|
Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Stigma, Evidence-Based Medicine, Health Disparities, Conference Missed our event? Check out the AD Summit videos and materials on our Summit Hub.  We’re fresh off of the excitement of hosting our Academic Detailing Virtual Summit, “A Deeper Understanding of Our Impact on Patient Care.” In prioritizing patient-informed care more than ever before, we explored patient narratives through live interviews, workshops, and special panels, all within a virtual space. Innovations included AD for criminal justice involvement, care delivery redesign for veterans, affirming care for transgender and nonbinary people, and patient-informed communication on sex positivity in HIV prevention. Take a peek at some of the highlights from our event below! AD Fireside Chat: A New Spin on a “Keynote Address” We opened our AD Summit with a real-time interview featuring the originator and co-founder of NaRCAD, Dr. Jerry Avorn, and the National Director of the Veterans Affairs Pharmacy Benefits Management Academic Detailing Service, Melissa Christopher. Audience members were excited to throw ideas around and ask questions about:
Program Development Workshops: Attendees Led the Charge! Our revamped course catalog of workshops invited attendees to be in the director’s seat, as well as behind the scenes as co-creators in small groups. Participants created resources that we’ve published on our website and social media channels, sharing creativity and expertise with the larger AD community. Our workshops covered a wide range of topics including:
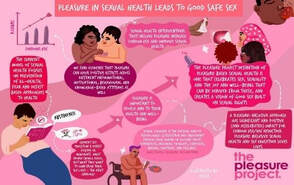 The Pleasure Project The Pleasure Project Special Panel: Understanding Critical Care Needed for Formerly Incarcerated Patients The outstanding team from New York City Department of Health and Mental Hygiene (NYCDOHMH) shared their groundbreaking detailing campaign, “Public Health Detailing for Criminal Justice Involvement”, with an audience that was hungry for innovation around inclusivity. The NYCDOHMH team shared NYC clinicians’ understanding of formerly incarcerated patients’ care, including clinicians who met the campaign with stigma, and those who were grateful to see such a campaign being implemented. Best Practices Spotlight: Prioritizing the Patient Experience For the first time in NaRCAD’s history, we highlighted leaders in the field who’ve been prioritizing the patient experience. The San Francisco team created space for conversation and discussion about gender-affirming care and ways to encourage safe clinical environments for transgender and nonbinary individuals through language, storytelling, and community outreach. We also heard from the Arizona team about the importance of pleasure being part of a patient’s sexual health history and the role of a detailer in supporting these conversations between clinicians and patients. 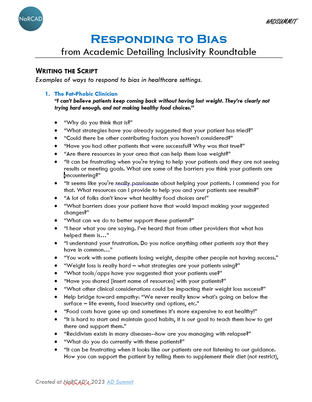 Inclusivity Roundtable: Real-time Script Creation We wrapped up our AD Summit with a roundtable session where attendees co-created a scripting resource to empower detailers to combat stigma during visits. We asked attendees to come up with responses to the stigmatizing comments below. A five-page resource was created in 60 minutes! 1. “I can’t believe patients keep coming back without having lost weight. They’re clearly not trying hard enough, and not making healthy food choices.” 2. “I don’t want those patients at my practice. They’re so difficult to handle and are really just looking for another opioid prescription. Treatment won’t work for them.” 3. “I’m so tired of keeping up with all these different pronouns. You’re either a man or a woman. It gets in the way of providing care.” 4. “I don’t need to use an assessment tool. I can always tell when someone’s at high risk of contracting HIV.” We want to continue these conversations, hear about your team’s innovations, and share resources in person this fall at our annual conference in Boston, MA. We hope to see you there! -The NaRCAD Team A special thank you to all of our AD Summit attendees and presenters as well as our partners at the Agency for Healthcare Research and Quality. For more information on our presenters, you can view the AD Summit Program Book. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation! Curated By: Aanchal Gupta, Program Coordinator, NaRCAD Tags: Stigma, Primary Care, Data Time and time again we’ve heard about the challenges detailers face when tackling clinician stigma. Detailers have shared comments from clinicians such as, “We don’t take those types of patients” or “I don’t want to be known as the gay doctor.” Addressing stigma and fostering understanding with clinicians can often feel overwhelming for detailers. In this edition of “AD-vice” we shine a light on these issues and share experiences from our community on how they managed stigma during detailing visits.  Understanding Stigma
 Addressing Stigma through Education and Conversations
 Addressing Stigma through Data and Resources
Our team at NaRCAD is here to learn and support you as we combat stigma and continue to promote inclusivity. Check out our new Healthcare Inclusivity Toolkit for detailers for additional resources.
