|
Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Stigma, Evidence-Based Medicine, Health Disparities, Conference Missed our event? Check out the AD Summit videos and materials on our Summit Hub.  We’re fresh off of the excitement of hosting our Academic Detailing Virtual Summit, “A Deeper Understanding of Our Impact on Patient Care.” In prioritizing patient-informed care more than ever before, we explored patient narratives through live interviews, workshops, and special panels, all within a virtual space. Innovations included AD for criminal justice involvement, care delivery redesign for veterans, affirming care for transgender and nonbinary people, and patient-informed communication on sex positivity in HIV prevention. Take a peek at some of the highlights from our event below! AD Fireside Chat: A New Spin on a “Keynote Address” We opened our AD Summit with a real-time interview featuring the originator and co-founder of NaRCAD, Dr. Jerry Avorn, and the National Director of the Veterans Affairs Pharmacy Benefits Management Academic Detailing Service, Melissa Christopher. Audience members were excited to throw ideas around and ask questions about:
Program Development Workshops: Attendees Led the Charge! Our revamped course catalog of workshops invited attendees to be in the director’s seat, as well as behind the scenes as co-creators in small groups. Participants created resources that we’ve published on our website and social media channels, sharing creativity and expertise with the larger AD community. Our workshops covered a wide range of topics including:
 The Pleasure Project The Pleasure Project Special Panel: Understanding Critical Care Needed for Formerly Incarcerated Patients The outstanding team from New York City Department of Health and Mental Hygiene (NYCDOHMH) shared their groundbreaking detailing campaign, “Public Health Detailing for Criminal Justice Involvement”, with an audience that was hungry for innovation around inclusivity. The NYCDOHMH team shared NYC clinicians’ understanding of formerly incarcerated patients’ care, including clinicians who met the campaign with stigma, and those who were grateful to see such a campaign being implemented. Best Practices Spotlight: Prioritizing the Patient Experience For the first time in NaRCAD’s history, we highlighted leaders in the field who’ve been prioritizing the patient experience. The San Francisco team created space for conversation and discussion about gender-affirming care and ways to encourage safe clinical environments for transgender and nonbinary individuals through language, storytelling, and community outreach. We also heard from the Arizona team about the importance of pleasure being part of a patient’s sexual health history and the role of a detailer in supporting these conversations between clinicians and patients. 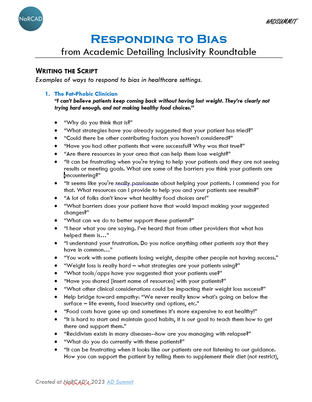 Inclusivity Roundtable: Real-time Script Creation We wrapped up our AD Summit with a roundtable session where attendees co-created a scripting resource to empower detailers to combat stigma during visits. We asked attendees to come up with responses to the stigmatizing comments below. A five-page resource was created in 60 minutes! 1. “I can’t believe patients keep coming back without having lost weight. They’re clearly not trying hard enough, and not making healthy food choices.” 2. “I don’t want those patients at my practice. They’re so difficult to handle and are really just looking for another opioid prescription. Treatment won’t work for them.” 3. “I’m so tired of keeping up with all these different pronouns. You’re either a man or a woman. It gets in the way of providing care.” 4. “I don’t need to use an assessment tool. I can always tell when someone’s at high risk of contracting HIV.” We want to continue these conversations, hear about your team’s innovations, and share resources in person this fall at our annual conference in Boston, MA. We hope to see you there! -The NaRCAD Team A special thank you to all of our AD Summit attendees and presenters as well as our partners at the Agency for Healthcare Research and Quality. For more information on our presenters, you can view the AD Summit Program Book. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation! Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Conference, Health Disparities We have exciting news at NaRCAD! We’re hosting our first-ever Academic Detailing Virtual Summit on June 22 & 23 from 12-5 pm ET. We’ve listened to what you’ve asked for, so we’re prioritizing hands-on skill-building, program development workshops, roundtables, and live interviews, with an emphasis on high interactivity and networking opportunities! How is this different than our annual conference? It's unique in three ways: more creativity, more patient voices, and more in-depth workshops. Our Summit invites our community to build real-time resources with one another – it's a chance to create as much as to learn. Our lens will focus more on patient-informed care as we move closer to examining patient narratives. Each day, you’ll choose a workshop track where you’ll connect with experts and community members on topics that matter most to you. Here’s a sneak peek of our program development workshops (to view the entire agenda, visit our AD Summit webpage): Day 1 Program Development Workshops:
Day 2 Program Development Workshops:
Join us! Registration is NOW OPEN. You can access all the presentations and one workshop per day for a fixed rate of $89. As a special promotion, the first 10 people who comment on this blog will receive free registration for the event. Hurry – you don’t want to miss this!
