|
Overview: Loren Regier, a NaRCAD Expert Training Facilitator, joins us to reflect on nearly 25 years of his AD career, his experiences in learning AD for the first time, and his role in being a mentor to a new generation of academic detailers. Loren is a hospital pharmacist by training and has served with the RxFiles Academic Detailing Program and the Centre for Effective Practice, both longstanding Canadian AD programs. by Winnie Ho, Program Coordinator Tags: Detailing Visits, International, Program Management, Sustainability, Training  Winnie: We’re delighted to hear more about your AD journey, especially about the ways in which you continue to be a leader and supporter of the AD journeys of many others. Can you tell us a little bit about how you got started in this field? Loren: I was a hospital pharmacist doing a lot of work related to clinical decision-making, public speaking, and education. The Director for our Saskatoon Health Region (SK, Canada) had come across academic detailing from a colleague in Vancouver, and was interested in piloting something similar to what is now the British Columbia Provincial AD (BC PAD) Service. Our region needed someone who would take on this project and build something from scratch. Only partly knowing what I was in for, I said “yes”. To train and learn more, I had the chance to shadow Terryn Naumann in June of 1997. Terryn was the pioneering solo detailer in North/West Vancouver. What was initially a 1-year project for us, became a 2-year, and then a 3-year project, eventually morphing into an ongoing AD service that expanded to cover our province of Saskatchewan.  W: That’s incredibly fortuitous that you had Terryn to turn to for help! We’ve gotten to interview her before at DETAILS and know that she was a trailblazer for AD across Canada. Before I ask you about your experiences now as a mentor to others, I would love your reflections on your experiences as a mentee back in the days when you were learning AD as a new trainee with Terryn as your guide. L: There are both good days and difficult days to think back to – it involved a lot of hard work, but I was fortunate to have an awesome mandate and the opportunity to see another successful service in operation. Most importantly, I was able to see what a successful visit looked like. I joined Terryn for 7 visits over 2 days. After each visit, we reflected on how the visit went, what we liked, and if there was anything one might handle differently. The opportunity to shadow Terryn instilled in me the vision that academic detailing was about both relationship and service, and that clinicians could find both aspects valuable and enjoyable.  W: We do encourage a lot of new people starting AD for the first time to try and find someone to tag along with. You were especially lucky with Terryn because she had had a few years to build up her network and relationships in her community. L: Relationships are key in AD – and witnessing those relationships and the resulting AD conversations – was educational and inspiring. W: Is there a particularly strong piece of advice or a mentorship experience that sticks with you to this day? L: One of the things I recall is that she said, “One day, when you have a tough visit, I want you to call me, because I’m one of the only people who will understand what you’re going through.” Well, the day came when I had to call Terryn and we were able to debrief on a challenge I had faced. That was a critical moment that served to propel me forward with greater insight and confidence.  W: You bring up something important – our work is focused on creating safe learning spaces for providers in order to enact change. What we’ve been able to expand on are the connections between individual members of the detailing community. Luckily, the field has grown and new detailers have many more role models and teachers to learn from. Let’s also talk about this vulnerable moment, because it requires a lot of trust to go to someone when something goes wrong.  L: The mentorship process ideally involves deep, authentic discussions about being a detailer. Being a detailer involves constantly putting your best self forward. Trust allowed both of us to open up to each other with lots of safe space to discuss our different approaches and experiences. Trust is essential for effectively exploring differences of opinion, and how to turn challenges into opportunities. Without it, you don’t get to understand where someone is coming from or to truly grow and learn. In addition, I need to mention Frank May who also became valued mentor over the years. Frank helped pioneer academic detailing in Australia. His thoughtful conversations and leadership were instrumental in my growth in AD, as well as my eventual role in helping train and mentor new detailers.  W: I have definitely seen the large and small ways that mentorship has propagated through the AD community. In the process of learning and educating others in this field, we never truly stop being mentors or mentees – it’s not a binary. It’s a great lifelong process. Let’s flash forward to now: given your experiences, how have you continued to integrate mentorship into your current work? L: A big part of my role these days has been training, mentoring, and supporting others - both academic detailers and those who are moving into program leadership. It’s important to recognize that the world needs more people to do this kind of work and that we need to pass the baton. That involves coming alongside their journey, having good discussions, and being able to dig deep into those critical ingredients for success.  It has meant being transparent about my decisions and leadership so that my team can not only see how I’m thinking and processing things, but also provide their own input and ideas. Being a mentor to me means modeling the approach of learning together and working enthusiastically and collaboratively when pursuing opportunities. W: You’re in a capacity now where you’re training future leaders in AD. You provide an important link and opportunity to reflect on where AD has been, but also the space to give new AD folks a chance to figure out where AD may go next. The people you mentor now will likely go on to mentor others, just as Terryn and Frank did for you. What advice would you give to those who are seeking to be strong mentors?  L: People can sense if they are respected and valued. If they know you care and are interested in their growth, they will open up, share the important stuff, and work together to address the challenges of academic detailing. If you add some fun and enjoyment along the way, the process serves as a model of what will eventually happen between the detailer and those they detail. W: That’s wonderful advice, because one of the best things you can do for someone who is learning is to fully believe in their potential and strengths. They’re already a part of your team – they’re there for a reason.  L: Somebody once asked the coach for Bobby Orr, one of the greatest Canadian Hockey players of all time, “How do you coach Bobby Orr?” and the reply was, “You don’t coach Bobby Orr, you give him room to play the game.” There’s some truth in applying that to leadership and in AD. You need to appreciate where your team members excel and empower them. It means coming alongside, supporting their input, and also giving them the freedom to make their own mistakes and learn from them. Give people the support they need to do best. They’ll show you what they’re capable of. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  LoLoren Regier is a Pharmacist and Consultant Editor with RxFiles Academic Detailing Service in Saskatoon, SK, Canada. Loren has guided the development of this provincial academic detailing service since the first “ground breaking” pilot project began in 1997. Loren is active as a member of the Canadian Academic Detailing Collaboration and provides training and consultation to various programs and initiatives. Loren’s interests cover the practical application of evidence to practice and the ongoing development of multifaceted interventions that support academic detailing. Additionally, Loren serves as a faculty facilitator for NaRCAD’s Academic Detailing Techniques trainings. Loren is co-editor of the RxFiles Drug Comparison Charts – 10th Edition and a contributor/reviewer for Geri-RxFiles and the RxFiles – Bringing Evidence to Practicesection of Canadian Family Physician journal. Loren obtained his degree from the University of Saskatchewan, College of Pharmacy in 1988 which he followed with a hospital pharmacy residency. He serves as a lecturer, instructor and preceptor in the areas of evidence informed drug therapy decision making, educational outreach and chronic pain management in a wide variety of professional settings Overview: Harald Langaas speaks with NaRCAD about his experiences in co-founding Norway’s first national AD program, KUPP. KUPP, which loosely stands for “Knowledge-Based Updating Visits” in Norwegian, has been actively serving Norwegian General Practitioners (GPs) for several years. by: Winnie Ho, Program Coordinator Tags: Chronic Illness, Detailing Visits, Evaluation, International, Program Management  Winnie: Hi Harald, thank you for joining us all the way from Norway to talk about KUPP, the Norwegian Academic Detailing program! Can you tell us a little bit more about yourself and the work that KUPP does? Harald: I’m a pharmacist by training, with experience in working at hospital pharmacies and as a pharmacy manager in the private sector. My interest has always been in how to better provide independent information about the use of medicines to healthcare professionals to improve the quality of healthcare. I work for one of the four Regional Medicines Informational Centers in Norway, one for each of the four health regions. The Norwegian AD Program is strongly connected with those Centers, so my position is split between the regional center and as Director of KUPP, which operates at the national level. KUPP is a small organization – it’s myself and a consultant in clinical pharmacology handling the administration of AD.  