|
An interview with Rachelle Woods, MSN, RN, Nurse Consultant at the Colorado Department of Public Health and Environment (CDPHE). By: Aanchal Gupta, Program Coordinator, NaRCAD Tags: HIV/AIDS, PrEP, Detailing Visit  Aanchal: Hi Rachelle! We’re so excited to learn more about the work you’re doing. To start, can you tell us about your background and your current role? Rachelle: I’ve been a registered nurse in the state of Colorado for 26 years. My clinical background is obstetrics and gynecology (OBGYN), which includes family planning, HIV/STI education, and direct patient care. I've also taught OBGYN and other health courses at a few nursing schools and universities as well as in the community. I've been at CDPHE for a little over three months and will be functioning as a nurse consultant and public health detailer. I'm currently working to harness a deeper understanding of the needs of each of the communities that I'll be serving within our state. In order to do that, I’ll be conducting a statewide community needs assessment. I plan to tailor the needs of each geographic area when detailing to identify areas of urgent need and take into consideration epidemiological concerns among special populations. CDPHE is implementing a public health detailing approach to control STI and HIV infections which are increasing in Colorado and across the nation. My role is to serve as both a recruiter and consultant to optimize healthcare integration of public health prevention practices regarding STIs, HIV, and viral hepatitis within our state.  Aanchal: It’s exciting to hear how your background intersects with your current role at CDPHE. I’m curious about the community aspect that you spoke about. What services and supports already exist in your community for the patient populations you’re working with? Rachelle: CDPHE has 80 contracts with several community-based organizations and local public health agencies throughout the state. Our goal is to collaborate across sectors and provide services within several of our communities. Our partners include pharmacies, pharmacists, clinical providers, non-clinical persons, public health agencies, publicly funded healthcare centers, and other community-based organizations.  A graph from CDPHE showing the number of clients who received a PrEP prescription from 2015-2018. A graph from CDPHE showing the number of clients who received a PrEP prescription from 2015-2018. Aanchal: It's important to leverage others in the community to provide the best care and support to patients. Tell us about CDPHE’s prior successes with HIV PrEP detailing. Rachelle: We had a public health detailer a few years back that focused on PrEP rollout. Between 2014 to 2019, PrEP use increased from 383 to 3,659 among Coloradoans. We’re now working on expanding our public health detailing program and have been focused on partnering with other local agencies to bring the best evidence to clinicians. The Denver Health and Hospital Authority has helped us disseminate relevant updates to providers so that we can better meet the needs of Colorado’s most vulnerable populations.  Aanchal: It’s impressive that your program had success with your first detailing intervention and that you’re continuing the momentum with a community-based approach to detailing. Since you began the role a few months ago, what resources helped you to learn more about academic detailing? Rachelle: I spent a great deal of time on the NaRCAD website and reviewing our internal resources. I was introduced to NaRCAD by my director, Rosemarie. She said, “I know that you have experience with educating clinicians, but I want you to take a look at this organization and see if perhaps there could be anything of benefit for you.” I spent a whole week absorbing the materials on the NaRCAD website. Being able to access the webinars and videos on demand was especially helpful. I'm somebody who likes to keep my finger on the stop button when watching a video so I can replay and relisten. I loved the fact that I could get a firm grasp of the concepts of AD at my own pace.  Aanchal: I’m glad you found the NaRCAD website to be useful as a new detailer. Based on that, if someone were in your shoes and was just starting out as a detailer, what advice would you give them? Rachelle: When you initially step into something new, you're outside of your comfort zone. Do you harness the fear and turn it into excitement for learning or do you shy away from it? It's important to step into it and remember that the goal is to better the communities that we live in. Take that excitement and run with it. Don't be afraid – as long as your intentions are in the right place, everything's going to work out. Aanchal: Definitely! I’m sure that’s a reminder many of us need to hear. Thank you so much for speaking with us, Rachelle! We look forward to hearing more about your findings from the community needs assessment and your exciting detailing project. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography: Rachelle Woods, MSN, RN brings an expansive clinical, leadership, and professional development background deeply rooted in OBGYN, STI/HIV, Family Planning, Transgender Health, and Infection Control to the Public Health Detailer role at CDPHE. Rachelle’s passion for all things infectious has afforded her a career rich in opportunity to meet people where they are and engage in robust discussion surrounding STI/HIV transmission, prevention, biomedical interventions and resources, and personal wellbeing. Her audiences have spanned multiple platforms and have included clinical and non-clinical staff, patients/families, teens, and students. Rachelle is looking forward to applying her skills and experience in support and growth of the Public Health Detailer role at CDPHE. Peer-to-Peer Learning: Building Meaningful Relationships through NaRCAD’s Peer Connection Program2/7/2022
An interview with Cheryl Radeloff, Senior Health Educator at the Southern Nevada Health District in the Office of Disease Surveillance. By Aanchal Gupta, Program Coordinator, NaRCAD Tags: Detailing Visits, HIV/AIDS, PrEP  Aanchal: Hi Cheryl, we’re looking forward to hearing more about your experience in the NaRCAD Peer Connection Program! How did you hear about the program and what encouraged you to sign up? Cheryl: I found out about the 2021 Peer Connection Program from a NaRCAD e-blast and was intrigued with the idea of joining a learning community. I instantly knew that I wanted to sign up since it would be a place where I could feel comfortable asking questions. I gravitated to the fact that I would be communicating with other peers in the field during cohort gatherings and learning about approaches that we could emulate in our program.  Aanchal: Yes, having that 1:1 time with your peer, as well as the cohort gatherings where other participants in the program come together, are added ways to network with the detailing community. Would you recommend this program to others that are interested in signing up? Cheryl: Absolutely! You should sign up even if you're a seasoned academic detailer or new to detailing. You're going to get tips, insights, and resources to get you started in a welcoming environment. This is a field where you never stop learning so it’s not only an opportunity to share lessons learned, but to learn from others as well. There are people from across the world who have different experiences and expertise that you can take back to your program.  Aanchal: One of the special aspects of the program is the sharing of resources and ideas. Are there any conversations that you had with your peer that made an impact on your detailing work or changed the way you thought about your program? Cheryl: The time spent with my peer was invaluable. During changing times with COVID-19, it can be daunting, and you tend to wonder if you’re doing things right or where you should even start. She was so generous in talking through challenges such as funding, recruiting providers, and more with me. She even shared a PowerPoint that they developed to educate pharmacy students about academic detailing. During the mid-point peer connection gathering, I was able to learn about a program in Chicago. They were very innovative; if they didn’t have an approach in place for their program, they designed it. Although my clinical topic may not be the same as others, there are still concepts and tools that I can model after these programs.  Aanchal: It’s great to hear about these fruitful conversations you had and how there’s always something to learn from others in the detailing community. How would you describe your experience overall with the peer connection program? Cheryl: Every time I attended a peer gathering, I always learned something and never had to question what I was gaining from these meetings. I think it’s essential to hear about what’s going on in the field. It’s difficult as we’re all busy people, yet it’s important not only for learning and development, but a necessary element to have peers to consult. I found the structure of this program to be helpful as we were given the reins to set up 1:1 meetings with our peer match over several months. In addition to that, there were gatherings where the entire cohort could come together and connect which I appreciated.  