from the state office. They’re eager to learn, but there’s typically less of a knowledge base, making it slightly more difficult to start the conversation. I’ve also learned about patient barriers as well, which affect access and provider care. Patients in rural areas are often friends or family with those throughout the community, including those who work at clinics. The notion that you would know the receptionist or provider at a clinic is enough to deter folks from seeking medical care around a topic like sexual health. To encourage access, our state has created a TelePrEP program that offers PrEP services to anyone via telemedicine. Consultations take place over the phone, labs are obtained at third party lab companies, and medications are mailed right to the front doors of patients. It was originally created to help folks in rural communities who face stigma-related barriers, but we’ve expanded the program across the entire state of Louisiana. It’s a great referral service that I can share with providers.  NaRCAD: It’s wonderful that you’re able to identify these challenges and have resources and tools to address them. What’s one piece of advice you’d give to folks who are detailing on a similar clinical topic or have a large geographical region to cover? Brandon: It’s important to have several different ways of presenting information to the providers you’re detailing and to use varied approaches depending on the barrier(s) they’re facing. I typically focus on emotional connection, financial concerns, and the evidence and science behind the key messages I’m delivering. I’m also ready for provider resistance, and am prepared to address it, which is something I learned from NaRCAD. When it comes to detailing over a large and diverse geography, it’s always necessary to plan ahead. My general rule of thumb is that however many hours it takes to drive to a location, that’s how many providers I want to meet with while I’m there. I typically try to use larger educational events, like meetings with clinics over lunch, as my anchor point for longer trips. After I have that scheduled, I search for smaller clinics around the area where I can meet with providers 1:1. It’s all about maximizing your time.  Biography. Brandon Mizroch received his MD/MBBS from the University of Queensland/Ochsner Clinical School Program in November of 2016. Since taking over as the PEP/PrEP Provider Outreach Specialist at the Louisiana Department of Health in August, 2017, he has worked with hundreds of doctors statewide on HIV prevention best practice. Since then he has expanded his educational base and now serves as the head of the academic detailing department at the Louisiana Department of Health, Office of Public Health, STD/HIV/Hepatitis program. As the Provider Network Supervisor he has helped lead the provider Outreach for the state’s first-in-the-nation Hepatitis C Elimination program. From grand rounds presentations at LSU-Shreveport Hospital and Baton Rouge General, to state-wide symposia and conferences, to one-on-one counseling encounters at dozens of clinics all over Louisiana, he has helped spread awareness and education on HIV prevention, syphilis screening and treatment, and HCV screening and treatment through evidence-based care. Featuring: Mary Nagy, MPH, RN/BSN, Public Health Detailer, HIV Care & Prevention Unit, Michigan Department of Health and Human Services, NaRCAD Training Alumnus Tags: Detailing Visits, Health Disparities, HIV/AIDS, Sexual Health, Stigma  NaRCAD: Thanks for joining us, Mary! You’re a Public Health Detailer in the HIV Care & Prevention Unit at the Michigan Department of Health & Human Services. Before we talk about how you got into your current role, can you tell us what you were doing before that? Mary Nagy: I was an ER nurse for five years. During that time I worked all over the country in lots of different settings, but I noticed the same patterns playing out no matter what city I was in. I was seeing patients daily who were either in the last hours of their lives or needing immediate life-saving interventions as a result of medical problems that might have been avoided entirely through basic services or preventative medicine. The longer I worked ER, the more clearly I saw the effect of systemic forces and environment on health, their unequal distribution across society, and the more I wanted to find a way to work towards health equity. I decided to study public health, and earned my master’s degree in Environmental Health Science at the University of Michigan. In addition to giving me the opportunity to design and carry out my own research, the program I did had a strong health policy component, which helped me add to the understanding of healthcare delivery I formed during the time I spent at the bedside. 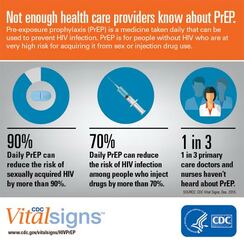 NaRCAD: Tell us what interested you about your current position and what a “day in the life” of a detailer looks like for you. Mary Nagy: I saw the job posted and was immediately interested in it because I think detailing, especially on the topic of pre-exposure prophylaxis (PrEP), is a really effective way to strengthen prevention infrastructure and affect health outcomes. Clinicians are under a lot of pressure and I was drawn to the idea of being a source of relevant, high quality, trusted information. The detailing program here in Michigan is comparatively young and its development is ongoing. Fortunately for me, lots of folks have been willing to help! I've drawn from a broad range of sources has been really helpful during detailing visits, because the needs of providers are so diverse; folks are asking about billing and coding for PrEP visits, standing orders, HIV risk assessment, nuts and bolts of services offered by our state lab, STI screening and trends, and financial supports for PrEP, best practices with PrEP initiation and follow up, and more. I’ve been working hard to broaden my knowledge base, but also to identify resources for questions I don’t know the answers to and topics I’m weaker on.  