W: I can absolutely see why AD fits a lot of your interests! Let’s talk about how KUPP got its start. You were part of the founding of a brand new AD program. What was that like, and what did you learn? H: My colleague Roar Dyrkorn had visited Australia, met the NaRCAD team in Boston, and was very inspired by AD. He saw it as an opportunity to improve the quality of prescribing in primary care and began lobbying to acquire funding for an AD program. Our first campaign in 2015 was put together within a month or two, focusing on NSAIDs (Non-steroidal anti-inflammatory drugs) for GPs. We were extremely fortunate to have Debra Rowett from Australia, who has been pioneering AD in Adelaide for many years, fly out to train our first detailers because we were still novices to this work. This campaign went quickly – maybe too quickly -- but we were able to implement it well, and we had success with the campaign. We’ve been continuing to detail ever since.  W: You also mentioned that Norway is divided into four health regions. Can you tell us a little bit more about these regions and the communities that you serve in each? H: The four jurisdictions, all funded and overseen by the government, are responsible for hospital services in that region. However, primary care services are overseen at the national level. In each region, KUPP has between 5-10 people that are trained as detailers and conduct visits in addition to working at the Regional Medicines Information Centers or at a Clinical Pharmacology department at a hospital. W: On average, how many clinicians does KUPP work with per year? H: There are about 5,000 total GPs in Norway, and we visit between 1,000-1,200 GPs a year, which is about 20%. We have limited resources while trying to reach as many providers as we can nationally. For the funding we have, we’re happy with our work, but of course, we are ambitious! We want to be able to visit everybody.  W: That’s a pretty sizable population that you reach, especially on limited resources! Can you provide some context about Norway’s healthcare system that help us better understand the context in which KUPP operates? H: In Norway, we have universal healthcare, which is fully funded by the government. It means that our healthcare system is quite homogenous across the country. The GPs that we focus on are mostly self-employed, but fully funded by the government. This does mean that when we make arrangements to schedule detailing visits, we have to contact GPs one at a time. They have no financial incentive to see us, and since we take up their time instead of them seeing a patient, they actually lose money by seeing us. This means that we have to ensure that a visit from us is useful and that it’s a valuable investment towards improving the treatment of their patients. We keep all visits to 30 minutes or less. Another important thing to mention is that patients are designated to their GPs. You can’t shop around for providers, so you have to see the same one each time or apply to change to another one. This means that a GP follows their patients for a long period of time, and have a lot of history with their patients.  W: That’s useful background information to know about. Since patients often stay with the same and only GP, how does that impact a GP’s insight into their patient population? H: Because of the long shared history, it means that when we are talking with clinicians, they know their patient pool very well. Even when a GP has taken over a practice, they will be very knowledgeable about who they are serving. W: I imagine that when detailing on chronic conditions, this is an advantage because a GP and a detailer can follow a patient population over time and offer continuous support! Now, we’ve been able to follow KUPP’s work for a while, especially with a lot of your recent presentations and research. How are things going with research and evaluation lately? H: It’s always been useful for us to evaluate and publish our results, especially when we approach the government for more funding. While we can’t do every campaign as a research project, I’ve been working on evaluating a campaign we did on diabetes and also a study on the impact of group visits vs. 1:1 detailing. We’re also working on a small qualitative evaluation of our virtual visits at the moment. It’s been exciting to be contacted by other research groups who want to work with us. It’s really inspiring for us to know there are groups who want to learn more about AD because of us, and that we’re being noticed and seen as a good research partner.  W: It’s always exciting to see where AD travels and how many borders it can cross. We always learn more because the AD community is constantly growing and innovating. As someone who has been at the forefront of establishing AD abroad, what are your hopes for the international AD community at large? H: I would sure hope to see more AD programs emerging in Europe. It would be very helpful to fully connect the AD initiatives that are ongoing around us, to build the same kind of network that North America has had between the United States and Canada. W: We hope to see more programs emerge too! Last question – any final words of advice for detailers and programs? H: The main advice would be to not give up. There will be resistance, and you will run into some troubles, but keep on working. If you believe in the method, and you believe in the work you do, it will pay off. The 1:1 approach is something that separates AD from other tactics, and makes it easier for both clinicians and funding organizations to see you as unique. This work is worth it. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Harald Langaas has been the director of a hospital-based medicines information centre (RELIS) in Trondheim, Norway since 2013. Together with colleagues at St. Olavs Hospital he started the first academic detailing program in Norway in 2015, and has been involved in AD work both as administrator and active detailer since then. Since 2018 he has been the director for KUPP – The Norwegian Academic Detailing Program. He is currently working on a PhD based on evaluation of academic detailing. Anna Morgan, MPH, RN, PMP, NaRCAD Program Manager Tags: Conference, COVID-19, Deprescribing, Diabetes, E-Detailing, Elderly Care, Health Disparities, HIV/AIDS, International, Jerry Avorn, Mental Health  Map of where NaRCAD2020 attendees tuned in from Map of where NaRCAD2020 attendees tuned in from Over 240 members of our worldwide community came together to be a part of something special--our 8th annual conference, and our first in a virtual setting. We were able to expand our reach and overcome barriers like travel time and financial constraints that have prevented our colleagues from attending previous conferences. There was a palpable sense of positivity, enthusiasm, and resilience, especially in a virtual space. We’re so proud of evaluations that cited a renewed sense of passion and commitment to AD based on the new lenses we applied to our programming, including comments about feeling “empowered” to continue this work in the year ahead (even amidst inevitable Zoom fatigue.) Check out our highlights and access all event resources below and on the Conference Hub.
 With so many of you expressing a continued need around more of our peer working sessions, we’ll be focusing largely on that in 2021—we can’t wait to support your work this year. In the meantime, tell us what you need to make next year a success. See you in 2021. The NaRCAD Team Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation! Evidence into Value and Action: Reflections on 30 Years of AD in South Australia (Part Two)10/5/2020
An interview with Debra Rowett, BPharm, Adv Prac Pharm, FPS, the Director of the Drug and Therapeutics Information Service (DATIS) in Adelaide, Australia. Debra joins Winnie Ho, NaRCAD Program Coordinator in a two-part conversation about a 30-year career of pioneering academic detailing in Australia and reflects on the past, the present, and the future of the field. In Part Two, we discuss the evolution of academic detailing as the world of healthcare changes. You can read Part One here. Tags: Detailing Visits, Evidence-Based Medicine, International, Medications, Program Management  Winnie: You wear so many hats when it comes to AD. How have those roles changed over your time with DATIS? Debra: Before I was Director of DATIS, my role was primarily around developing our detailing materials, and evaluating the evidence and our program. I was always interested in the synthesis of evidence and turning that into value for clinicians. I was a clinical pharmacist who was working with people across many disciplines, and there was a growing body of evidence, but translating that into practice was always a challenge.  W: I think you touch on a fundamental aspect of AD – that we turn evidence into value, and that we translate all this research into action. It’s very critical that AD continues to provide that independent, trusted, unbiased source of information to ensure evidence is disseminated responsibly and utilized properly. D: I would agree with that, very much. We live in an information-dense era and much of the information is synthesized and aggregated at the population-level, but clinicians are responsible for decisions at the individual patient level. I think AD is about bringing evidence to the point at which clinical decision making is made. W: I’m curious about your experience with evaluating evidence for AD materials. It’s clearly a difficult, but super important aspect of AD. You have all these clinicians who are trying their best to make the best possible decision for their patient – and AD comes in, and in many ways, helps share in that responsibility.  