Aanchal: Those are some great takeaways, and we are glad to hear about the impact the program has had on your work! To wrap up, we’d love to learn more about what you’ve been up to at the Southern Nevada Health District. Cheryl: I’ve been with the Southern Nevada Health District for 13 years. Along with being a detailer, I’m also the public health co-chair for our HIV prevention planning group. We meet a few times a year to talk about HIV prevention initiatives, as required by the CDC. I also work with many of our community-based organizations to talk about the fundamentals of HIV. Academic detailing has been an important strategy for the work that we do. Our main AD initiatives we've been working on are uptake of PrEP and PEP. We have two PrEP navigators who've been educating the community about these initiatives. Lastly, congenital syphilis has been a big topic for us as we’re currently fourth in the country for the highest rates of syphilis. Aanchal: Thank you so much for sharing your experience, Cheryl. We’re so glad that the Peer Connection Program has had a positive impact on your detailing work and can’t wait to hear more about your program’s AD initiatives in the future. We look forward to continuing these connections with our 2022 cohort! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography: Cheryl Radeloff is currently a Senior Health Educator with the Southern Nevada Health District Office of Epidemiology and Disease Surveillance. Formerly she was Disease Investigation and Intervention Specialist II. She is also an adjunct professor of Sociology at UNLV as well as Women’s Studies at the College of Southern Nevada. She received her Ph.D. in Sociology from the University of Nevada, Las Vegas in 2004. Her dissertation “Vectors, Polluters, and Murderers: HIV Testing Policies toward Prostitutes in Nevada” explored the development of mandatory testing laws for legal and non-legal sex workers in the state of Nevada. Her work duties include serving as the public health co-chair for the Southern Nevada HIV/AIDS Prevention Planning Group as well as training community providers on Rapid HIV Testing. She is the co-author of multiple editions of Transforming Scholarship: Why Women’s and Gender Studies Students are Changing Themselves and the World with Michele T. Berger for Routledge Press. An interview with Karen Curd, Program Manager, Midwest AIDS Training and Education Center in Indiana (MATEC-IN). by Anna Morgan, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: HIV/AIDS, PrEP, Training  Anna: Thank you so much for joining us today, Karen. We're excited to learn more about you and your program. Can you start off by telling us a little bit about your professional background and how you ended up in your current role? Karen: Thanks for having me! I stumbled into public health by accident. I majored in kinesiology in college and interned with a health promotions department at a local hospital after graduation. That’s what really got me interested in health education. I ended up meeting somebody who worked at the local county health department in STI prevention. She encouraged me to apply for an open position as a disease intervention specialist; that ended up being both a challenging and rewarding job. It taught me so much about public health and I was hooked! I moved on to work as the STI screening and surveillance coordinator, which allowed me to interact more with healthcare providers. Nearly a decade went by of working in STI prevention before I joined the Midwest AIDS Training and Education Center-Indiana (MATEC-IN) team as the training coordinator. I now work as a program manager at MATEC-IN.  Anna: We’re so happy you ended up in public health! Can you share more about your current role as program manager and about MATEC-IN as a whole? Karen: MATEC is part of the national network of AIDS Education and Training Centers. MATEC houses 10 states across the region, and I work at a local partner site in Indiana. We provide training and technical assistance to healthcare providers throughout the state, primarily focusing on HIV and increasing their comfort and capacity to provide HIV care. For those outside of the field, I usually explain my role as part health educator, part event planner, and part networking and resource specialist. A lot of what we do is connect healthcare providers to all the amazing organizations and individuals who provide support and care for people living with HIV. We spend a lot of time talking to people, finding out what information or resources they need, and connecting them. We also develop new tools and trainings as needed. Anna: Your team is doing such incredible work supporting and connecting healthcare providers. How do you see the strategy of academic detailing fitting into this work? Karen: The Ending the HIV Epidemic (EHE) initiative aims to reduce new HIV infections in the United States by at least 90% by the year 2030 through activities focusing on four pillars. The four pillars are: diagnose, treat, prevent, and respond. At MATEC-IN, we hope to focus our EHE efforts on the diagnose and prevent pillars by encouraging and engaging primary care providers throughout our state. We want to be recruiting these community providers to increase routine HIV testing, and to become comfortable recommending and prescribing pre-exposure prophylaxis, or PrEP, to their patients. We hope to use academic detailing to educate these busy providers. We see AD as another great tool in our toolbox.  Anna: You recently partnered with us for a customized academic detailing virtual training and successfully recruited 18 trainees. Can you tell us a little about what that process was like and what tools you used to recruit those trainees? Karen: We planned our training as a regional MATEC opportunity and opened recruitment to our entire 10-state region to any organization funded by EHE. We first hosted an introduction to academic detailing session for our other MATEC sites which gave them an opportunity to learn about what academic detailing was and begin thinking about who they might want to recruit from their state for the 3-day NaRCAD training. Because the training is extremely interactive and is limited as far as size, we wanted to make sure that we were recruiting the right individuals. Our director, Malinda Boehler, developed a recruiting tool that we shared with the different site directors in our region. We then asked each site to recruit two to three individuals from their state and have the individuals complete a short questionnaire that we developed prior to registering for the training. Anna: You did a thorough job recruiting detailers and it shows; we had an amazing training with you all because you selected such engaged and passionate trainees. Do you have any tips you would share with other folks who are looking to recruit a large number of trainees for a customized training? Karen: Set expectations. I would stress the importance of clearly defining training expectations as far as what attendees should and should not expect to learn over the 3 days. We wanted to make sure that it was clear to trainees that the NaRCAD training would not cover the day-to-day of how an academic detailing program would be rolled out at their specific institution, but rather the communication techniques used during an academic detailing visit. We had a lot of conversations with trainees before they came to the training and I think that helped to set those expectations. Anna: That’s a great tip! You were in a unique position where you were able to observe the training. What were some of your key takeaways?  