Best, The NaRCAD Team Tags: Conference, Detailing Visits, Stigma Take a peek at the NaRCAD2022 conference materials on our Conference Hub.  Earlier this month, our team at NaRCAD hosted the 10th annual International Conference on Academic Detailing, “Celebrating 10 Years of Community Engagement.” We hopped on the virtual AD bus and heard from programs from across North America and beyond. This year, the conference featured campaigns focused on menopausal hormone therapy, initiation of antiretroviral treatment (iART), falls prevention, COVID-19, biosimilars, antiracist health care, polypharmacy, and opioids. The theme of community engagement was seen throughout the entire 3-day event, and we’re thankful to everyone who joined from around the world. Check out some of the highlights from our 2022 conference below.  Welcome Addresses:
Field Presentations:
 Breakout Sessions:
Expert Panels:
Special Presentation: “Looking Inward: AD as an Intervention for Antiracist Health Care”:
Real-time Roundtable:
 Thank you for all your engagement and support throughout the last 10 years of NaRCAD annual conferences! We are humbled to see how much the AD community has grown and are excited to be able to feature innovations at our conferences that have informed your work over the years. Our team at NaRCAD will continue to provide space for everyone to come together to share ideas, ask questions, and network. We look forward to seeing you in 2023. -The NaRCAD Team A special thank you to all of our NaRCAD2022 presenters as well as our partners at the Agency for Healthcare Research and Quality! Check out the NaRCAD2022 program book for more information on the presenters. Have thoughts on our DETAILS Blog posts?
You can head on over to our Discussion Forum to continue the conversation!  This series features tried-and-true practices from our AD experts. This week’s guest blogger is Zack Dumont, BSP, ACPR, MSPharm a NaRCAD Facilitator and Academic Detailer at RxFiles Academic Detailing Service. Curated by Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Detailing Visits, Stigma, Training  Model the compassion you expect from others. In recent years, the academic detailing community has been trying to recognize the harmful role of stigma in many clinical settings and to include stigma reduction in our detailing messages. In applying this framework, we encourage an empathetic view of people who experience stigma. They don’t choose to have addictions, exhibit certain behaviors, or to be ‘villainous’. We can all agree they don’t deserve harsh judgment and criticism. I invite you to bring forth your most charitable mindset for a moment and apply that same framework when you encounter stigma during a detailing visit. Imagine that the clinicians or people you detail hold stigma not because they want to stigmatize others, but for some more relatable reasons: they’re impressionable, they’re naïve, they’re vulnerable. In the same way that a clinician wouldn’t expect someone with a substance use disorder to suddenly recover if harshly confronted, we can’t expect the person who stigmatizes to respond to similar tactics. Be patient, be persistent (after all, you care and want them to be their best selves), and be persuasive with those that you’re detailing. You have a lot of natural talent, training, and experience to efficiently help people make informed decisions through detailing visits. Don’t limit it to therapeutic decision-making; extend it to the mental and emotional aspects of care, as well.  Balance and refine your self-reflections. Alone or with a colleague, find a quick and easy way to debrief after each visit – save the more intense feedback for quarterly or annual reviews. Maybe it’s asking two simple questions like, “What went well?” and “What could have gone better?” and taking a moment to reflect on each. And, just like AD visits which are 90% prep and 10% execution, the more the better when it comes to ‘prepping’ your self-reflection questions. So, “What went well?” could be more specific to one of your strengths:
Your “What could have gone better?” question could focus on an area of improvement unique to you:
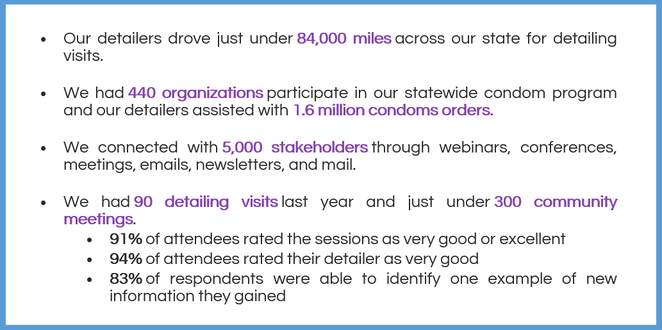
This isn’t easy, but it’s low risk with the potential for big reward… so I encourage you to jump in! Want more tips? Stay tuned for the next installment in our Words of AD Wisdom series, and reach out to the NaRCAD team, subscribe to our network, or check out our discussion forum to hear more tips and ways to train your brain!  Biography. Zack is a clinical pharmacist with the RxFiles Academic Detailing Service in Regina, Saskatchewan, Canada and an expert facilitator for NaRCAD's training courses. He has been involved with the RxFiles since 2008, with experience in both academic detailing and content development of RxFiles’ evidence-based drug therapy comparison tools. Zack also serves as the Clinical Manager for the Saskatchewan Health Authority Pharmacy Department. His practice has largely been hospital-based, with more specialized experience in anticoagulation and heart failure. His professional interests include evidence-based medicine, information technology, and leadership. Zack graduated as a Pharmacist from the University of Saskatchewan in 2008. Following graduation, he completed a hospital pharmacy residency with the Regina Qu’Appelle Health Region. He also completed a Master’s degree in Pharmacy, with a focus on leadership, from