D: Evaluating evidence is also about recognizing what we don’t know in the evidence. When reviewing the evidence for an AD program, we look for where there are gaps in the evidence, where there’s controversies, and differences in opinion about the evidence. No matter how well done, you make choices along that entire process about what to include, what to exclude – and even with the synthesized evidence, there is still human judgement about how to use it. W: Right, and that human judgement also needs to focus on how that evidence came to be and how it was produced. D: Absolutely. As we know evidence-based medicine is not just about the randomized controlled trials and published evidence, it’s about the intersection of published evidence, clinical judgement, and the patient’s specific needs, goals, and circumstances. The real opportunity for AD is that you can personalize this information for the provider to work with.  W: It’s extraordinarily rewarding work, and it’s a constant process in grappling with the things we don’t know. As someone who has been in this work for a long time and has had to adapt a long-standing AD program to changing guidelines and medical evidence, you’ve likely seen some big shifts in the medical consensus. Take opioids for example – the consensus around the safety of its use has had a dramatic change over the years. How have you adapted when the evidence base can sometimes change quickly within a few years? D: It’s important that we come to providers with a balanced view, and that we acknowledge with them that there is uncertainty, that there is complexity, and that it isn’t easy to make these decisions with their patients. There’s a lot of things that we don’t know. If you come with too much certainty, you lose credibility because translating evidence into routine clinical practice is complex. Every time a medicine is prescribed for and used by a patient, we’re forecasting how the future will proceed - the exact benefits and harms that a patient will experience are uncertain.  People are living longer and with multimorbidity which presents new medical challenges. We’re seeing more people living with issues like musculoskeletal problems, hypertension, diabetes, renal problems, atrial fibrillation, and surviving their myocardial infarctions. The number of medications that patients take now compared to 30 years ago have increased. There are individual guidelines for each condition, that don’t necessarily take the other comorbidities into account. The drugs used to treat one issue may lead to treatment conflicts for another condition and needs to be taken into consideration. It’s not just in one area of practice that has changed too, or just our demographics – we’re seeing fewer solo General Practitioners and more team-based practice in Australia. AD needs to take all of that into account when considering how to detail, and also who to detail.  W: Can you explain what you mean by “who to detail”? D: It’s important to understand who the decision-maker is and what the decision you’re trying to address is – for some of our AD programs it might involve other health professionals; it’s not always the doctor. W: Right, and this whole of office approach looks at all the players involved in the continuum of care, and acknowledges that they may play a role in how clinical decisions are ultimately made.  D: Yes, and I think this is why AD is even more important now than it was when we first started. It allows us to bridge individual condition silos, and helps providers navigate multimorbidity. Healthcare is never a one-size fits all, even for an individual. Their circumstances and treatment goals can change over the course of their lives. AD can personalize the information and tailor it to the needs of the clinician. AD can also be the conduit between population level evidence and its translation into clinical decision making - that is one of its greatest strengths. W: NaRCAD has been lucky to see overarching growth of AD programs everywhere, along with all of its exciting new innovations and evolutions. Any final thoughts on AD before we hear from you at our upcoming conference? D: One of the things I try and impart when teaching the method of AD is to value the knowledge of the person you are detailing. There is a lot of listening that occurs in successful AD if you are truly to meet the needs of the provider you are visiting. If you keep at the very heart of what you do, respect for learning together and hold true to the principles of academic detailing, you will meet incredible people everywhere you go. It makes for a wonderful career. (Part Two of Two) Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Debra Rowett, BPharm, Adv Prac Pharm, FPS, has led an academic detailing team for over 20 years and is a member of the team which designed, developed and delivered the “Best Practice in Educational Visiting” training for academic detailers in Australia. Debra has worked closely with NPS Medicinewise since their inception and has provided consultancies to other national and international academic detailing programmes. Debra is an experienced academic detailer with expertise in designing, developing, training, implementing and evaluating academic detailing programmes. Debra has served as the President of the Australian Pharmacy Council and is currently the Vice President of the Council of Pharmacy Schools. Debra has worked extensively in the area of quality use of medicines, inter-professional practice, policy and health workforce development in Australia. Debra is a member of the national Drug Utilisation Sub-Committee of the Australian Pharmaceutical Benefits Advisory Committee (PBAC). An interview with Debra Rowett, BPharm, Adv Prac Pharm, FPS, the Director of the Drug and Therapeutics Information Service (DATIS) in Adelaide, Australia. Debra joins Winnie Ho, NaRCAD Program Coordinator in a two-part conversation about a 30-year career of pioneering academic detailing in Australia and reflects on the past, the present, and the future of the field. In Part One, we introduce you to DATIS and academic detailing in the Australian context. Stay tuned for Part Two! Tags: Data, Evidence-Based Medicine, International, Program Management 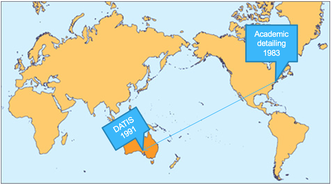 Winnie: We’re so glad to have a chance to chat with you about your long career in AD, Debra! Debra: This is a great part of the job, talking to other people in the AD community. It really is a great privilege to be working with academic detailing organizations in different countries. I’ve loved getting to meet and learn from so many different people. W: I would agree! I’m sure you have some great stories of what it’s like to work internationally in this field. D: One of the things that it has really highlighted is the nuance of language. At a training workshop in the U.S early in my career, I was saying how we would meet with doctors in their "surgery", and how important it was to meet them in their surgeries close to where they make decisions. The workshop participants really politely said to me, but isn’t surgery a really bad time to detail? Oh! Surgery – I meant their office.  W: We really would have quite a different communication model if we had detailers visiting providers mid-surgical operation! This does gives us a good starting point into discussing how Australian AD is unique. Besides the context of the word "surgery", what else would our non-Australian colleagues need to know about Australia to understand the context of what you do with the Drug and Therapeutics Information Service (DATIS)? D: I have been involved with DATIS since its formation in 1991. I was a clinical pharmacist at the Repatriation General Hospital, a teaching hospital, when Jerry Avorn’s paper was published. His work on how AD could influence clinical decision making really resonated with us in Adelaide. One of the big things to know about Australia is that we have a National Medicines Policy, which aims to improve positive health outcomes for all Australians through access to and quality use of medicines. DATIS was one of the first programs funded through the Quality Use of Medicines initiative, and in 1998 NPS MedicineWise (formerly the National Prescribing Service) was funded.  W: Australia is enormous - it must be a challenge to cover. What is the geographical coverage of your AD program? D: South Australia has a population of about 1.4 million people and a vast geographic reach – the furthest of my AD visits is about 800km (500 miles) away from where we are! We work to provide AD to over 85% of all family physicians in South Australia, so about 1,300 General Practitioners (GPs) each year. We provide AD services to aged care, primary care and hospital providers. We also work in partnership with NPS MedicineWise who have implemented AD at the national level. W: That’s certainly an enormous coverage zone, especially for those core 12 people! How has this work manifested in South Australia?  D: At the heart of our program is service, and we build our program to emphasize that. There are three aspects of DATIS: service delivery of detailing visits, training of detailers, and research. We have a core team of 12 people who carry this work out alongside our colleagues who join us for various projects. Because of our multiple different contracts, the clinicians we provide services to can see us for multiple reasons in a year. Between visits, providers will ring us with clinical questions about therapeutic issues that have arisen in their practice. We have also developed interprofessional communication training to support interprofessional practice with a focus on pharmacists and physicians. Our AD programs usually seek to address a therapeutic area or clinical issue however a recent AD program we developed with our hospital pharmacy colleagues was to support pharmacist preceptors implement a performance outcome framework based on entrustable professional activities for interns and undergraduate pharmacy students. W: It's incredible that DATIS has such a focus on this three-pronged approach, because it continues to help push our understanding of best practices in AD through implementation, study, and training others to carry on the work. Can you tell us a little more about the foundation that DATIS is built upon?  