Karen: I’m so thankful to have had the opportunity to observe. Even though I technically wasn’t a participant who engaged in role play, I found that learning from other trainees was the most valuable. The training facilitators were also excellent. They provided a very safe and structured environment for learning and role playing. Not only did the participants have the opportunity to practice and role play, but they were also encouraged to offer feedback to peers. We had a range of folks in our small group; some had been working in the field for years and some were brand new to the field. It was amazing to see them learn from each other. One participant shared with me that the training provided them with persuasive communication skills that will be useful in situations outside of a detailing visit, like an interaction with a client, a patient, or partner organization. Anna: The skills you learn at an academic detailing training can be applied to so many situations, including those with family and friends! Is there any additional advice you would share with others who are looking to become a detailer or support a detailing program? Karen: Be flexible. When our team initially began looking for information about academic detailing, we were looking for existing materials that we could adapt for our state and do the detailing ourselves. After meeting with your team at NaRCAD and learning more about the process, we realized that we needed to redirect our efforts to recruiting trainees from EHE funded sites within our region to broaden our reach. I would also recommend starting recruitment efforts early to allow plenty of time to find the right recruits in order to build a successful training cohort! Anna: That's great advice, Karen. What does the future look like for this group of trainees and how do you plan to continue to support them across state lines? Karen: Our region has hired an EHE coordinator who plans to engage frequently with the training cohort. We want to bring these folks together through monthly check-ins because we know that detailing can be isolating. Not all the trainees are doing the same exact work, but we think getting them connected with folks who are doing detailing in other states on the same topic will be beneficial. We’ve also been spreading the word about academic detailing at our health department in Indiana since our state doesn’t have a structured AD program like some other states do. We hope to get more folks trained from our state in the future and use academic detailing across diverse topic areas. Anna: How exciting! We’re thrilled to continue to partner with you as academic detailing expands throughout your state and region. We look forward to future trainings and hearing about your team’s successes! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Karen Curd is the Program Manager at the Midwest AIDS Training and Education Center (MATEC) in Indiana. She has worked in public health for nearly two decades, starting her career as a Disease Intervention Specialist for the Marion County Public Health Department (MCPHD) in Indianapolis, Indiana. She also served as Screening and Surveillance Coordinator for MCPHD before transitioning to the role of HIV/MAI Training Coordinator at MATEC Indiana in 2011. In her current role of Program Manager, Karen oversees several MATEC initiatives focused on providing training and technical assistance to healthcare providers throughout Indiana. Karen received her BS in Kinesiology from Indiana University in Bloomington, Indiana. An interview with Kelsey Genovesse, PA-C, MPAS, Public Health Detailer and Clinician, AIDS Education Training Center (AETC), University of Utah Infectious Disease. The public health detailing program at the AETC is currently focused on expanding pre-exposure prophylaxis (PrEP) throughout the state of Utah and educating clinicians on STI prevention and guidelines for correct treatment. by Anna Morgan, MPH, RN, PMP, NaRCAD Program Manager Tags: Detailing Visits, E Detailing, PrEP  Anna: Hi Kelsey! Thanks for joining us on DETAILS today! Can you tell us a bit about your background, your current role, and your program? Kelsey: I’m a physician associate (PA) by training and previously worked in family practice with underserved communities, including migrant farmworker populations and patients in federally qualified health centers. Our program in Utah is tiny; our AETC only has three or four employees. I do the outreach, schedule the detailing sessions, detail the clinicians, collect the data, and evaluate the program. We’re fortunate that our first year was so successful and we’re looking forward to continuing to expand our program over time. This year, we were even nominated for a Utah Telehealth Education Award! Anna: That’s incredible – what a great accomplishment! Your program is unique in that it started with e-Detailing right from the beginning. Can you tell us a little bit about that?  Utah AETC Utah AETC Kelsey: We attended an in-person Public Health Detailing Institute run by the San Francisco Department of Public Health in partnership with NaRCAD in March of 2020. We had planned to focus on in-person detailing only in Northern Utah because we didn’t have the capacity to drive all over the state. Shortly after we left the training, the pandemic shut everything down and we had to move our program to a virtual platform. We couldn't put the program off because our funding timeline wasn’t changeable, so we gave e-Detailing our best shot. Anna: Your attempt at e-Detailing turned out to be quite successful. Can you tell us more about the nitty gritty of pivoting to e-Detailing? Kelsey: Absolutely. When it became clear that we were moving to e-Detailing, we had to recreate our entire plan. We began with strategizing about outreach to clinicians. Nobody in Utah knows what public health detailing is - this is not a model that has been used here before. We had to get creative about spreading the word about our program. We connected with experts on our topics and clinicians who were already doing a lot of training on PrEP and asked them if they wanted to do a detailing visit with us. This was extremely successful, and we received referrals and warm handoffs to other clinicians from those initial visits. We also used a lot of listservs so that we could contact multiple clinicians at once. We worked with the Utah Department of Health and gave them a flyer we created about our program that was sent to all the clinicians on their listserv. We even connected with local medical groups, like the Utah Medical Association, a PA Association, and a Nurse Practitioner Association. These approaches brought in a lot of clinicians for detailing visits and helped us spread the word.  Anna: Rather than emailing each clinician and sending out hundreds of individual emails, you targeted hundreds of clinicians at once – I love that approach! It sounds like you also had some great AD champions in your network. Kelsey: Yes. I found that I was also doing a lot of e-Detailing sessions with folks who were not clinicians but were involved in the healthcare system in another capacity. I discovered that when I was connecting with these folks, whether it be someone at the health department or a representative from a health-based community program, they were wonderful champions who knew a lot of clinicians. Visits with these non-clinicians also helped spread the word about our program and open access even more. Anna: Many programs have faced challenges when gaining access virtually, but you were able to overcome many of these challenges with your innovative approaches. Has your program faced any other challenges with e-Detailing? Kelsey: We frequently detail clinicians who are short on time. I’ve tried to create a schedule where I have a little bit of availability, almost seven days a week, so that there are more options for clinicians whose schedules are busy. I also try to keep the detailing visits focused on the topics that clinicians are most concerned about. I always send them a comprehensive follow-up email with the resources they've asked for after the visit. Anna: Clinicians’ limited time is a common challenge for detailers—these strategies are helpful to employ when this challenge arises. Do you see specific opportunities with e-Detailing that you wouldn't see with in-person visits? Kelsey: Yes! Within our first year, we connected with providers in rural areas that may have taken us a longer time to gain access to using an in-person approach.  Anna: That’s a great point, especially for a state as large as Utah. Do you envision incorporating any in-person detailing in the future? Kelsey: We’ve had a few clinics that have asked for us to come in person, but as we just discussed, it can be time-consuming. However, there is something to be said about showing up and seeing what a town or clinic looks like in order to understand a community structure better. We’re going to try adding it in in the future. Anna: Being physically present in a clinic can certainly help with assessing the needs of a clinician. You mentioned earlier that within your role you’re not only doing outreach and detailing visits, but you’re also working on your program’s evaluation. Can you share a bit about that? Kelsey: Kristefer Stojanovski, MPH, PhD, the Evaluation Specialist from San Francisco Department of Public Health, has helped us tremendously with our evaluation work. We have pre- and post- surveys for clinicians to fill out with each detailing visit to collect data related to their knowledge around the clinical topic. It has an open format at the end to allow clinicians to request certain information prior to their first visit and leave feedback and comments. I'm hoping that as our sample size increases, that the data starts to look a little bit more robust. At the end of last year, we also sent an email asking clinicians to give us feedback on how they felt their experience was and if they felt like this was a program that was worth continuing. At least a third of our detailed clinicians sent back responses, and all of them were very positive. Most of the feedback reflected on how useful the information was when it was tailored and directed to their personal practice. A couple of clinicians noted they felt they were practicing to the standard on the topics, but detailing helped them gain knowledge they were unaware they were missing. It was nice to see that folks felt that it was useful. Anna: We’re excited to hear more about your evaluation as you gather more data. We'll wrap up with our final question: what’s one piece of advice you'd give to other programs that are just starting out, specifically with e-Detailing? Kelsey: Be flexible in your approach – group detailing sessions or detailing sessions with non-clinicians can be extremely effective, and can lead to 1:1 clinician visits. Also, stay organized! Keep track of who you're reaching out to and who you're following up with. Having all that information tracked over time will help with your evaluation down the road. Anna: That's fabulous advice, Kelsey. We’re looking forward to continuing to watch your program grow and succeed! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Kelsey Genovesse is a Physician Associate with the AIDS Education Training Center and University of Utah Infectious Disease Department. After eight years in underserved family medicine Kelsey started the Utah Public Health Detailing Program to expand support and education to providers throughout the state of Utah on evidence based practices surrounding STIs and PrEP. She also provides care in the Free HIV PrEP Clinic with the University of Utah offering in person and virtual services to help expand access to HIV Prevention throughout the state of Utah, specifically to those without insurance. In June 2021 she was Nominated for a Deborah LaMarche Telehealth Excellence Award for her work with the Utah Public Health Detailing Program. Innovations in e-Detailing: Using Digital Platforms to Increase PrEP Prescribers in Oregon4/15/2021
An interview with Ashley Allison, Lead Training Coordinator, Oregon AIDS Education and Training Center (AETC). Ashley works with health departments and clinic systems to coordinate HIV-related training across the state ranging from prevention to care and treatment. She also oversees the detailing program where their main goal is to expand PrEP access in Oregon. by Anna Morgan, MPH, RN, PMP, NaRCAD Program Manager Tags: COVID 19, Detailing Visits, E Detailing, HIV/AIDS, PrEP  Anna: It was so nice to catch up on your team’s progress at our recent virtual training with the San Francisco Department of Public Health! Your program launched about two years ago and really took off when you pivoted to e-Detailing. Can you tell us more about that? Ashley: Our program started with in-person visits and we would send our detailers out with a little briefcase of materials and an iPad full of slide decks—it was pretty “old school”. When the pandemic began, we had to take a hard look at our entire program to successfully pivot to e-Detailing. As we began e-Detailing, we developed an outreach process and approach that has been working well for us. Here are a few of the steps and considerations that you can share with other new programs:
We’re trying to find new ways to engage clinicians who’ve received the materials but haven’t yet scheduled a detailing visit. We want to provide multiple entry points and make our detailing visits more accessible.  Anna: Thanks for outlining this process and giving us a better understanding of how your program gains access to clinicians! What do you do to connect with clinicians who have yet to set up an appointment? Ashley: One of our solutions has been what we call “virtual office hours”. In the calendar slots where a detailer has no detailing visits scheduled, they can hold open office hours, and we send out a promotional email about them to clinicians. Multiple clinicians can be there at once and chat about anything under the umbrella of the HIV care continuum. The detailer slowly shifts the clinicians who attend office hours into a detailing relationship by creating opportunities to meet again 1:1 to further discuss certain topics. Anna: That’s such an innovative approach in gaining access. Can you discuss some of your team's other recent successes as it relates to virtual detailing?  Ashley: Virtual detailing has allowed us to increase our number of detailing visits due to the decreased number of resources and time required to complete an e-Detailing visit, including scheduling. We spent a lot of time looking into different platforms for automated appointment scheduling and ended up finding the Appointlet scheduling app. It allows us to manage all of our detailers’ schedules in a centralized place. It’s extremely intuitive and easy to use. We’ve also switched our evaluation from a handwritten survey to a digital version on Survey Monkey. We made our survey significantly longer when we moved it to Survey Monkey and pulled a lot of our questions from example surveys from other programs and the national HIV curriculum website. Our questions are specific to knowledge, attitudes, and practice and allow us to distinguish if a clinician isn’t doing something because they don’t have the knowledge, they don’t feel comfortable, or they don’t see it as within the scope of their role. Despite the lengthier survey, our response rate has been much higher now that we can send follow-up emails with the survey link right in it. Survey Monkey has also allowed us to quickly review the pre-evaluation data prior to detailing visits. If there are any red flags, we can highlight it for the detailers so they can customize which key messages will likely resonate with the clinician during their visit. Anna: That's great. There are certainly advantages to using a virtual platform to conduct the different steps of the program process. What are some of your goals for the remainder of 2021?  Ashley: We want to start implementing a successful hybrid model of in-person detailing and e-Detailing while also training our new detailers in a robust and consistent way. We want to continue with our main goal of increasing the number of PrEP prescribers in Oregon and making it more accessible across the state. We also want to start detailing pharmacists, depending on how the current legislation lands around providing supports for pharmacists to prescribe PrEP. We feel confident in our key messages for primary care providers. We’re excited to start crafting our key messages in ways that appeal to pharmacists and address the different barriers to implementation for them as well. Anna: Those are excellent goals! What’s one tip that you would offer other academic detailing programs who’d like to replicate your success? Ashley: Utilize e-Detailing; it’s a wonderful tool! Many developers are coming out with apps to serve this new digital landscape that can assist in implementing e-Detailing successfully. It’s just a matter of finding the right tools by taking a little bit of extra time and patience to experiment. I would also say that it’s important to build a relationship with your state’s health department leadership and obtain an official endorsement letter from the state supporting your activities. Establishing a relationship not only positively impacts your program’s visibility and ability to gain access to clinicians, but it also helps to make sure you're aware of other outreach initiatives, which allows you to align efforts and not duplicate processes. Anna: Terrific advice, thanks, Ashley! You’ve given us such a unique perspective on e-Detailing. We look forward to continuing to hear about all of your team’s successes and groundbreaking ideas. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Ashley has been with the Oregon AETC since 2018 where she works to bridge the gap between local public health priorities and education and training opportunities available to providers. Before joining the Oregon AETC, Ashley spent over two years working for local and international HIV focused CBOs in Johannesburg, South Africa. A majority of her work in Johannesburg focused on grant writing and managing the implementation of community-based HIV medication adherence models in partnership with provincial and municipal public health. Prior to moving to Johannesburg, Ashley spent five years working at Planned Parenthood in Portland, OR occupying a variety of roles, including clinic assistant, phlebotomist, patient advocate, and call center representative. Ashley credits her passion for supporting patient access to quality HIV prevention and care to the experiences she had with patients while providing HIV testing and counselling services at Planned Parenthood. An interview with Vishal Kinkhabwala, MD, MPH, HIV Prevention Activities Coordinator, HIV Prevention Unit, Michigan Department of Health and Human Services. The overarching goal of the HIV Prevention Unit is to expand access to PrEP for patients throughout the state of Michigan. by Anna Morgan, MPH, RN, PMP, NaRCAD Program Manager Tags: Conference, Detailing Visits, E-Detailing, HIV/AIDS, PrEP  Anna: We’re so happy to be catching up with you today, Vishal! Can you tell us a little bit about yourself and how you got into the work of academic detailing? Vishal: My background is in both public health and medicine. After finishing medical school, I realized that as much as I loved the clinical aspect, I wanted something that combined both my passions of public health and clinical medicine. My first