the University of Cincinnati. By Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD An interview with Lexie Hach, Regional Health Specialist, Bureau of HIV, STD, and Hepatitis, Capacity Extension Program, Iowa Department of Public Health. Tags: Detailing Visits, Evidence-Based Medicine, Stigma, Rural AD Program  Anna: Hi, Lexie! We’re excited to chat with you today about your detailing work in rural Iowa. Your program started about 5 years ago and was born out of the HIV and Hepatitis Community Planning Group (CPG). Can you share more about the CPG and how the detailing program was created? Lexie: The CPG is made up of healthcare providers, people with lived experience, case managers, educators, and other stakeholders. The group serves in an advisory capacity to the Bureau of HIV, STD, and Hepatitis at the Iowa Department of Public Health (IDPH) and their main task is to ensure that the state has an inclusive participatory planning and evaluation process for the delivery of prevention and care services. About 5 years ago, the CPG recognized a need for more education in the rural parts of Iowa related to best practices in HIV, sexually transmitted infections (STIs), and Hepatitis. That’s when we learned about AD. We started building our detailing program based on a lot of the work that New York City’s program was doing. We now have 5 detailers, who we call Regional Health Specialists (RHS).  Anna: What an interesting start to your program! You’re currently assigned to detail in 15 counties in central Iowa covering over 20 sexual health topics, from stigma to your statewide condom program to new screening recommendations. Do you detail on these topics beyond the primary care setting? Lexie: Yes! Our goal as detailers is to provide the best health outcomes for people living with HIV and those living with, or at risk for, STIs and Hepatitis C. We meet with the medical community including, local health departments, community-based corrections, substance use specialties, mental health, and many community based organizations. We also attend a variety of community meetings. We know that many people living with HIV pass through community-based organizations. We want to make sure that those organizations are equipped with the correct information to get people the care they need through resources or referrals. Our team has created detailing materials for both medical professionals and community-based organizations to maximize our impact. Anna: Working with community-based organizations is a great way to make sure people have access to the best possible prevention and care, especially in a rural state like Iowa. How does Iowa’s geography impact your detailing work?  Lexie: Iowa has 3.1 million people with about 54 people per square mile. Our state is 85% farmland with country roads, winter weather, and a lot of construction. It is not uncommon to lose cell service or your GPS signal while driving in the very rural parts of Iowa. We’ve adapted our detailing approach because of this and have found that group sessions work best for us. We identify champions in the clinics and are then able to set up 1:1 visits with clinicians as needed. Anna: We often hear from programs that group detailing is a great way to get your foot in the door and spread the word about AD. It’s nice to know that it’s working so well for your program too! I imagine Iowa’s geography also impacts patient care. Lexie: Yes, it does. There can be stigma around seeking sexual health care in rural parts of Iowa. Many times, patients know someone working at the clinic in their town. It’s common for patients to travel long distances to get to a clinic where they don’t know anyone. It’s also common for patients to have to travel over 2 hours to access HIV care at a specialty clinic. Anna: And that’s 2 hours one way! Has your program been able help with increasing access to care? Lexie: Yes, I can share one story that stands out the most to me. A couple of years ago, I was presenting at a community meeting with 15 or so people in attendance. The CEO of a federally qualified health center (FQHC) in Southern Iowa was also present and we were able to connect and network afterwards. We talked about how far patients must travel for Ryan White HIV care and he saw a need that the community health center could fill. We connected with senior leadership, there were additional meetings, and together we were able to bring Ryan White HIV care services to the health center. Those services are still there today and now people living with HIV in Southern Iowa can access Ryan White services closer to home. Anna: There is so much to be said about the power of AD, networking, and champions! Let’s wrap up with hearing about some of your program’s successes from this past year. Lexie: We’re so proud of all that we’ve accomplished this year! Here are some highlights: Anna: Those are some impressive numbers across both the clinical and community settings. Thank you for letting us feature your detailing work and learn more about the impact your team is making in your state! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Lexie Hach holds an Associate Degree in Nursing, Bachelor of Arts degree in Health Promotion and Women’s Health, and a Master of Arts degree in Community Health Education. Lexie is currently a Doctoral student in Public Health (DrPH) with an Epidemiology concentration at the University of Nebraska Medical Center (UNMC). Lexie has held positions in nursing, health education, public health, and healthcare marketing. Lexie has been with the Bureau of HIV, STD, and Hepatitis Capacity Extension Program at the Iowa Department of Public Health for over five years as a Regional Health Specialist (RHS). Lexie was previously with the bureau as a Disease Intervention Specialist (DIS). Lexie was instrumental in developing and implementing the RHS program in Iowa’s rural communities. In her RHS (academic detailing) role, Lexie educated a variety of different stakeholders on best practices related to HIV, STIs, and Hepatitis in central Iowa. Lexie has helped support the Sexually Transmitted Disease (STD) Program as a DIS due to COVID-19 and also helped as a COVID-19 contact tracer. Lexie was the previous workforce health department co-chair for Iowa’s statewide strategic plan to stop HIV in Iowa (Stop HIV Iowa). Lexie recently returned to her roots in the STD program and now serves as an Integrated DIS and Special Projects Coordinator, but continues to work alongside her fellow RHS colleagues. By Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD An interview with Trish Rawn, BScPhm, PharmD, Clinical Service Director and Academic Detailer, Centre for Effective Practice (CEP). CEP is a not-for-profit in Canada that aims to close the gap between evidence and practice for healthcare providers. Tags: Stigma, Detailing Visits, Substance Use  CEP's COVID-19 Resource Centre CEP's COVID-19 Resource Centre Anna: Hi Trish! Thanks for joining us today. Your team has been working on a number of AD campaigns including, falls prevention, type 2 diabetes, benzodiazepine use in older adults, chronic non-cancer pain (CNCP), and opioid use disorder (OUD). Can you tell us about some of the other recent work you’ve been doing at CEP? Trish: Our team’s academic detailing work is a big part of what we do, but CEP has other supports as well. We create clinical tools and resources on myriad clinical topics where practice gaps have been identified. Our most popular resource has been our COVID-19 Resource Centre to support primary care clinicians in adapting their practice during the pandemic. It’s become a massive resource that has had over 140,000 downloads. Anna: Wow! That’s an impressive amount of downloads. One of the other priority areas where your team has identified practice gaps is OUD. This topic often has a lot of stigma associated with it. Is this something you’ve experienced with the opioid detailing campaigns?  Trish: When we first started detailing on CNCP, opioid tapering, and OUD, there was a lot of fear and stigma among clinicians. They didn’t want to be known as the doctor “prescribing all the opioids.” Some clinicians were concerned that they might get in trouble, and they’d say things like, “I don’t have any of those patients” or “They’re all inherited patients.” Clinicians also sometimes felt like they didn’t want to say the wrong thing to patients, so they wouldn’t say anything at all. We’re all guilty of this and we’ve tried to encourage language like, “Hey, I might be saying the wrong thing here, but let's just start the conversation.” Anna: Just starting the conversation with the right intentions is helpful, even if you don’t get the language completely correct. Have you seen any stigma at the patient level? Trish: We found that patients themselves were experiencing stigma when seeking help and when trying to talk openly about opioids with their clinicians. Family doctors are in a vital position to help patients because they tend to have long-term, trusting relationships with them; they have sometimes taken care of them since they were children. Studies show that when opioid replacement therapy is prescribed by family doctors, there are improvements in patient uptake, patient satisfaction, and treatment success. We wanted to get the clinicians to a place where they felt confident talking with patients about opioids and where their patients felt comfortable sharing their experiences. It may feel like a jump for a clinician to go from, “I'm here to measure your blood pressure and adjust your medications” to “Let's talk about opioid addiction and set goals around tapering.” 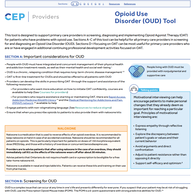 CEP's Opioid Use Disorder Tool CEP's Opioid Use Disorder Tool Anna: I can see how talking about OUD might make some clinicians feel uncomfortable. What types of resources has your team developed to support both clinicians and their patients to feel more comfortable having these conversations? Trish: For our academic detailing visits on opioids and CNCP we developed a resource called Talking Points with Patients, which includes scripts for clinicians to handle different scenarios. For example, one of the scenarios is about a patient asking for a dose increase for an opioid, but the clinician not agreeing that a dose increase will help manage their pain. We also have a Specific, Measurable, Achievable, Relevant, and Time-Bound (SMART) Goals resource to help clinicians set goals with their patients by taking the focus off the pain number scale and focusing on actions like, “What activities would you like to do if you had less pain?” Anna: It’s clear that your team works hard to develop and tailor resources to support clinicians and patients. What kinds of local resources from your community are available for detailers to share with clinicians? Trish: We often help clinicians find local resources through a program called The Healthline, which is a website that connects patients with social supports, like counseling, food, and safety. We’re also lucky to have Rapid Access Addiction Medicine (RAAM) clinics in our community that are a one-stop shop for patients with OUD where they’re assessed, given support and a plan for tapering, and referred to other community services. Anna: It’s so important for clinicians and patients to be linked to local resources and know that they have a community supporting them. Can you share some data about how clinicians reacted to the opioid-specific campaigns overall?  