D: Behavior change theory and implementation science has informed our work from the outset in 1991, including the development of the training program which was designed in collaboration with psychologists and experienced GP medical educators. Social marketing frameworks, an adult learning approach, the concept of cognitive biases, clinical reasoning all recognize the many interacting and complex influences on behavior. We try to learn from these and apply to the design and implementation of AD. We also use pharmacopidemiology methods to understand evidence to practice gaps and for evaluation. As AD evolves and changes, something I really emphasize is staying true to the principles of AD – this is a rigorous process. W: We’re seeing innovations all over the world and across so many clinical topics. Are there any unique innovations that you feel differentiates Australia AD from other AD programs?  D: One innovation that we're exploring is applying the principles of AD to patient behavior change interventions. As part of person-centered care, it is important for patients to understand their medicines, and to be involved and empowered in shared decision making. We haven’t called this work AD, but have applied the principles of AD in this research. Complex clinical decisions need to be made each and every day by providers, and it's a privilege to be able to bring providers the best available evidence through academic detailing services, part of the power of AD is the adaptability and personalization to providers along the continuum of care. We are seeing the world of healthcare change, and we have so much to learn as it does. (Part One of Two) Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Debra Rowett,BPharm, Adv Prac Pharm, FPS, has led an academic detailing team for over 20 years and is a member of the team which designed, developed and delivered the “Best Practice in Educational Visiting” training for academic detailers in Australia. Debra has worked closely with NPS Medicinewise since their inception and has provided consultancies to other national and international academic detailing programmes. Debra is an experienced academic detailer with expertise in designing, developing, training, implementing and evaluating academic detailing programmes. Debra has served as the President of the Australian Pharmacy Council and is currently the Vice President of the Council of Pharmacy Schools. Debra has worked extensively in the area of quality use of medicines, inter-professional practice, policy and health workforce development in Australia. Debra is a member of the national Drug Utilisation Sub-Committee of the Australian Pharmaceutical Benefits Advisory Committee (PBAC). An interview with Marlys LeBras, PharmD, a clinical pharmacist with RxFiles Academic Detailing Program. by Winnie Ho, Program Coordinator Tags: COVID-19, E-Detailing, International, Program Management  Winnie: Thank you for speaking with us today Marlys! Can you tell us a little bit about your work with the RxFiles Academic Detailing team? Marlys: Absolutely! I’ve been with RxFiles for just over 4 years as an Information Support Pharmacist doing both frontline academic detailing as well as co-leading various academic detailing training sessions, with the most recent being this past April. Our program covers Saskatchewan, Canada, but our website, app, and book are used outside of the province and Canada as well.  W: RxFiles is definitely one of the larger and more established programs we’ve had the honor of partnering with through the years. Can you tell me how maintaining the daily operations of your program have been impacted by COVID-19? M: One of the bigger things that’s changed for our team has been moving our academic detailing training sessions online for our team of 12 detailers. We had to shorten our two-day in-person training, and shifted to hosting shorter sessions and offering more pre-training day and post-training day webinars to cover all of the content, including “how-to virtually detail”.  W: No matter how well virtual substitutions are planned, it’s not the same as being together. We’re all really missing our colleagues, and it’s heightening a sense of isolation. How do you think your team has adjusted to moving the training online? M: I think our team adjusted quite well to the training adaptations. We were able to give them enough notice about the shift. What came out from training days is that our team members really do miss being in-person and having that social interaction – even the chit-chat in between sessions. For in-person trainings, we typically have time for a team-building activity in the evening where people catch up. We’ve been trying to incorporate more games and fun into our virtual training to have that social aspect. Personally, I really miss debriefing with colleagues in-person after detailing visits.  W: It seems like keeping the team connected is a big part of your team culture. How has your team stayed connected through the pandemic? M: We typically do a roundtable at the mid-point of a detailing topic. We typically go around and share a little bit about our detailing experiences. Pre-COVID, no one wanted to turn on their cameras. It was never a requirement, but now everyone is turning them on. It’s been really nice just seeing people’s faces. Also, one of the things that’s been nice about going virtual is that we are able to open up staff meetings and invite more detailers to participate with us. We would have never been able to do that as easily in person.  W: We’ve seen opportunities like these spring up as teams need to be particularly innovative under tough circumstances that prevent in-person connection. Speaking of teams, dream teams don’t come out of nowhere. A lot of work goes into creating and maintaining a strong, positive, and connected team. At NaRCAD, we talk a lot about what makes a good detailer, but what are some of the hallmarks of a strong detailing team? M: Team work is a really interesting thing to dive into. I reflected on this question, and think that a strong detailing team supports one another. That support can be helping each other out in the detailing session itself (e.g. co-detailing), or through communicating with each other about the providers we serve and in between detailing sessions (e.g. a prescriber moved from one detailing area to another). We want the team to be successful in moving towards our goals together. Another thing that COVID brought to my attention is that a strong detailing team also has a positive attitude. I really feel that during our transitions, everyone has been really positive and embraced the changes.  W: You’ve shared a lot of examples of how your team regularly communicates at various points during a detailing campaign, which shows a culture of checking in and making sure no detailer is left out. Can you speak a little about how that culture’s been built up at RxFiles and how you maintain it? M: I think Loren Regier, who is in charge of Projects, Transitions and Training, has been such an asset in the development of our program, has really emphasized checking in. He really showed us the value of that, and not only does he talk about it, he has made it very easy for someone to approach him and talk about how the detail went, both the successes and challenges. W: Having access to mentorship, and making sure a team-based approach is emphasized by leadership is key. It’s clear that the RxFiles team is doing well in adapting to these challenges faced by so many detailing teams. Maintaining positivity and seeing challenges as opportunities for growth is something that’s critical for teams to continue to have an impact. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Marlys LeBras is a clinical pharmacist with the RxFiles Academic Detailing Program at the University of Saskatchewan. She completed her Bachelor of Science in Pharmacy at the University of Saskatchewan, her Hospital Residency with the former Regina Qu’appelle Health Region, and her post-graduate Doctor of Pharmacy (PharmD) degree at the University of British Columbia. An interview with Ramona Shayegani, PharmD, Program Lead, Academic Detailing Service, Veterans Affairs Southern Nevada Healthcare System by Kristina Stefanini, NaRCAD Project Manager Tags: E-Detailing, International, Materials Development, Opioid Safety, Substance Use, Rural AD Programs  Kristina: Programs are transitioning their academic detailing (AD) efforts to e-Detailing or virtual detailing amid the COVID-19 pandemic. As part of your role at the Veterans Health Administration (VHA) Academic Detailing Service, you’ve completed e-Detailing visits, which you presented on at the NaRCAD 2019 conference. I wanted to interview you today, Ramona, to learn more about how you transitioned to e-Detailing. First, how did your program decide to do e-Detailing? Ramona: Thanks for interviewing me! We heard about an e-Detailing pilot project from our national office and we were excited to participate as our region is spread out and rural, covering Nevada, northern California, Hawaii, and Manilla, Philippines. We felt this would be an excellent setting in which to incorporate video calls into our communication with clinicians. As a result, e-Detailing has allowed us to reach our full potential as a service. Kristina: Amplifying a program’s impact and reach through e-Detailing is something many other programs want to experience. Have providers been receptive to e-Detailing visits given the current COVID-19 pandemic? Ramona: I think it varies by site, but for the most part, providers are very eager to learn about the VHA’s telehealth program. Initially, when we started e-Detailing, we launched a campaign to encourage clinicians to complete telehealth visits with patients. Now providers remember our names, and they reach out about setting up telehealth meetings with their patients and figuring out how to conduct video calls. It’s very rare for providers to reach out to academic detailers for help. We usually have to initiate outreach requests. Kristina: That’s terrific that clinicians are the ones reaching out for the service. When you’re getting ready for an e-Detailing visit, do you prepare the same way as you would for an in-person visit? What materials do you use, and how do you use them?  