job after graduating was in New York where I linked newly-diagnosed HIV patients into care. About a year later, I found an opportunity at the Michigan Department of Health and Human Services that fit with what I ultimately wanted to do, HIV prevention. My current work is focused on ending the HIV epidemic in Wayne County. One of my favorite parts of my job is detailing, which I do part-time. Our program officially began detailing in September of 2019. We’re in the process of making the jump to e-Detailing, but we’re still in the planning stages. Anna: Before we chat about how you and your team have been preparing for e-Detailing, let’s talk about how clinicians in Michigan have received your messages around PrEP. Were clinicians receptive to your detailing efforts when you were conducting in-person visits? Vishal: Most clinicians that we detailed were either already familiar with PrEP or had that enthusiasm to learn about it. Many of the clinicians were excited about helping with MDHHS’s overall goal of increasing patient access to PrEP and talking about the associated HIV prevention counseling. Clinicians were typically familiar with PrEP but weren’t aware of the nitty-gritty details of how to prescribe and manage it. A big part of what we discussed during our detailing visits was identifying which patients are candidates for PrEP. Our program’s purpose is to increase access, even if it’s just for one or two patients.  Anna: It’s wonderful that the clinicians you’ve detailed have been supportive of your program’s goals. Transitioning to e-Detailing will certainly be easier knowing that you have support from clinicians. What have you learned so far from planning for e-Detailing? Vishal: It’s been fun prepping for e-Detailing with our team. The big thing I’ve learned through networking with detailers from other jurisdictions is to be flexible and be prepared for any situation, especially in the virtual environment. You might have one idea of how your session will go, and it could go in the opposite direction, which is part of the charm of detailing. It’s about forming a connection and tailoring your methods to what the clinicians' and practices' needs are. I’m a relationship-oriented person, and I feel like that’s one of the most rewarding parts of doing this. One of the things that also excites me about virtual education is the access to information right at your fingertips. For example, I was detailing a clinician about PrEP and HIV prevention last year who asked me, "Well, I have this issue with a lot of patients with STDs. Can you talk to me about STD treatments?" It was an in-person visit, so I only had the materials that I had brought with me, which were all focused on HIV. The beauty of doing e-Detailing is that you can have resources pulled up and can get the information for the clinician almost instantaneously. As I said earlier, detailing is all about having that relationship, meeting the clinician where they're at, and serving their needs. Virtual education gives you another tool to be able to do just that.  Anna: What a positive spin on e-Detailing! Speaking of sustainability, that’s the theme for our upcoming conference. You attended our conference last year in Boston and will be presenting at our virtual conference this year. What were some key takeaways from last year’s conference that you were able to bring back to your program and implement? Vishal: Last year’s conference was my first exposure to NaRCAD and the world of detailing- it was honestly one of the coolest experiences I’ve ever had. It was great to be exposed to e-Detailing through the virtual detailing panel before it was even brought to the forefront during COVID. Because I was hired a few months prior to the conference, I had not attended a training yet. I joined the “AD 101” breakout group, which was supremely helpful. When I got home, I did mock detailing sessions with my colleague and reviewed all the resources on the NaRCAD website. I also practiced detailing on the stress balls I have in my office! Anna: It’s so nice to hear how impactful the conference was for you as a new detailer. We strive to include a diverse audience of new and veteran detailers each year. What are you looking forward to most about this year’s conference? Vishal: There are so many absolute rock stars in the field of detailing. I’m looking forward to getting to see familiar faces and meet new faces over the virtual platform. I’m excited for the exchange of ideas, programs, and concepts. So many people have given me ideas for our program in Michigan. It’s such a good feeling when I can say that not only have I received help from others, but that I’m able to inspire other people. It’s also comforting to know that this is such a passionate group of people that no matter the adverse situation, the work continues getting done. I’m counting down the days until the conference in November! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Vishal has been working with the Michigan Department of Health and Human Services since August 2019 as the HIV Prevention Activities Coordinator. His work focus is on program planning and implementation for the Ending the HIV Epidemic Initiative, focused on southeastern Michigan. As part of this initiative, he works as a part-time Academic Detailer with a focus on HIV Prevention with the overarching goal of increasing access to PrEP throughout the state of Michigan. He completed his Master of Public Health degree from Benedictine University in Lisle, IL in August 2013 and his Doctor of Medicine degree from Avalon University School of Medicine in Willemstad, Curacao in June 2018. Prior to working for the State of Michigan, Vishal worked for the New York State Department of Health as a Disease Intervention Specialist, working on a pilot HIV Molecular Clusters initiative. Vishal is particularly looking forward to moving the Michigan Department of Health and Human Services PrEP Detailing program forward into the realm of virtual “eDetailing.” An interview with Kristefer Stojanovski, MPH, PhD(c), Public Health Researcher and Evaluation Specialist, Capacity Building Assistance Program, San Francisco Department of Public Health by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Data, Evaluation, HIV/AIDS, PrEP, Sexual Health NaRCAD: Hi, Kristefer! Thanks for taking the time to chat with us today. Can you tell us a bit about your background and the work you’re currently doing as it relates to academic detailing?  Kristefer: Thanks for having me. I’m a public health researcher and an evaluation specialist with the Capacity Building Assistance Program at San Francisco Department of Public Health. I serve as a specialist and a technical assistance provider for the West region of the United States. My work is focused on data and evaluation of academic detailing programs that are working on topics like sexual health, HIV, and PrEP. My main goal is to help folks measure, or think about, what “success” may look like for an academic detailing program. NaRCAD: What data do you think is most important for academic detailers to track during their visits when measuring or thinking about success? Kristefer: I see evaluation data and detailing efforts as one complete package. Detailers should think about their data at a high level and focus on the information they’re collecting and how that information serves the overall goal of detailing, which is to improve knowledge, attitudes, intentions, and behaviors of providers and clinics. At the same time, detailers should think about how they can show that they’re achieving that goal. For example, it’s useful to track how many providers they’ve seen, how much time was spent with providers, what they talked about during the visit, the resources that were provided, how the providers plan to use those resources, if a follow-up visit was scheduled, and the purpose of that follow-up visit. It’s important to track a mix of quantitative and qualitative data, but the critical components that should be tracked are the outcomes and the process of detailing. NaRCAD: What about academic detailing programs? What data should they collect?  Kristefer: In a typical detailing program, detailers have a longitudinal, continuous outreach to providers. There’s an interesting conversation to be had about how we can use that temporal matrix as a tool and strategy for evaluation. I’m interested in how we can use the work academic detailers are doing – the actual visits themselves - as pieces of data over time. For example, if detailers are collecting some of the rich conversation that they’re having with providers or clinics, it’s fascinating to track those conversations over time and see how the detailing program is changing the knowledge, attitudes, intentions, and behaviors of those providers and clinics. There’s a lot of work that detailers are already doing that can be easily turned into data sources for both the detailing effort and the evaluation effort. I like to think about how we can make things as simple as possible. NaRCAD: Is there a specific platform that makes things simple and is best for collecting data for academic detailers and programs? Kristefer: That certainly becomes a little bit more individualistic when thinking about the needs, challenges, and abilities of each jurisdiction. Detailing is a conversational effort that is attempting to make concrete behavior change, so it becomes more convoluted when you think about how to track a conversation. Some jurisdictions might have a place to track conversations in their electronic health record, where others may not. At the most basic level, detailers can chart their conversations on one-page Word documents. The detailers I worked with charted their conversations with providers over time and eventually put it in one large PDF that could be easily uploaded into a qualitative data analysis software. You have to be creative when it comes to tracking this information. NaRCAD: How would you recommend that programs with limited resources go about data collection and evaluation?  