Image from UNAIDS Image from UNAIDS NaRCAD: Why are you passionate about HIV prevention, and why is academic detailing for HIV prevention so important? Mary Nagy: Even though I’m very new to the field, I think it’s a very exciting time to be doing this work because I do believe it is possible to end the HIV epidemic in the US within the next few decades. Racial and ethnic minorities continue to be underrepresented in PrEP utilization and overrepresented in new HIV diagnoses, and I want my work to contribute to correcting this. I think PrEP can be a tool for health justice and being part of that is valuable to me.  NaRCAD: You’ve mentioned environment a couple of times. Can you tell us how environment is connected to HIV contraction and prevention, if at all? Mary Nagy: I think that’s where my mind goes, because I’ve seen the powerful effect of environment on health, and this is certainly true on a population level. I never want to diminish the power and agency of individuals, but everyone operates under multiple layers of forces. Examples of this include policy, especially the persistent legacy of overtly racist housing policies; the “war on drugs” and resulting mass incarceration; or a justice system that data shows us doesn’t work in the same ways for everyone. These systemic forces, applied to millions of people over many decades, result in the disparities we see in HIV rates, overall health, wealth, and many other areas. Increasing access to PrEP means we can mitigate some risk for folks who might have more exposure due to the environmental context in which they live. For Michigan, one of the ways detailing can help make PrEP easier to access is increasing geographic availability. A large portion of our state is rural, and many counties do not currently have a known PrEP provider. Another challenge is, of course, cost. The cost of PrEP and associated visits and screening tests is a policy issue, and while we hope and expect to see cost come down in the future, in the current landscape, it's important to prioritize educating providers and their staff on available financial supports and how to apply them, so cost doesn’t keep people who can benefit from PrEP from getting and maintaining access.  Image: University of New Mexico Image: University of New Mexico NaRCAD: In addition to geography and coverage, what are some other barriers you’ve encountered when doing academic detailing for HIV prevention? Mary Nagy: Stigma around HIV and other STIs is a big issue. We know that when providers talk openly with patients about their sexual health, they’re better able to accurately assess risk for HIV and STIs and screen and treat appropriately, but those conversations are not happening with enough regularity. Rates of STIs like gonorrhea, chlamydia, and syphilis have been rising, and continue to increase, so there's a lot of opportunity there. NaRCAD: How has detailing been received overall? Are providers open to education on PrEP? When I think about why detailing is important and why I’m doing it, the first thing that comes to mind is a recent survey of primary care providers MDHHS carried out in Southeast Michigan. Providers were asked which supports would best help them to incorporate PrEP into their practice, and "education" was by far the most frequent answer. In addition to the research I’ve seen indicating detailing is an effective intervention to change provider behavior, it's clear that the providers themselves agree that education is important. If we can work with providers to make PrEP available and easy to initiate and maintain, the protection it offers from HIV can improve health outcomes for patients at high risk.  Biography Mary Nagy, MPH, RN/BSN Public Health Detailer, HIV Care & Prevention Unit Michigan Department of Health and Human Services Mary is the public health detailer for the State of Michigan and conducts direct outreach with medical providers to support HIV prevention strategies and stigma reduction statewide. She received her master’s degree in Environmental Health Science from the University of Michigan School of Public Health where as a Graham Sustainability Fellow her research focused on municipal water quality and affordability. Mary also has several years of experience working in as an Emergency Department RN in trauma centers across the US and her work in health equity is informed by her time as a frontline health worker. 'Guest Blog | Alyson Decker, NP, MPH | San Francisco Department of Public Health Tags: Detailing Visits, HIV/AIDS, PrEP, Sexual Health  Our AD program is part of a 3-year demonstration project (CDC Project PrIDE), and as part of our grant-funded work our overarching goal is increasing PrEP access and prescribing to MSM (men who have sex with men) of color and transgender persons who are at substantial risk of acquiring HIV. Our goals include improving sexual health in the primary care setting, refining sexual health history-taking, increasing screening and testing for those with risks, promoting best practices around PrEP prescribing, and helping to establish relationships between our health department and our community providers.  