Trish: Absolutely! I can share some key findings from our opioid campaigns. Opioid therapy for CNCP AD campaign (n=475): After the detailing sessions, clinicians indicated they were confident in their ability to have a conversation about tapering when appropriate, even when the discussion was challenging (93.5%). Non-pharmacological and non-opioid alternatives for CNCP AD campaign (n=323): Clinicians indicated that after the detailing sessions they were confident in their ability to help patients:
OUD AD campaign (n=250): Clinicians indicated that the detailing sessions enabled them to support patients with OUD by:
Anna: That’s incredible. It’s obvious that your campaigns have made a huge impact on clinicians. What advice would you give to other AD programs who are supporting clinicians in reducing stigma, especially as it relates to opioids? Trish: I would recommend remembering three key points: Examine your own biases: When developing detailing tools, you need to make sure that you’re aware of your own biases and that your tools include the lens of equity, diversity, and inclusion. This is something we are actively working on incorporating in all our work at CEP. Make space for clinician experiences: It’s important to remember to be sensitive to the clinician perspective. There have been times, especially with opioids, where clinicians have had painful experiences with patients overdosing. Be aware of their perceptions and respectful of the trauma they may have experienced. Know your patient population: Understand who the patients are, the trauma they’ve faced, and the stigma they may endure. Look at the experiences of your team, the clinicians, and the patients you’re working with and try to understand how these different perspectives all influence one another as you develop your resources. Anna: That’s beautifully said, Trish. Thank you so much for sharing about your important work in reducing stigma around OUD. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Trish Rawn is the Clinical Service Director for the Centre for Effective Practice Academic Detailing Service. She is a hospital pharmacist who has been detailing for 6 years on topics such as antipsychotics in the elderly, opioid tapering, chronic pain, diabetes, falls prevention, and benzodiazepine deprescribing. Aanchal Gupta, NaRCAD Program Coordinator Tags: Conference, Detailing Visits, Stigma, E Detailing, Opioid Safety Take a peek at the NaRCAD2021 conference materials on our Conference Hub.  Fresh from our move to Boston Medical Center, our team at NaRCAD hosted the 9th annual International Conference on Academic Detailing, a virtual event concentrating on “Cultivating Relationships for Community Resilience.” There were robust discussions on critical topics, useful tools shared, and connections built. With over 300 registrants from across the globe, the AD community continues to learn and grow thanks to your support and passion for this work. Check out some of the highlights from our 2021 conference below. Day 1 + 2 Welcome Addresses
Field Presentations
Breakout Sessions
Expert Panels
Special Presentation: “Detailer Training in Action: Ask the Experts”
Real-time Roundtable
 Our team at NaRCAD is immensely grateful for your continued feedback and insights during our conference. This community has a wealth of knowledge to share, and as we approach 2022, we plan to continue to facilitate opportunities to connect you with others in the field, create a space to have conversations about stigma, and support your needs in the field. We look forward to seeing you in 2022. -The NaRCAD Team A special thank you to all of our NaRCAD2021 presenters! |
| Elisabeth Fowlie Mock, MD, MPH, FAAFP is a self-employed Family Physician consultant living in Holden, Maine. She attended Vanderbilt Medical School and obtained a Master’s in Public Health at UNC-Chapel Hill. She is a clinical educator for the Maine state Academic Detailing program (MICIS) and Alosa Health in Boston. She is Board Certified in both Family Medicine and Addiction Medicine. Her part-time clinical work includes evening shifts as a hospitalist and prescribing at a high-risk, low-barrier buprenorphine clinic. She is passionate about women’s and girls’ basketball, travel, learning chess and singing. |
by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager
Tags: Hepatitis C, HIV/AIDS, PrEP, Rural AD Programs, Sexual Health, Stigma, Training
 Dr. Mizroch participating in a NaRCAD training
Dr. Mizroch participating in a NaRCAD training
Brandon: Absolutely. I was hired to do work around PrEP and PEP, detailing providers across the state of Louisiana, in 2017. Since then, my role has expanded and I promote education for providers about syphilis, congenital syphilis, and Hepatitis C. Our department now has 3 detailers, including myself.