Kristefer: A lot of times we say we want to have high-tech solutions when we don’t actually need them. For a resource constrained department, having that one-page Word document that allows detailers to chart their interactions is more than enough data. Charting for just five minutes after a detailing visit about everything that took place becomes a wealth of information. You can also use an Excel document to input data from provider surveys. There are many low-tech ways to track information and it’s important to be aware of the low hanging fruit in terms of data collection. You want to be able to easily collect data that serves the detailing efforts, the program, and the evaluation and improvement process. NaRCAD: That’s a great way to look at it. What are some best practices for using data for leadership buy-in? Kristefer: I can’t stress enough how important data is in getting leadership buy-in. Data is not only quantitative and qualitative, but also using the information gathered to tell a story. It would be a strong statement if someone was able to go to leadership with a story about how providers have changed their practices based on the detailing effort. Using concrete results and showing leadership that detailing is making a change is extremely helpful for buy-in. Being able to show crazy big outcomes with your data won’t happen, but sharing stories from providers and clinics about how detailing has helped them is quite moving. I’ve heard some amazing stories during my evaluation. For example, detailers helped providers at some clinics to provide patients with directly observed therapy for PrEP at the same time that they were providing them with medication-assisted treatment for opioid use disorder. It’s impressive that detailing at those sites was able to make the clinics think creatively and be able to provide PrEP to these patients. NaRCAD: That certainly is impressive! What has surprised you the most about the academic detailing data you’ve evaluated?  Kristefer: I can’t help but to think that pharmaceutical companies spend millions of dollars and resources on this model and they certainly wouldn’t have been doing this for decades if it didn’t work. We’re almost a little late to the game as public health practitioners, but through my experience evaluating some of this work and reading other evaluations, I’ve been shocked by how much providers truly value detailers. It’s fascinating to see how these health systems and departments are viewed as trusted partners by providers and clinics and how detailing has served as a role to improve that partnership and collaboration. Providers have often said how crucial this information has been in getting access to Department of Public Health resources they didn’t even know existed, which is pretty sad. Seeing public health and the medical system working side by side in this kind of way has been breathtaking.  Biography. Kristefer Stojanovski is a PhD Candidate in the Department of Health Behavior & Health Education, School of Public Health at the University of Michigan. Kristefer has been doing community-based mixed methods research since 2010. His research explores the social and structural determinants to sexual health and HIV outcomes among key populations in the U.S. and in Southeastern Europe. Kristefer’s work interrogates how stigma drives HIV risk and infection using complex systems theory, structural equation, agent-based and multilevel modeling. Kristefer also translates his research into policy and decision-making. He is an evaluation specialist with the Capacity Building Assistance program with the San Francisco Department of Public Health. An interview with Brandon Mizroch, MD, MBBS, Provider Network Supervisor, Louisiana Department of Health by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Hepatitis C, HIV/AIDS, PrEP, Rural AD Programs, Sexual Health, Stigma, Training  Dr. Mizroch participating in a NaRCAD training Dr. Mizroch participating in a NaRCAD training NaRCAD: Thanks for chatting with us today, Brandon! We’re excited to be catching up with you. Can you tell us about your program at the Louisiana Department of Health and the work you’re currently doing? Brandon: Absolutely. I was hired to do work around PrEP and PEP, detailing providers across the state of Louisiana, in 2017. Since then, my role has expanded and I promote education for providers about syphilis, congenital syphilis, and Hepatitis C. Our department now has 3 detailers, including myself. Louisiana became the first state in the country to undergo an incredibly revolutionary Hepatitis C Elimination Plan, which has caused my detailing focus to shift. There’s been huge advancements in the drugs that treat Hepatitis C, but they’ve been inaccessible to much of the population due to cost. We negotiated a fixed rate price for Hepatitis C treatment and can now treat 100% of the population, compared to the 3% of the population we could treat previously. There’s been a big push to identify and train providers who’ve never previously treated patients with Hepatitis C. I’ve been leading the charge by getting the word out, running symposiums, and working with the marketing team that’s creating our statewide campaign.  NaRCAD: Wow, that sounds like innovative and exciting work. Can you explain your program’s approach a bit more? Brandon: I try to blend a few different approaches together. I attended the NaRCAD training during my first year as a detailer. NaRCAD built the foundation of detailing for me. I always use the NaRCAD methodology to get my foot in the door and identify providers who can be champions within their practices. I find it much easier to follow up and do longer didactic sessions about complex clinical topics when I use the techniques of academic detailing during my first face-to-face visits with providers. I connect with about 20 providers in this 1:1 model each month. I also work with residency programs, hospital systems, and present at Grand Rounds to expand my reach. There’ve even been instances where I’ve attended dinners for physicians that are hosted by pharmaceutical companies to network and identify new clinics that would benefit from detailing. NaRCAD: We’re happy to see that you’re blending academic detailing with other approaches. Do you provide follow-up to providers after your visits? Brandon: Follow-up is incredibly important, no matter what approach is being used. I like to send an email after each visit that includes digital resources for both providers and patients. I also offer providers the ability to call, text, or email me because of the apprehension that exists around topics where the knowledge base is still growing. Maintaining relationships with providers also ensures that we have a strong provider network that we can continue to educate on other clinical topics down the road.  NaRCAD: Building a connection with providers is imperative, especially as you move into different clinical topics. Your program spans the entire state. Do you find that there’s a difference when you provide clinical outreach education in rural vs. urban communities? Brandon: Yes, there’s certainly a difference. The providers in urban areas tend to have a higher knowledge base when it comes to PrEP and syphilis, perhaps due to marketing efforts or higher patient loads. This makes starting the conversation a bit easier. Additionally, urban communities have access to navigators, who help with non-medical aspects, like transportation issues, lack of health insurance, and long commute times that all prevent folks from getting the treatment they need. Providers in urban areas are also busier and easily distracted during 1:1 visits, which can make detailing a bit difficult. On the other hand, rural communities are quite the opposite. Providers tend to have more time in their schedules and are excited to sit down with somebody from the state office. They’re eager to learn, but there’s typically less of a knowledge base, making it slightly more difficult to start the conversation. I’ve also learned about patient barriers as well, which affect access and provider care. Patients in rural areas are often friends or family with those throughout the community, including those who work at clinics. The notion that you would know the receptionist or provider at a clinic is enough to deter folks from seeking medical care around a topic like sexual health. To encourage access, our state has created a TelePrEP program that offers PrEP services to anyone via telemedicine. Consultations take place over the phone, labs are obtained at third party lab companies, and medications are mailed right to the front doors of patients. It was originally created to help folks in rural communities who face stigma-related barriers, but we’ve expanded the program across the entire state of Louisiana. It’s a great referral service that I can share with providers.  