The added benefit of public health detailing is that it also increases awareness about the issues that affect our community. I have been inviting clinicians that I meet to join us in our city-wide Getting to Zero consortium, which helps providers feel that they are part of this important movement of preventing HIV transmissions, deaths, and stigma.  In San Francisco, there is a need for urgency around this issue, especially because it’s become evident that as HIV transmissions continue to decrease, the disparities among new HIV positive diagnoses become more apparent. Many of these disparities are among communities who still may not be aware of PrEP, or are facing barriers to access. Our academic detailing program strives to reach the providers who work with these vulnerable communities.  When kicking off an intervention such as this, identifying the clinicians who see this target population is the first step. To do this, we used STD surveillance data to determine which providers and clinics were diagnosing syphilis and rectal gonorrhea and chlamydia, which are associated with an increased risk for HIV. However, since many providers are not performing appropriate screenings, we also reached out to clinics known to serve our priority population and those located in neighborhoods with the highest HIV incidences.  The next step is how to “get in the door” with these clinicians, which means finding a way to secure a 1:1 visit. I’ve found that initial non-responsiveness isn’t the end of the world—persistence pays off, so keep trying to get in the door, or find an entry point through other community contacts. Sometimes, choosing a different access point can really work well to start a relationship. There are many places where 1:1 visits aren’t feasible due to clinic structure or culture. If I’m able to detail to a small group, it can be a way to meet with a few providers and gain insight about how PrEP might be incorporated or enhanced in their setting. Being invited to an all-staff meeting is often an excellent way to kick off an introduction to this important intervention, and can result in follow-up conversations with individual clinicians. One benefit of meeting in small groups is that if a clinician hears a fellow clinician say that he or she is already prescribing PrEP, there may be more openness to discussing the topic; other providers might feel comforted in having a PrEP "ally", resulting in buy-in from the clinic overall. Some clinicians may think that this type of intervention isn’t relevant to their patient population; as I detailer, I often hear responses such as, “I don’t see this population reflected in my practice,” or “My patients don’t have this risk,”, even if it’s been proven that these clinics do, indeed, serve priority populations. In order to talk about PrEP, you first have to talk about risks for HIV, which often means talking about sex. I think there can be discomfort on both the patient and provider side, and sex is often still a stigmatized topic. There are also overarching resource barriers, including the fact that clinicians are extremely busy and have to address competing health needs in the primary care setting.  While a small pool of clinicians have minimal understanding of PrEP, and require a basic overview about elements like identifying potential PrEP candidates, how to take a good sexual history, and how to bring up PrEP in an appointment, I’ve found that many clinicians are aware to some extent about PrEP already, and are interested in next-level details about how to implement it. This might include what kind of testing is recommended, how to increase number of basic screens, and increasing their knowledge about comprehensive health. There are also providers who are very advanced in their knowledge of what options are available to populations with risks for HIV. This is where the academic detailing becomes more intricate; some providers are seeing lots of patients with risk factors, and may have been prescribing PrEP already. In a scenario such as this, my messaging focuses more on how to support clinicians in ensuring consistent follow-up with their patients, or in how to deal with multiple risk factors, such as when high-risk sexual behavior may overlap with instances of substance use or homelessness. For those who are just getting started, it may help to know that even after meeting with 300 providers, I still get nervous each time I prepare to detail, especially if I’m unfamiliar with a practice. Regardless of the nature of my visits, I walk away feeling that I’ve accomplished something if I’ve answered only one question that’s helped the clinician with his or her practice. And I’ve found that in most cases, the people I meet with are very thankful for this service, and are appreciative of the health department. I always thank providers for the work they do and remind them what an important role they have in the community.  Biography. Alyson Decker, NP, MPH Alyson Decker is a Clinical Prevention Consultant and nurse practitioner with Disease Prevention & Control at the San Francisco Department of Public Health. As the branch’s lead academic detailer, she helped develop San Francisco’s first HIV pre-exposure prophylaxis (PrEP) detailing program. Her role consists of detailing with community providers to increase PrEP prescribing in the primary care setting and promote best prescribing practices. In addition, she provides training assistance to healthcare providers and frontline staff around improving sexual healthcare and STD testing and treatment. She also sees patients at the municipal sexual health clinic, San Francisco City Clinic. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|