We look forward to learning from all of you. See you there! -The NaRCAD Team Can't join our event? Join us at our annual conference in November in Boston, MA! Overview: Dr. Nate Rickles, PharmD, PhB, BCPP, FAPhA is an associate professor pharmacy practice at the UConn School of Pharmacy with experience in developing AD programs, most recently for the CDC-funded CEDPP (Connecticut Early Detection and Prevention Program) project. Dr. Natalie Miccile, PharmD, MBA currently works as a retail pharmacy manager at ShopRite Pharmacy. She’s working with Nate to onboard pharmacies participating in the CEDPP program and working with the pharmacy students who are supporting the process of referring patients to screening, diagnostic, and prevention services. by: Winnie Ho, Program Coordinator Tags: Cancer, COVID-19, Detailing Visits, Health Disparities, Program Management  Winnie: We’ve been excited for a chance to speak with you both! Nate, you spoke on our Clinical Innovations in AD session at the NaRCAD2020 Conference, sharing your work to support underserved, and sometimes undocumented, women in accessing care. Thank you both for joining us today – can you tell us a little bit more about the program and the issues it addresses? Nate: CEDPP consists of two components: the Connecticut Breast and Cervical Cancer Early Detection Program (CBCCEDP) and the Well-integrated Screening and Evaluation for Women Across the Nation (WISEWOMAN). The services are offered free of charge with the goal of significantly increasing breast and cervical cancer services for medically underserved women. The Department of Public Health’s traditional outreach method of using clinical navigators at established WISEWOMAN sites could only reach a relatively small population. We received a CDC Innovation Grant to investigate the role that community pharmacies could play in increasing referrals to a free public health prevention program for vulnerable populations, as these pharmacies are accessible, front-line, and generally well-trusted in the community.  W: That’s an important goal to close this gap and to ensure more women can access the services they need. Why did your team feel that AD was a useful approach to address the lack of access to screening services? Nate: I’m very passionate about the notion that building relationships through 1:1 connections are going to be more powerful long-term in creating behavioral change. AD works so well because the techniques are very persuasive in dealing with common barriers like pharmacists believing there’s little time in their day, not enough staffing, or not the right financial incentive. Our project manager Peaches Udoma had sent out flyers and e-mails to local pantries and shelters, but we hadn’t received many referrals through this tactic. The predominant way we’re getting referrals is through 1:1 outreach with pharmacists and our students reaching out to the referred participants to connect them with services.  Winnie: Can you tell us more about how your intervention navigated the pharmacists’ barriers you described? Natalie: We had a lot of interest from pharmacists, especially when they learned about the impact they could have. However, for a full month, we weren’t seeing results. When I checked in, we learned that they were genuinely overburdened with their workflow, which wasn’t surprising. We had to think about who else in the office could do it – and it turned out to be the pharmacy technicians. They were often at the point of sale and would be more likely to know if patients were uninsured or underinsured. We began detailing the pharmacy technicians directly instead. Many of them were bilingual, which helped in distributing the right flyers to the right women. We worked with the pharmacy technicians on communicating the benefits our programs offered, with attention to utilizing accessible language and avoiding unnecessarily complicated healthcare terms. We learned that emphasizing key things like free gym memberships or free nutritional services provided was very useful in getting women to agree to be referred. Addressing the language barrier and slight language changes was key to us finally getting referrals. However, when COVID-19 hit, we had to reassess since we started getting zero referrals again. It made sense as few people want to wait around in a public space, and pharmacies also became overwhelmed. Our team pivoted to reaching out directly over the phone after receiving lists of potential contacts from the pharmacies. We wanted to show our partners that we could be resilient in this time and to not let this program fall through.  