NaRCAD: It’s wonderful that you’re able to identify these challenges and have resources and tools to address them. What’s one piece of advice you’d give to folks who are detailing on a similar clinical topic or have a large geographical region to cover? Brandon: It’s important to have several different ways of presenting information to the providers you’re detailing and to use varied approaches depending on the barrier(s) they’re facing. I typically focus on emotional connection, financial concerns, and the evidence and science behind the key messages I’m delivering. I’m also ready for provider resistance, and am prepared to address it, which is something I learned from NaRCAD. When it comes to detailing over a large and diverse geography, it’s always necessary to plan ahead. My general rule of thumb is that however many hours it takes to drive to a location, that’s how many providers I want to meet with while I’m there. I typically try to use larger educational events, like meetings with clinics over lunch, as my anchor point for longer trips. After I have that scheduled, I search for smaller clinics around the area where I can meet with providers 1:1. It’s all about maximizing your time.  Biography. Brandon Mizroch received his MD/MBBS from the University of Queensland/Ochsner Clinical School Program in November of 2016. Since taking over as the PEP/PrEP Provider Outreach Specialist at the Louisiana Department of Health in August, 2017, he has worked with hundreds of doctors statewide on HIV prevention best practice. Since then he has expanded his educational base and now serves as the head of the academic detailing department at the Louisiana Department of Health, Office of Public Health, STD/HIV/Hepatitis program. As the Provider Network Supervisor he has helped lead the provider Outreach for the state’s first-in-the-nation Hepatitis C Elimination program. From grand rounds presentations at LSU-Shreveport Hospital and Baton Rouge General, to state-wide symposia and conferences, to one-on-one counseling encounters at dozens of clinics all over Louisiana, he has helped spread awareness and education on HIV prevention, syphilis screening and treatment, and HCV screening and treatment through evidence-based care. 'Guest Blog | Alyson Decker, NP, MPH | San Francisco Department of Public Health Tags: Detailing Visits, HIV/AIDS, PrEP, Sexual Health  Our AD program is part of a 3-year demonstration project (CDC Project PrIDE), and as part of our grant-funded work our overarching goal is increasing PrEP access and prescribing to MSM (men who have sex with men) of color and transgender persons who are at substantial risk of acquiring HIV. Our goals include improving sexual health in the primary care setting, refining sexual health history-taking, increasing screening and testing for those with risks, promoting best practices around PrEP prescribing, and helping to establish relationships between our health department and our community providers.  The added benefit of public health detailing is that it also increases awareness about the issues that affect our community. I have been inviting clinicians that I meet to join us in our city-wide Getting to Zero consortium, which helps providers feel that they are part of this important movement of preventing HIV transmissions, deaths, and stigma.  In San Francisco, there is a need for urgency around this issue, especially because it’s become evident that as HIV transmissions continue to decrease, the disparities among new HIV positive diagnoses become more apparent. Many of these disparities are among communities who still may not be aware of PrEP, or are facing barriers to access. Our academic detailing program strives to reach the providers who work with these vulnerable communities.  When kicking off an intervention such as this, identifying the clinicians who see this target population is the first step. To do this, we used STD surveillance data to determine which providers and clinics were diagnosing syphilis and rectal gonorrhea and chlamydia, which are associated with an increased risk for HIV. However, since many providers are not performing appropriate screenings, we also reached out to clinics known to serve our priority population and those located in neighborhoods with the highest HIV incidences.  The next step is how to “get in the door” with these clinicians, which means finding a way to secure a 1:1 visit. I’ve found that initial non-responsiveness isn’t the end of the world—persistence pays off, so keep trying to get in the door, or find an entry point through other community contacts. Sometimes, choosing a different access point can really work well to start a relationship. There are many places where 1:1 visits aren’t feasible due to clinic structure or culture. If I’m able to detail to a small group, it can be a way to meet with a few providers and gain insight about how PrEP might be incorporated or enhanced in their setting. Being invited to an all-staff meeting is often an excellent way to kick off an introduction to this important intervention, and can result in follow-up conversations with individual clinicians. One benefit of meeting in small groups is that if a clinician hears a fellow clinician say that he or she is already prescribing PrEP, there may be more openness to discussing the topic; other providers might feel comforted in having a PrEP "ally", resulting in buy-in from the clinic overall. Some clinicians may think that this type of intervention isn’t relevant to their patient population; as I detailer, I often hear responses such as, “I don’t see this population reflected in my practice,” or “My patients don’t have this risk,”, even if it’s been proven that these clinics do, indeed, serve priority populations. In order to talk about PrEP, you first have to talk about risks for HIV, which often means talking about sex. I think there can be discomfort on both the patient and provider side, and sex is often still a stigmatized topic. There are also overarching resource barriers, including the fact that clinicians are extremely busy and have to address competing health needs in the primary care setting.  While a small pool of clinicians have minimal understanding of PrEP, and require a basic overview about elements like identifying potential PrEP candidates, how to take a good sexual history, and how to bring up PrEP in an appointment, I’ve found that many clinicians are aware to some extent about PrEP already, and are interested in next-level details about how to implement it. This might include what kind of testing is recommended, how to increase number of basic screens, and increasing their knowledge about comprehensive health. There are also providers who are very advanced in their knowledge of what options are available to populations with risks for HIV. This is where the academic detailing becomes more intricate; some providers are seeing lots of patients with risk factors, and may have been prescribing PrEP already. In a scenario such as this, my messaging focuses more on how to support clinicians in ensuring consistent follow-up with their patients, or in how to deal with multiple risk factors, such as when high-risk sexual behavior may overlap with instances of substance use or homelessness. For those who are just getting started, it may help to know that even after meeting with 300 providers, I still get nervous each time I prepare to detail, especially if I’m unfamiliar with a practice. Regardless of the nature of my visits, I walk away feeling that I’ve accomplished something if I’ve answered only one question that’s helped the clinician with his or her practice. And I’ve found that in most cases, the people I meet with are very thankful for this service, and are appreciative of the health department. I always thank providers for the work they do and remind them what an important role they have in the community.  Biography. Alyson Decker, NP, MPH Alyson Decker is a Clinical Prevention Consultant and nurse practitioner with Disease Prevention & Control at the San Francisco Department of Public Health. As the branch’s lead academic detailer, she helped develop San Francisco’s first HIV pre-exposure prophylaxis (PrEP) detailing program. Her role consists of detailing with community providers to increase PrEP prescribing in the primary care setting and promote best prescribing practices. In addition, she provides training assistance to healthcare providers and frontline staff around improving sexual healthcare and STD testing and treatment. She also sees patients at the municipal sexual health clinic, San Francisco City Clinic.  