Ramona: The campaigns we’re working now are so fast-paced, so we’re sharing materials via PowerPoint presentations on a video conferencing platform; we also use electronic PDFs. In addition to showing providers electronic materials, you can still model an approach as you would in person by holding up some of the materials on the camera. For example, with naloxone education, we have naloxone spray “dummy” versions that I show providers on video; I ask if they have ever seen what a naloxone spray looks like, and whether they would be interested if I sent a model version, which they usually say yes to. Kristina: That’s something we try and tell detailers who are pivoting to e-Detailing, which is that much of the interactive approach of an in-person visit is still accessible via video! Many detailers who are trying this out for the first time are eager to find ways to build a meaningful, trusting relationship with clinicians--do you have any advice for strong relationship-building approaches during e-Detailing visits?  Ramona: Sometimes, especially if it’s a new provider, I try to remind myself that I might not get to talk about any of the key messages. It’s really important to take that time to introduce yourself and your service. I don’t feel like it’s anything different than meeting someone face-to-face for the first time. However, detailers need some time to try this with each other, their team, or providers that they have a good relationship with. Detailers need to build that confidence before they go out and try these video calls with people they’ve never spoken with. The more I do it, the more confident I feel, which is key in building these relationships. Kristina: That makes sense—it’s about comfort and confidence as much as knowing the evidence. We’ve also encouraged detailers to know that it may take more time to build up to delivering the key messages than you’d like it to, and to be patient and focus on building the relationship when carrying out visits online. In your experience, have you seen any drawbacks to e-Detailing? Ramona: One thing is that detailers don’t have the luxury of getting a feel of what the clinic is like, which would be easy to observe in person. A lot of times when I am in a clinic, I get a chance to talk to an auxiliary support team, or I could just walk to the other room and talk to the nurse. I’ve found ways to adapt to e-Detailing to try and have more of the team’s perspective; I’ll often ask providers if they think it would helpful for the nurse to be on the call so we can have a group discussion. Kristina: It’s really about thinking outside the box and adapting the in-person approach, while trying to maintain connection. Is there anything else you’d like to share from your experiences with implementing e-Detailing? Ramona: Detailers should acknowledge that this is a brand-new approach; you may not feel like this is your preferred way to talk to providers. Remember that it will take some time to get comfortable with it. There’s a learning curve. Now that I use this approach full-time, I just love it, and I don’t want to go back! It’s just as effective, a lot more efficient, and it allows you to be flexible.  Biography. Ramona Shayegani is the program lead for VHA’s Academic Detailing service in northern California, Nevada, Hawaii and Manila. She received her Doctor of Pharmacy degree from Oregon State University in 2014 and has clinical background in mental health and addiction medicine. She was one of the first detailers to pilot e-Detailing at the VA and has completed over 400 virtual detailing visits. Overcoming the Impossible: Pivoting to Meet the Needs of Family Physicians During COVID-196/10/2020
An interview with Lindsay Bevan, MScHQ candidate, Project Manager, Primary Care Academic Detailing Service, Centre for Effective Practice by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: COVID-19, Detailing Visits, E-Detailing, International, Program Management  Anna: Hi Lindsay! Thanks for chatting with us today about the exciting work happening at Centre for Effective Practice (CEP) in Canada. Can you tell us about your role and share some highlights from your team’s recent work? Lindsay: I’m the manager of the primary care academic detailing service at CEP. We have a provincial service, which started in March of 2018 that serves family physicians across Ontario. Prior to our current service, we have run services in long-term care to support appropriate prescribing as well as primary care to support diabetes management. Our current service is still growing, but we’ve served just over 880 family physicians to date. Our focus has mainly been around opioids and chronic pain. We were just about to launch a series of “visits” (campaign topics) on prescribing in older adults, but we quickly pivoted to meet the needs of family physicians and began working on a visit around managing primary care in the COVID-19 context.  Anna: It’s so important to understand and meet the needs of family physicians when it comes to academic detailing, especially during a tremendously stressful time. Can you tell us a little bit more about the COVID-19 visit and the process behind its launch? Lindsay: Our provincial government declared a state of emergency in Ontario on March 17th, so we knew COVID-19 would be top of mind for our physicians and that they’d need more information. We also knew that we’d have to deliver the visits virtually, which was a fairly new territory for us. We had to modify our usual content development and detailer “upskilling” (bringing detailers up to speed on the content, key messages, and evidence around the topic) processes in order to meet the demands of family physicians by getting them information around COVID-19 when they needed it. The content development process for our other visits typically takes six months, with the detailer upskilling taking the last month and a half of that six-month period. COVID-19 turned everything upside down and made us rethink what we assumed was impossible. Within two weeks of the declaration of emergency, we started pulling together content for our COVID-19 resource centre (clinical tool for this visit, which is also available to all primary care providers), one week later we started training our detailers and within a month, we were delivering virtual visits to family physicians.  Anna: It’s impressive how quickly your team was able to launch this visit. COVID-19 is different from other topics that your team has focused on because the information and guidelines are continuously changing. How has your program kept detailers up to date? Lindsay: The detailer upskilling process for other visits includes weekly webinars to review key messages and the surrounding evidence, and a two day in-person workshop where detailers get to practice their visit discussions with each other and family physicians prior to launching visits. We also use a content development team for our detailing tools and bring those tools to the detailers to review when they’re about 90% complete. We typically don’t edit or change those tools after visits have begun. For our COVID-19 visit however, the detailer upskilling weekly webinars and the content development for our ever-evolving online COVID-19 resource centre have been continuous, ongoing processes. Our detailers have also taken on a larger role within both processes. Each detailer has been responsible for searching for, appraising and synthesizing information on a specific sub-topic of COVID-19, and then submitting this information for inclusion in our resource centre as well as presenting it at our weekly webinars to their fellow detailers. Our detailers need to be up-to-date on the emerging and evolving evidence and jurisdictional guidance around COVID-19 because family physicians don’t have time to sort through all the information being made available to them daily during the outbreak. Anna: It’s critical to provide physicians with the most up-to-date information, especially in situations like the COVID-19 pandemic where they’re bombarded with new recommendations and guidelines from multiple sources on a daily basis. How many COVID-related visits has your detailing service provided to physicians during this time? Lindsay: We’ve had 95 initial visits to date and approximately 12% of those visits have been with physicians whom we’ve never detailed before. We’re just starting to reach back out to physicians to see if they would like a follow-up visit since evidence has evolved and challenges have changed since we first started. The initial conversations were focused on testing, assessing and managing patients with the virus, and we’re now seeing those conversations shift to focus on resuming primary care services within the COVID-19 context. The detailers have done an amazing job in transitioning their detailing conversations to ensure they’re always covering the emerging areas of interest and need for family physicians. We’ve seen little to no requests from physicians for detailing visits on anything but COVID-19 or on maintaining care in the context of COVID-19, which speaks to the impact this topic has had on family physicians.  