Winnie: Pivoting your intervention to have team members directly contact the women you were trying to refer instead of through the pharmacy technicians must have required your team to make adjustments to accommodate language needs. How did your team tailor the AD intervention to address language barriers? Nate: We noticed that we had many of the women we reached out to who spoke Spanish as a native language, and quickly realized we were probably losing a lot of patients because of the language barrier. We onboarded a pharmacy student, Isabella Hernandez, who, in addition to being a very dynamic, charismatic, and outgoing person, also spoke Spanish. Once Natalie onboarded her and shared the main concepts around the screening and referral, Isabella was quickly able to pull in over 80 referrals; we didn’t have even half or a third of that through our prior efforts. We’ve been closely tailoring our work since, with flyers in Spanish, Portuguese, and in Arabic. We have also Arabic speakers to communicate with Arabic-speaking patients, and we have the capacity to expand into other languages.  Natalie: I originally worked with the lists of contacts we received and tried to engage directly. However, because we recognized our bilingual pharmacy students were able to better engage with these women, my role now is to oversee our callers, get their referrals, and help touch base with site navigators to ensure referrals are being processed, and how we can improve our screening process. We’re prioritizing language accessibility because our first encounters are first impressions. Our patients matter, and we want to make things as smooth as possible for them. We’re even at a point where Isabella is running trainings with our other callers, so she can give them hints on how to be more flexible in the conversation to fit our clients’ needs. Winnie: This is a really outstanding demonstration of flexibility and tailoring a program to address barriers to practice change. We hope that other programs continue to follow your example of integrating best practices to communicate with patients from diverse communities! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Nathaniel ("Nate") Rickles is an Associate Professor in the Department of Pharmacy Practice at the University of Connecticut School of Pharmacy. He received his B.S. in psychology and chemistry from Dickinson College, Pharm.D. from the University of the Sciences in Philadelphia, M.S. and Ph.D. in the Social and Administrative Sciences from the University of Wisconsin-Madison. Dr. Rickles also completed a psychiatric pharmacy practice residency and is board certified in this area. He was inducted as a Fellow of the American Pharmacists Association. His primary research interests are to develop, implement, and evaluate intervention programs that improve pharmacist communication with patients and/or other team members and subsequently to improve medication adherence and patient safety. Primary teaching interests involve courses on communication skills, mental health, health behavior change, cross-cultural health care, and research methods. Dr. Rickles is an active researcher with several grants and publications involving enhancing the role of pharmacists in changing patient and provider behaviors.  Natalie Miccile received her PharmD from the University of Connecticut School of Pharmacy in Storrs, CT and MBA from the University of Connecticut School of Business in Hartford, CT. Her MBA concentrations include Digital Marketing and Strategy and Investment Analysis. She works as a consultant for UConn School of Pharmacy on research initiatives that involve enhancing the role of pharmacists in the community setting and is pharmacy manager at Shop Rite Pharmacy in Milford, CT. Dr. Miccile is MTM certified and an active member of the Connecticut Pharmacists Association. This interview features Carla Foster, MPH, who leads the conceptualization, implementation, and evaluation of Public Health Detailing as an Epidemiologist within the Bureau of Alcohol and Drug Use Prevention, Care and Treatment (BADUPCT) at the New York City Department of Health and Mental Hygiene (NYC DOHMH). She is currently activated for the COVID-19 emergency response as Lead Analyst managing the Reporting Unit within the Integrated Data Team of DOHMH’s Incident Command System. By Winnie Ho, Program Coordinator Tags: Data, Detailing Visits, Evidence-Based Medicine, Health Disparities, Program Management, Stigma, Substance Use, Training  Winnie: Hi Carla! You’ve certainly had a lot on your plate with so many diverse campaigns. Can you walk us through the conceptualization process for your detailing campaigns, and how your team came to choose cocaine use as your current detailing topic? Carla: We can start with some data on this. In 2018, more New Yorkers died from drug overdose than from homicide, suicide, and motor vehicle crashes combined. Cocaine – in both crack and powder forms – has played an increasingly prominent role in this crisis. The mortality rate from overdose deaths involving cocaine more than doubled between 2014 to 2018, amounting to 52% of all drug overdose deaths in NYC. Some of the associated risks are serious - increased exposure risk to fentanyl, cardiovascular disease events and death.  