Mike Fischer, MD, MS, NaRCAD Director Tags: Conference, Director's Letter, HIV/AIDS, Jerry Avorn, Opioid Safety, PrEP, Training Fall is the season for conferences, and the most exciting one for us is #NaRCAD2017: Combatting Threats to Optimal Care! This year’s conference is a great chance for everyone interested in AD to learn more, whether you’re part of a long-standing program or just beginning to learn about the versatility and effectiveness of implementing this strategy to improve health outcomes. Our agenda is up, so take a peek, and register if you haven’t yet!  The keynote presentations will provide critical insights for creating and sustaining AD programs in different settings. Dr. Zoe Edelstein will kick off Day 1’s programming, representing the New York Department of Health and Mental Hygiene. This keynote will teach us about their public health detailing intervention to increase use of HIV pre-exposure prophylaxis (PrEP). The New York program was originally founded in 2002, so Dr. Edelstein’s presentation will help anyone from a public health background understand how to both develop and sustain AD, and to adapt it for new and pressing health challenges. 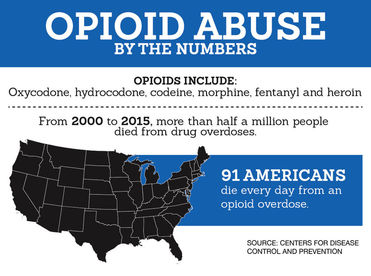 Dr. Carol Havens from Kaiser Permanente will provide a detailed overview of the longest-running AD program in the US, a program that was developed with input from Jerry Avorn soon after the original AD studies were published. We look forward to being inspired by lessons learned from a leading integrated health care system’s ongoing commitment to improving the quality of care around opioid safety with clinical outreach education. The rest of our conference agenda draws almost entirely from proposals submitted by members of our NaRCAD network – we received twice as many proposals this year! We’re looking forward to our “Field Presentations” sessions, featuring empiric results from detailers on the ground; expert panelists from the CDC, state departments of public health, and clinical care sharing important impressions on clinician stigma on the critical issues of HIV prevention and opioid safety; and breakout sessions covering many of the practical issues and challenges that detailers face when bringing best evidence to clinicians. Of course, for many of us, the highlight of each conference is the annual update from Jerry Avorn on the state of AD--see his recent blog piece, “Who Do You Trust?” for a preview of what’s to come!  The NaRCAD team is excited by the knowledge that integral opportunities, connections, and partnerships will be created at our unique 2-day event. But as excited as our team and our extended community may be about the conference, it’s not the only terrific development underway at NaRCAD this fall. We’ve continued to provide training and support for groups from around the country and the globe, with 2 trainings in the techniques of AD this past September, and more planned this fall and winter! Keep your eyes on our Training Series page for the official announcement of our Spring 2018 AD techniques training, and contact us at any time about opportunities and resources to support your AD program. See you soon, -Mike Biography. Michael Fischer, MD, MS, NaRCAD Director
Dr. Fischer is a general internist, pharmacoepidemiologist, and health services researcher. He is an Associate Professor of Medicine at Harvard and a clinically active primary care physician and educator at Brigham & Women’s Hospital. With extensive experience in designing and evaluating interventions to improve medication use, he has published numerous studies demonstrating potential gains from improved prescribing. Read more. Year One of Colorado Department of Public Health & Environment’s Detailing Program Guest Blogger: Deborah Monaghan, MD Public Health/Academic Detailer Colorado Department of Public Health and Environment NaRCAD Training Alumnus Tags: Detailing Visits, HIV/AIDS, PrEP, Training As the first and only detailer hired by the Colorado Department of Public Health and Environment, which serves 5.6 million people (about 3 million of which cluster around one metro area), the idea of building a detailing program from the ground up was incredibly exciting…and daunting. From the outset, it was important to determine the place of detailing within the community and establish its fit in the department’s mission. Shortly after joining the team, I presented the intended scope of my work at a department meeting--and it generated tremendous interest in the use of academic detailing for public health initiatives far beyond the current planned intervention. This served to solidify the potential value of clinical education outreach to leadership throughout the department. Lessons learned are continually surfacing as we move into year two, and a few key concepts are worth sharing. 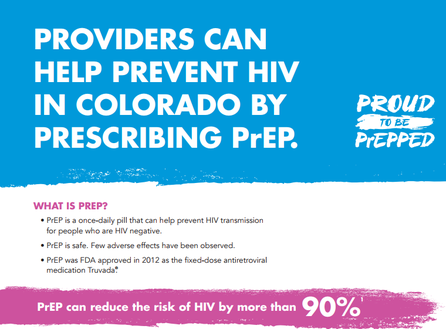 Particularly in the early stages of program establishment, it was essential to stretch resources and leverage partnerships. NaRCAD connections with other detailing programs facilitated the exchange of print resources, protocols and lessons learned, saving valuable development time. Through CDC-funded capacity building visits, I shadowed detailing teams at two other health departments' AD programs (San Francisco Department of Public Health and the New York City Department of Health & Mental Hygiene), which provided a framework for our own program’s function. At every opportunity, I presented our detailing goals to community partners and stakeholders, resulting in many connections to medical providers, which, in turn, generated most of our initial provider visits. Submitting articles for local clinical practice newsletters and magazines also established recognition and trust in the state’s new detailing initiatives.  Once provider-facing detailing visits began, two things became quite clear: Providers crave connection to their public health department. Providers want regional data. In a state with both urban and rural/frontier areas, urban clinicians wanted to be seen as “boots on the ground” to impact large populations by treating their own patients, while rural providers wanted to be acknowledged as part of the team and directed to resources they could access remotely. All clinicians, both urban and rural, wanted the latest disease and health data for their county, zip code, and even census tract level to compare to the rest of the state. It has taken multiple attempts to get in the door in many practices. However, after a detailing visit, most providers are outspoken that they found the session worthwhile, and we've used this opportunity to ask for referrals to other providers who might be open to visits. The time investment has also enabled two-way communication allowing us to get a “finger on the pulse” of regional health and disease, particularly in the more rural areas. The initial time invested to establish relationships with providers was high, but the rate of return has justified the investment. With a new detailing program, the responsibility falls to the detailer to establish credibility, both in resources provided as well as in value for time spent.  If I were starting a detailing program again, or could support new programs who were just getting started, I would love to be armed with these lessons learned: Establish as many protocols, procedures and resources as possible. Just start! Even if every detail isn’t in place, start visiting with providers. (The steep learning curve of on-the-ground visits is incredibly valuable and will continue to shape and improve your methods.) Document everything! As methods change and processes improve, document what is changing and why. Document with the goal of sharing not simply a starting point and a finished product but an entire story. Be willing to adjust in real time. Providers will have varying needs from one to another and from one day to the next, and our flexibility will ultimately strengthen the relationships we are trying to build, allowing academic detailing to have the greatest possible impact. Biography.
Deborah Monaghan, MD Public Health/Academic Detailer, Colorado Department of Public Health and Environment Deborah joined CDPHE in 2016 as the Department’s first detailer and currently provides clinical outreach on HIV prevention and sexual health. A graduate of the University of Mississippi School of Medicine, internship took Deborah to Drexel University in Philadelphia, Pennsylvania followed by residency at St Mary’s Hospital in Grand Junction, Colorado. She will complete her MSPH through the University of London School of Hygiene and Tropical Medicine in 2018. Initial response from the provider community receiving detailing has been overwhelmingly positive, and Deborah hopes to facilitate expansion of detailing efforts into other branches of public health to impact more Coloradans. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|