Anna: Wow – it’s amazing that your service has been able to detail so many physicians on COVID-19 while also recruiting new ones. Lindsay: Yes, overall, the visits have been well-received. We were a bit more cautious with our approach to promoting our COVID-19 visit and recruiting new family physicians. We didn’t want to add to the current noise at this time. Instead, we took a more passive but strategic approach, like adding a banner to our website where family physicians can quickly sign up for a visit, and having our partners share our visit and resource centre with their membership base. One of the neat things about this visit is that because we’re offering it virtually, we’re able to expand our geographical reach and provide our detailing service to more physicians.  Anna: Using a virtual platform certainly has its pros, especially within the world of academic detailing! What has your program’s experience been like with integrating e-Detailing into your service? Lindsay: The transition wasn’t unsurmountable for our detailers because they are quick learners, and we’ve had a lot of support through the resources offered by NaRCAD and our partnership with the Canadian Academic Detailing Collaboration (CADC). We also did internal virtual training sessions with our detailers where they were able to practice using all the features of the Zoom videoconferencing platform. Overall, it’s been a positive learning experience, and one that has furthered our team’s ability to be adaptable and enhanced our problem-solving skills. We do feel however that there’s been an impact on the detailer-physician relationship since we’ve transitioned to virtual detailing, especially for the 12% of family physicians who are new to our service. When a detailer is in a physician’s practice, they can see how busy a waiting room is or how stressed the staff appear to be. When family physicians join a virtual detailing visit, it’s much harder to gauge what kind of day they might be having and adjust the discussion accordingly. Furthermore, the act of going into a physician’s practice itself can create goodwill that helps establish and strengthen the detailer-physician relationship, and that opportunity is lost during virtual detailing.  Anna: That’s an excellent point. Observing the waiting room and interacting with office staff is also essential to a detailer’s needs assessment. Detailers lose this piece of a visit when the detailing is done virtually. Is virtual detailing something that CEP will continue doing once COVID-19 related restrictions are lifted? Lindsay: Our detailers and family physicians would like to return to in-person visits. There seems to be some conversations that lend themselves better to virtual communication, and others for which an in-person presence offers greater value and impact. When it comes to relationship building, in-person interactions still offer something special. We would also like to build off the momentum we’ve started with our virtual visits. We’re exploring the idea of offering virtual detailing to family physicians who would otherwise have their visit rescheduled due to extreme weather or to family physicians located where we don’t already have a detailer covering the area. We’ve all done what we thought was impossible in providing the majority of healthcare visits virtually. I hope that folks across the healthcare system will continue to use that momentum moving forward to increase access to care.  Biography. Lindsay Bevan works for the Centre for Effective Practice (CEP) where she collaborates with a team of amazing individuals to develop and implement evidence-based supports and services to help narrow the gap between best evidence and care in Ontario. As a project manager, she oversees the planning and implementation of the CEP’s primary care academic detailing service, which serves family physicians across Ontario. Prior to joining CEP, Lindsay worked at the University Health Network in the infection prevention and control unit, where she updated internal infection control policies and developed patient and provider educational material. Lindsay is currently completing her Master of Science in Healthcare Quality at Queen’s University. An interview with Terryn Naumann BSc(Pharm), PharmD the Director of Academic Detailing and Optimal Use at the British Columbia Ministry of Health by Winnie Ho, NaRCAD Program Coordinator. Overview: Terryn previously spoke about her experiences on a virtual detailing panel at the NaRCAD2019 conference. You can watch the video recording here. Tags: Detailing Visits, E-Detailing, International  NaRCAD: Terryn, thank you so much for speaking with us today about your experiences with detailing in the province of British Columbia. The BC Provincial Academic Detailing (PAD) Service certainly has a lot of ground to cover. Tell us about the program goals and geography. Terryn: For reference, British Columbia is geographically larger than Texas, but the population of British Columbia is only about 5 million people. We provide our detailing services to family practice physicians, nurse practitioners, and a few other healthcare professionals. Our detailers each do more than 175 visits per year, and collectively, they see about 2000 providers per topic, which includes about a third or so, of all the family physicians in BC. We have 12 detailers in total, half of whom are working in less densely populated areas. For example, the northern end of the province is mostly small communities with only 3-4 providers in each town. One year, one of the detailers drove over 17,000 km (10,563mi) for her visits alone!  NaRCAD: That’s an incredible amount of work that your detailers have been up to! And you yourself have been active in AD for a long time. What was your experience then like? Terryn: I started in 1993 with the program that would one day expand to become the PAD service, and I detailed for about 7 years. I came back to academic detailing in 2008 as the coordinator of the provincial program. When I started in 1993, I had just graduated with my PharmD. I had read about AD and was excited to try something new. You have to realize, at the time, technology wasn’t that advanced... I didn’t even have an e-mail address when I first started. You couldn’t just send people a note and say “When would you like to meet?” It wasn’t simple to access people. NaRCAD: How would you describe how AD has changed since you started?  Terryn: When I started, I was the first academic detailer in Canada. There were about 70 physicians that I would go out to visit for each of the topics I put together after having the content reviewed by a local physician specialist from within our own community. One of the things that has changed is the breadth of resources and the growth of the AD community. There are so many more people involved, content is more thoroughly researched, and the literature is more readily accessible through technology. NaRCAD: Technology has certainly changed the way the world works, and it’s something that detailing programs are turning to more and more to tackle the challenges you’ve mentioned, such as trying to serve a large and scattered population with a limited team. We’ve seen the increased use of tele-communications to do detailing. What has your experience been with virtual detailing, also commonly called ‘e-detailing’?  Terryn: One of the things we value about AD is that truly interactive, face-to-face encounter and that ability to individualize sessions to the provider’s learning needs. Virtual detailing uses a different methodology altogether. I think there are advantages to virtual detailing, but sometimes I think that it’s not as simple as moving AD to a web platform. I worry about the personal elements you can lose, even when using a web platform where you can see each other. My detailers often end up making slides of the original materials, which sometimes turns the session into more of a presentation. NaRCAD: Can you elaborate further on the nuances you’ve seen with this new approach? Terryn: We started with something we called Technology-Enabled AD (TEAD) which was a limited study done to compare the efficacy of TEAD versus a traditional face-to-face visit. They found that there was an effective knowledge exchange during both types of sessions, but the time it took for TEAD was far shorter. However, when we added TEAD as an optional feature for our providers, we ran into multiple challenges, such as detailers and providers not being familiar enough with the technology. The large majority of our providers choose to meet in person when they have that option.  That said, virtual detailing has been useful considering BC’s terrain and rough winters. Some regions have winter 8 months of the year and travel is limited for safety reasons. We have used virtual detailing, but find that we need detailers that are tech-savvy and can guide providers through accessing the platform easily. The key is maintaining the interactivity component and having the session not become a presentation. If we can embrace virtual detailing as its own, unique skillset, we may be able to take advantage of all of its benefits. I think that we’re also at a changing point in technology – the next generation of providers (and detailers) will have grown up with and be more comfortable using technology. NaRCAD: There will be a lot of growth in detailing as we are able to incorporate more options into how we reach providers, with the emphasis being on building a strong relationship. Terryn: The goal of AD has always been to have a clinician who values a discussion about the evidence, and then is able to incorporate the evidence into their own practice and drug therapy decision making. E-detailing is just another modality for doing that. We found that virtual detailing is most effective after establishing a prior relationship with the provider during a face-to-face visit. We received fantastic feedback from one provider who felt the virtual detailing session that he participated in from the comfort and privacy of his home allowed him to ask questions he might otherwise have avoided asking in a group setting. If we can use technology to build relationships like that, then ultimately isn’t that what we want? I would say that it is.  