W: That’s stunning data. Especially in the midst of the opioid crisis, it’s important that we don’t lose sight of other substance use issues going on right now. I’d love to learn a little more about the challenges and lessons that your team has learned by detailing on cocaine use. C: First, we have to be aware that fentanyl, a powerful opioid 50 to 100 times stronger than morphine may be found in many substances, including cocaine. We’re very concerned about fentanyl and cocaine because people who use cocaine do not have tolerance to opioids and are at even higher risk for overdose. It’s also important to address the perception of who is most impacted by high mortality rates. There’s this idea that cocaine use is more prominent in younger populations, but our data show that it’s actually impacting an older population more than many might expect. In particular, residents age 55-84 in the Bronx Borough have experienced the largest increase in cocaine overdose death rates in New York City from 2014 to 2018.  That’s why it’s critical for us to raise awareness in an effort to mitigate misconceptions and stigma around risky use and those who may have a substance use disorder (SUD). In addition to shame, there are still very real potential socioeconomic and legal consequences from disclosing substance use, which can deter folks from even seeking help. We take into account the unjust consequences of policies applied unevenly according to race, and how this impacts implicit biases in terms of which patients are thought to use substances, which types of substances they might use and even more critically, which type of treatment, if any, they are offered. Implicit biases combine with the effects of systemic racism to compound these consequences. It’s important to note that it’s not race that drives poor health outcomes, but racism.  W: Challenging stigma is one of the most powerful ways that detailing campaigns can combat the damage done by the War on Drugs, because stigma can make the difference of whether or not people receive dignified care. With a campaign so focused on addressing stigma and with a topic this important, how do you prepare your detailers for this task? C: We devote a significant amount of time towards training our detailing reps – a week-long training, 8 hours a day. We spend a large amount of that time talking in detail about stigma as related to cocaine use. It’s critical to us that our detailers are comfortable and knowledgeable when speaking about this topic, because it sets the tone for the providers who then set the tone for their patients. We ensure that our representatives are prepared to respond to a wide range of questions or comments, because this builds the provider-detailer relationship and enhances the value of the detailing visit. We’ve found during our follow-up visits that this support has led to high provider engagement with the campaign and providers reporting incorporation of the key recommendations into their daily practice, which is the aim of our public health detailing campaigns.  W: How have providers responded when detailed on a topic that carries so much stigma? C: The good news is that we’ve found NYC healthcare providers to not only be receptive to our work on substance use, but they’re eager to partner with us to support their patients once they learn about the severity of the issue. Our team provides statistics that relate to the provider’s specific neighborhoods and specialty, giving them real-time pictures of what’s happening with the patients they see. We know that it’s still a difficult topic to bring up, so we help address this with our action kit resources on stigmatic language and counter-top brochures that signal to patients that the provider’s office is a safe place to discuss these issues.  W: It gives me tremendous hope to hear about that there’s been enthusiastic response from providers. It means that things are changing. Let’s also talk a bit about program sustainability. Your team has worked extensively on campaigns across multiple topics. What have you learned from implementing past campaigns? C: Each public health detailing campaign is different, but we’ve learned some key strategies that support the growth and success of subsequent campaigns: 
Our overall goal is to do everything we possibly can to improve the health of our fellow New Yorkers. I like to remind our detailers of this James Baldwin quote that informs our public health detailing mission: “Not everything that is faced can be changed, but nothing can be changed until it is faced.” Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Carla Foster, MPH is an Epidemiologist at the New York City Department of Health and Mental Hygiene (NYC DOHMH). Her research focuses on the implementation and evaluation of public health detailing campaigns across New York City with the aim of reducing overdose mortality. Prior to joining the NYC DOHMH, she led development of clinical practice guidelines at the American Urological Association. She received dual Bachelor of Arts degrees in Africana Studies and Neuroscience from Wellesley College. Carla also obtained her Master of Public Health Degree in Epidemiology from Columbia University. Anna Morgan, MPH, RN, PMP, NaRCAD Program Manager Tags: Conference, COVID-19, Deprescribing, Diabetes, E-Detailing, Elderly Care, Health Disparities, HIV/AIDS, International, Jerry Avorn, Mental Health  Map of where NaRCAD2020 attendees tuned in from Map of where NaRCAD2020 attendees tuned in from Over 240 members of our worldwide community came together to be a part of something special--our 8th annual conference, and our first in a virtual setting. We were able to expand our reach and overcome barriers like travel time and financial constraints that have prevented our colleagues from attending previous conferences. There was a palpable sense of positivity, enthusiasm, and resilience, especially in a virtual space. We’re so proud of evaluations that cited a renewed sense of passion and commitment to AD based on the new lenses we applied to our programming, including comments about feeling “empowered” to continue this work in the year ahead (even amidst inevitable Zoom fatigue.) Check out our highlights and access all event resources below and on the Conference Hub.
 With so many of you expressing a continued need around more of our peer working sessions, we’ll be focusing largely on that in 2021—we can’t wait to support your work this year. In the meantime, tell us what you need to make next year a success. See you in 2021. The NaRCAD Team Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation! Featuring: Mary Nagy, MPH, RN/BSN, Public Health Detailer, HIV Care & Prevention Unit, Michigan Department of Health and Human Services, NaRCAD Training Alumnus Tags: Detailing Visits, Health Disparities, HIV/AIDS, Sexual Health, Stigma  NaRCAD: Thanks for joining us, Mary! You’re a Public Health Detailer in the HIV Care & Prevention Unit at the Michigan Department of Health & Human Services. Before we talk about how you got into your current role, can you tell us what you were doing before that? Mary Nagy: I was an ER nurse for five years. During that time I worked all over the country in lots of different settings, but I noticed the same patterns playing out no matter what city I was in. I was seeing patients daily who were either in the last hours of their lives or needing immediate life-saving interventions as a result of medical problems that might have been avoided entirely through basic services or preventative medicine. The longer I worked ER, the more clearly I saw the effect of systemic forces and environment on health, their unequal distribution across society, and the more I wanted to find a way to work towards health equity. I decided to study public health, and earned my master’s degree in Environmental Health Science at the University of Michigan. In addition to giving me the opportunity to design and carry out my own research, the program I did had a strong health policy component, which helped me add to the understanding of healthcare delivery I formed during the time I spent at the bedside. 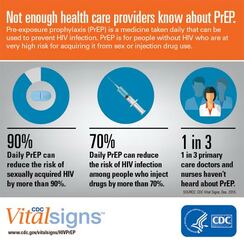 NaRCAD: Tell us what interested you about your current position and what a “day in the life” of a detailer looks like for you. Mary Nagy: I saw the job posted and was immediately interested in it because I think detailing, especially on the topic of pre-exposure prophylaxis (PrEP), is a really effective way to strengthen prevention infrastructure and affect health outcomes. Clinicians are under a lot of pressure and I was drawn to the idea of being a source of relevant, high quality, trusted information. The detailing program here in Michigan is comparatively young and its development is ongoing. Fortunately for me, lots of folks have been willing to help! I've drawn from a broad range of sources has been really helpful during detailing visits, because the needs of providers are so diverse; folks are asking about billing and coding for PrEP visits, standing orders, HIV risk assessment, nuts and bolts of services offered by our state lab, STI screening and trends, and financial supports for PrEP, best practices with PrEP initiation and follow up, and more. I’ve been working hard to broaden my knowledge base, but also to identify resources for questions I don’t know the answers to and topics I’m weaker on.  