Biography. Terryn Naumann is the Director of Academic Detailing and Optimal Use at British Columbia’s Ministry of Health’s Pharmaceutical Services Division. She earned her pharmacy degrees from the University of British Columbia and completed a hospital pharmacy residency at St. Paul’s Hospital in Vancouver. Terryn began her career in academic detailing in 1993 when she worked at Lions Gate Hospital in North Vancouver as the clinical pharmacist for the Community Drug Utilization Program – the first academic detailing program in Canada. Since 2008, Terryn has led BC’s Provincial Academic Detailing (PAD) Service, a team of 12 academic detailing pharmacists who conduct over 2000 academic detailing/small group learning sessions each year. She is a member of the Canadian Academic Detailing Collaboration, having served as chairperson and secretary. She has also been a facilitator at several of the Centre for Effective Practice’s Basic Academic Detailing workshops. An interview with Zack Dumont, BSP, ACPR, MS, a clinical pharmacist with the RxFiles Academic Detailing Service in Regina, Saskatchewan, Canada and a NaRCAD Training Facilitator by Winnie Ho, NaRCAD Program Coordinator Overview: The Cannabis Act went into effect in Canada in October of 2018. The legalization of a drug with strong potential for a myriad of clinical uses was followed by many questions from patients and providers alike about its effectiveness, its safety, and lack of previous research. The RxFiles have carried out a cannabinoid academic detailing campaign to address the demand for truth in a time where research has just begun to shed light on previous myths, misconceptions, and clinical promises. Tags: Health Policy, International, Materials Development, Opioid Safety, Stigma, Substance Use  NaRCAD: Zack, thank you for taking the time to speaking with us today! RxFiles has been around for more than 20 years. What do you do you believe is driving the demand for the resources that academic detailing is providing? Zack: There’s an element of doubt in the information out there, because people have experienced misinformation before. People are often interested in the truth and that’s one of the most amazing things about academic detailing. There is also a desire for practical information that can be used to actually treat patients, and there’s a ton of overlap there. These things are important to these very, very busy providers who want the best for their patients. NaRCAD: We know that your team is working on a cannabinoid campaign, which can be a nebulous topic. Can you discuss a little more about cannabinoid policy and conceptions in Canada? Zack: We’re coming up on the one-year anniversary of recreational marijuana legalization, but medicinal cannabis has been legal for about two decades. With the legalization of recreational cannabis though, we’re seeing fairly rapid change in perceptions of what the truth is. It’s tough to keep up with. With academic detailing, it was challenging to decide how to tackle it – can we just talk about the medicinal cannabis side? Or do we have to dive deeper? When we dug into it, it became clear that we also had to talk about the recreational side. For example, the people we provided our services to also wanted to know, “if I decline my patient cannabis prescriptions, what will they be able to get on their own?”  NaRCAD: Did RxFiles choose to launch its cannabinoid campaign with the passage of the Act, or has this been planned for a longer period of time? Zack: It’s coinciding with our work on pain, following our work on pain and opioids. In addition, because legalization was approaching, the providers had more questions because their patients were asking about cannabis as an alternative to opioids. NaRCAD: How have provider responses been to the cannabinoid campaign so far? Zack: It’s welcomed. Our information is usually welcomed. There’s some frustration over how little information there is out there. While frustrating, I think it’s kind of comforting to know that we’re not that far behind. It’s kind of mixed, but at the same time, they’re still happy to get information from a trusted resource. There's a lot of gray area information right now because it's a newer field.  NaRCAD: Right now is a shifting and transformational time, especially with something like cannabinoids with a distinct history of stigma and legalization, even with all this new interest. As an academic detailer, how do you source your information knowing that there isn’t enough research out yet and a lot of gray area information? How do you begin to build a campaign around a topic like this? Zack: The evidence pyramid gives us the best approach for practical information, for people who are the interface of care. You want to find high quality, synthesized information. Whether its osteoporosis or COPD or pain or cannabis, you start with the guidelines and figure out what kind of information they are providing. We started with some recently published guidelines and it was a synthesis of systematic reviews, and made an attempt to summarize all the evidence of where cannabis was found to be of benefit. We also reviewed the bibliography with all the primary literature and metanalyses. This process is pretty similar for any academic detailing topic. The other process is going to the people we provide services for, and asking what their patients are asking to treat with cannabis. They tend to ask about cannabis for pain, insomnia, or for things like tremors and that gives us some guidance in terms of what kind of literature we want to find. Of course, we are also looking into what the key messages are in the information we find and distribute. With cannabis, the interesting thing was the lack of information on the different conditions it could be used for. In some ways, it was easier, as weird as it sounds. We didn’t have as much reading to do on that topic.  NaRCAD: Is there any advice you would give any other academic detailing organizations considering this topic for a campaign? Zack: One, you’re going to have your conversations about stigma. There isn’t a perfect picture of who uses cannabis and it could be absolutely anyone. You’ve got to have the conversation about stigma and get to know your own biases. In the same vein, we thought about how important word choice and language is. We thought about whether or not we call it cannabis, marijuana, pot, or cannabinoids. Do we call it a medication or a product? All of those words and the considerations that we’ve given opioids - do we call them "addicts", or is it "dependence", and what are the differences between addiction and dependence? The third piece would be that you’ve got to talk to your providers in your local area and find out what their main questions are. Your job is to provide a service, and if you can find out what their wants and needs are, you’ll provide a far more satisfying service for them and could establish strong relationships that you can build on. There will be a lot of information out there and you will need a lot of leads to help you sort through it all. This won’t be the last time we're addressing this. NaRCAD: Thank you for taking the time to speak with us, and for leading the charge in bringing cannabinoids to the conversation about treatment for pain.  Biography. Zack Dumont is an clinical pharmacist with the RxFiles Academic Detailing Service in Regina, Saskatchewan, Canada and a new expert facilitator for NaRCAD's training courses. He has been involved with the RxFiles since 2008, with experience in both academic detailing and content development of RxFiles’ evidence-based drug therapy comparison tools. Zack maintains clinical practices for inpatient internal medicine, with more specialized experience in anticoagulation and heart failure. His professional interests include teaching evidence-based medicine, knowledge translation, development of clinical decision supports, collaboration, and leadership. Zack graduated as a Pharmacist from the University of Saskatchewan in 2008. Following graduation, he completed a hospital pharmacy residency with the Regina Qu’Appelle Health Region, where he currently serves as a Clinical Support Pharmacist, with involvement in training new staff, precepting pharmacy residents and undergraduate students, and providing clinical support to various health region committees and working groups. Guest Blog Interview: David O’Riordan, MPharm, MPH, PhD Senior Pharmacovigilance Officer Pharmaceutical Care Research Group University College Cork, Ireland Tags: Detailer Visits, International, Training  NaRCAD: Thanks for speaking with us, David! Tell us a bit about your professional background in healthcare, and how you became involved in academic detailing. David: I am a pharmacist by training, and a couple years ago I decided to carry out a PhD in Clinical Pharmacy at the University College Cork. As part of the PhD, I completed a systematic review examining how pharmacists can be utilized to optimize prescribing in primary care, including through academic detailing. After finding NaRCAD’s resources through a Google search, I registered for the NaRCAD conference in Boston. Dr. Fischer, Dr. Avorn, and all the other attendees at the conference were very encouraging. I left the conference determined and enthused to lead an academic detailing intervention back home. Dr. Avorn and Dr. Fisher put me in touch with Eimir Hurley, a PhD scholar in Ireland, who formerly worked in academic detailing at Alosa Health, and who ended up being a great help in executing the intervention.  