Image from UNAIDS Image from UNAIDS NaRCAD: Why are you passionate about HIV prevention, and why is academic detailing for HIV prevention so important? Mary Nagy: Even though I’m very new to the field, I think it’s a very exciting time to be doing this work because I do believe it is possible to end the HIV epidemic in the US within the next few decades. Racial and ethnic minorities continue to be underrepresented in PrEP utilization and overrepresented in new HIV diagnoses, and I want my work to contribute to correcting this. I think PrEP can be a tool for health justice and being part of that is valuable to me.  NaRCAD: You’ve mentioned environment a couple of times. Can you tell us how environment is connected to HIV contraction and prevention, if at all? Mary Nagy: I think that’s where my mind goes, because I’ve seen the powerful effect of environment on health, and this is certainly true on a population level. I never want to diminish the power and agency of individuals, but everyone operates under multiple layers of forces. Examples of this include policy, especially the persistent legacy of overtly racist housing policies; the “war on drugs” and resulting mass incarceration; or a justice system that data shows us doesn’t work in the same ways for everyone. These systemic forces, applied to millions of people over many decades, result in the disparities we see in HIV rates, overall health, wealth, and many other areas. Increasing access to PrEP means we can mitigate some risk for folks who might have more exposure due to the environmental context in which they live. For Michigan, one of the ways detailing can help make PrEP easier to access is increasing geographic availability. A large portion of our state is rural, and many counties do not currently have a known PrEP provider. Another challenge is, of course, cost. The cost of PrEP and associated visits and screening tests is a policy issue, and while we hope and expect to see cost come down in the future, in the current landscape, it's important to prioritize educating providers and their staff on available financial supports and how to apply them, so cost doesn’t keep people who can benefit from PrEP from getting and maintaining access.  Image: University of New Mexico Image: University of New Mexico NaRCAD: In addition to geography and coverage, what are some other barriers you’ve encountered when doing academic detailing for HIV prevention? Mary Nagy: Stigma around HIV and other STIs is a big issue. We know that when providers talk openly with patients about their sexual health, they’re better able to accurately assess risk for HIV and STIs and screen and treat appropriately, but those conversations are not happening with enough regularity. Rates of STIs like gonorrhea, chlamydia, and syphilis have been rising, and continue to increase, so there's a lot of opportunity there. NaRCAD: How has detailing been received overall? Are providers open to education on PrEP? When I think about why detailing is important and why I’m doing it, the first thing that comes to mind is a recent survey of primary care providers MDHHS carried out in Southeast Michigan. Providers were asked which supports would best help them to incorporate PrEP into their practice, and "education" was by far the most frequent answer. In addition to the research I’ve seen indicating detailing is an effective intervention to change provider behavior, it's clear that the providers themselves agree that education is important. If we can work with providers to make PrEP available and easy to initiate and maintain, the protection it offers from HIV can improve health outcomes for patients at high risk.  Biography Mary Nagy, MPH, RN/BSN Public Health Detailer, HIV Care & Prevention Unit Michigan Department of Health and Human Services Mary is the public health detailer for the State of Michigan and conducts direct outreach with medical providers to support HIV prevention strategies and stigma reduction statewide. She received her master’s degree in Environmental Health Science from the University of Michigan School of Public Health where as a Graham Sustainability Fellow her research focused on municipal water quality and affordability. Mary also has several years of experience working in as an Emergency Department RN in trauma centers across the US and her work in health equity is informed by her time as a frontline health worker. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|