NaRCAD: That’s terrific—it sounds like you had a great team at your disposal to begin this work. Can you tell us a little about the unique characteristics of the Irish health system? David: Ireland has a public and private health system. Public patients are more likely to wait longer for appointments. Private insurance is a substantial cost to individuals, though. The health care system is quite fractured unless you’re a private patient. Pharmaceutical drug representatives are also allowed to visit primary health practices here. NaRCAD: In April, you published a study titled “Pharmacist-led academic detailing intervention in primary care: a mixed methods feasibility study” in the International Journal of Clinical Pharmacy. Why did you choose urinary incontinence as a clinical topic? David: As this was a feasibility study, I decided to use one topic as part of the intervention. I organized a meeting with a group of general practitioners (physicians) who would be involved in the academic detailing intervention. The topic of urinary incontinence was chosen by the physicians because they highlighted that it was a topic not discussed regularly among themselves, and currently their only source of information is provided by pharmaceutical drug representatives.  NaRCAD: What barriers to success did you come across in your feasibility study? David: For this project, I was the only academic detailer. I started detailing after going to the two-day Basics Academic Detailing Training in Boston in May 2016. In some cases, during the roll out of the intervention I found it difficult to get past the practice manager, but luckily I had learned strategies on getting in the door in Boston that were useful in my effort. On a few occasions, the practice managers didn’t follow through on connecting me with the physicians. I got around this by utilizing physicians I knew in other practices to gain access to their practice. A lot of it came down to how well you know the physicians. I was lucky that they trusted me when I spoke to them. When I did get to meet with physicians, they all seemed very enthusiastic. NaRCAD: Can you talk a bit more about how receptive physicians were to academic detailing? David: Absolutely! This was a mixed methods study, so my colleague Eimir Hurley carried out focus groups after my detailing sessions to evaluate the feasibility of the intervention. Eimir conducted the focus groups on my behalf to reduce bias. The physicians liked that I wasn’t from a pharmaceutical company and that the sessions only lasted 10-15 minutes. They liked that local physicians had chosen the topic, and I wasn’t coming with my own agenda. NaRCAD: How are you or others going to use your feasibility study results to implement across the country? David: I am currently not involved in academic detailing, but I hope to be again in the future. If someone from another part of Ireland read my paper, they would recognize that physicians are very willing to take part in academic detailing. From my experience physicians didn’t feel threatened and really enjoyed the interaction. They liked the interactive style of the visits, and the way that that the evidence was delivered. My study provides a platform for other researchers to detail to a wider group of physicians in Ireland. NaRCAD: Anything else? David: I am very grateful for the NaRCAD team for providing the academic detailing training. I knew literally nothing about academic detailing, and through meeting their team members Sarah Ball, Amanda Kennedy, Mary Liz Doyle-Tadduni, and others, I felt encouraged to go back and detail. I was the only person from Ireland at the training, and the NaRCAD team gave me some useful feedback. I really enjoyed academic detailing, and I was especially proud when my paper was published. I discovered there is an appetite for this educational intervention in Ireland.  Biography David O’Riordan, MPharm, MPH, PhD Senior Pharmacovigilance Officer Pharmaceutical Care Research Group University College Cork, Ireland David holds a Masters in Pharmacy (MPharm), Masters in Public Health (MPH), Post Graduate Certificate in Teaching and Learning in Higher Education (PG Cert) and a PhD in Clinical Pharmacy. He has extensive experience as a community pharmacist. He previously worked as a Lecturer in Clinical Pharmacy in University College Cork (UCC). While there, he contributed to and assisted in the delivery of research-led teaching at undergraduate and postgraduate level. He also supervised on a number of research projects. He was a clinical trials pharmacist involved in the Thyroid Hormone Replacement for Subclinical Hypo-Thyroidism Trial (TRUST). This was a randomised placebo controlled clinical trial comparing levothyroxine to placebo in community dwelling older adults (≥65 years) with subclinical hypothyroidism (SCH). He is also a tutor on the Irish Pharmacy Union (IPU) Academy. This educational initiative was developed by the IPU to support pharmacist engagement with Continuous Professional Development (CPD). He is currently the Senior Pharmacovigilance Officer at the HRB-Clinical Research Facility, UCC. NaRCAD & Training Facilitator Loren Regier, BSP, BA  Tags: Detailing Visits, International Our team's training facilitator Loren Regier recently shared these pearls of wisdom about talking (and listening more) to front-line clinicians. In 1:1 academic detailing visits, detailers have the challenge of finding the right balance between sharing information and acquiring insight into a clinician's practice. It's the kind of balance an expert detailer can execute well, but how? Loren's tips on talking more when necessary to draw out the clinician's needs by asking good questions, and toggling to actively listening and talking less to understand clinicians' biases, are below. Talk More: -If someone is at the point of having “bought in” to a concept/idea, they may just need information. In this situation, it's okay to talk a little more, especially if you sense the “thirst for relevant information.” Talk Less: -If, however, a person has not yet bought in to an idea, it is often more important to talk less, or move towards equalizing the talking. -They will reject too much information that they don’t believe. But in discussing, there is the chance to explore ambivalence, raise doubts, and compare notes. -In all cases, learn to listen and listen well. -I What quick tips would you share with other detailers on assessing needs? Sound off in the comments section below! Biography. Loren Regier, BA, BSP
Clinical Director, Academic Detailing Service, Centre for Effective Practice, Program Coordinator, RxFiles Academic Detailing, U of S, College of Pharmacy/Nutrition, Facilitator, Educational Outreach/Academic Detailing Training | Loren is the Program Coordinator of the RxFiles Academic Detailing Service in Saskatoon, SK, Canada. Loren has guided the development of this provincial academic detailing service since the first pilot project began in 1997. Loren is active as a member of the Canadian Academic Detailing Collaboration and provides training and consultation to various programs and initiatives. Read more.  by Arielle Mather, MPH, Education & Training Manager Tags: Conference, International, Jerry Avorn, Opioid Safety On November 13th and 14th, 2014 NaRCAD hosted the Second International Conference on Academic Detailing. The focus of this year’s conference was on educational outreach in an era of rapid health care reform, with perspectives from prominent figures in government, research, and business. The conference explored a pressing clinical theme on each day, including presentations of academic detailing programs currently addressing these topics in the field. After Dr. Jerry Avorn, NaRCAD’s co-director, opened the conference with a review of the past, present, and future of academic detailing, Dr. Joshua Sharfstein, Maryland Secretary of the Department of Health and Mental Hygiene, discussed the challenges of improving health care and outcomes for the residents of his state. Jean Slutsky, Chief Engagement and Dissemination Officer of the Patient-Centered Outcomes Research Institute (PCORI) reviewed the key principles for effectively communicating research results that improve patient health outcomes. The clinical theme for Day 1 was prescription opioid use and overuse. Dr. Harry Chen, Vermont Secretary of the Agency of Human Services set the stage by reviewing the origins of current problems with opioid use and sharing details of his state’s initiatives for prescribing pain medication. This talk was followed by an interactive panel session that highlighted two academic detailing programs (in South Carolina and New Mexico) seeking to reduce opioid overuse and abuse. Small group breakout sessions allowed for more detailed conversation about these programs and other specific topics. Day 2 of the conference began with an overview of the business case for evidence based practice, presented by Dr. Troyen Brennan, Chief Medical Officer of CVS Health. Daniel Wolfson of the American Board of Internal Medicine Foundation, followed with a presentation on the Choosing Wisely campaign, which is designed to engage clinicians in the critical questions of how to make healthcare safer and more efficient. Dr. Alice Bonner of Northeastern University began the conversation of the day 2 clinical theme: antipsychotic medication use in long term care. After Dr. Bonner’s introduction, two ongoing academic detailing programs (in Massachusetts and Saskatchewan, Canada) aimed at addressing this problem shared their insights. The challenge of sustaining academic detailing programs was addressed by Frank May, who has successfully implemented programs in multiple settings internationally. Dr. Madeleine Biondolillo, Associate Commissioner at the Massachusetts Department of Public Health, made the final presentation, reviewing how academic detailing fits in with the other approaches that the state uses to improve health. In addition to the formal sessions, conference attendees from 15 US states, Canada, Europe, and Australia had a chance to interact informally, share ideas about academic detailing, and develop connections that will help support increased collaboration in the future. The third installment of this AHRQ funded conference series will be held next year in November 2015. Finalized dates and registration information will be announced in the coming months. If you would like specific slide sets from any of the conference presentations, please email us. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|