Louisiana became the first state in the country to undergo an incredibly revolutionary Hepatitis C Elimination Plan, which has caused my detailing focus to shift. There’s been huge advancements in the drugs that treat Hepatitis C, but they’ve been inaccessible to much of the population due to cost. We negotiated a fixed rate price for Hepatitis C treatment and can now treat 100% of the population, compared to the 3% of the population we could treat previously. There’s been a big push to identify and train providers who’ve never previously treated patients with Hepatitis C. I’ve been leading the charge by getting the word out, running symposiums, and working with the marketing team that’s creating our statewide campaign.

Brandon: I try to blend a few different approaches together. I attended the NaRCAD training during my first year as a detailer. NaRCAD built the foundation of detailing for me. I always use the NaRCAD methodology to get my foot in the door and identify providers who can be champions within their practices. I find it much easier to follow up and do longer didactic sessions about complex clinical topics when I use the techniques of academic detailing during my first face-to-face visits with providers.
I connect with about 20 providers in this 1:1 model each month. I also work with residency programs, hospital systems, and present at Grand Rounds to expand my reach. There’ve even been instances where I’ve attended dinners for physicians that are hosted by pharmaceutical companies to network and identify new clinics that would benefit from detailing.
Brandon: Follow-up is incredibly important, no matter what approach is being used. I like to send an email after each visit that includes digital resources for both providers and patients. I also offer providers the ability to call, text, or email me because of the apprehension that exists around topics where the knowledge base is still growing. Maintaining relationships with providers also ensures that we have a strong provider network that we can continue to educate on other clinical topics down the road.

Brandon: Yes, there’s certainly a difference. The providers in urban areas tend to have a higher knowledge base when it comes to PrEP and syphilis, perhaps due to marketing efforts or higher patient loads. This makes starting the conversation a bit easier. Additionally, urban communities have access to navigators, who help with non-medical aspects, like transportation issues, lack of health insurance, and long commute times that all prevent folks from getting the treatment they need. Providers in urban areas are also busier and easily distracted during 1:1 visits, which can make detailing a bit difficult.
On the other hand, rural communities are quite the opposite. Providers tend to have more time in their schedules and are excited to sit down with somebody from the state office. They’re eager to learn, but there’s typically less of a knowledge base, making it slightly more difficult to start the conversation.
I’ve also learned about patient barriers as well, which affect access and provider care. Patients in rural areas are often friends or family with those throughout the community, including those who work at clinics. The notion that you would know the receptionist or provider at a clinic is enough to deter folks from seeking medical care around a topic like sexual health. To encourage access, our state has created a TelePrEP program that offers PrEP services to anyone via telemedicine. Consultations take place over the phone, labs are obtained at third party lab companies, and medications are mailed right to the front doors of patients. It was originally created to help folks in rural communities who face stigma-related barriers, but we’ve expanded the program across the entire state of Louisiana. It’s a great referral service that I can share with providers.

Brandon: It’s important to have several different ways of presenting information to the providers you’re detailing and to use varied approaches depending on the barrier(s) they’re facing. I typically focus on emotional connection, financial concerns, and the evidence and science behind the key messages I’m delivering. I’m also ready for provider resistance, and am prepared to address it, which is something I learned from NaRCAD.
When it comes to detailing over a large and diverse geography, it’s always necessary to plan ahead. My general rule of thumb is that however many hours it takes to drive to a location, that’s how many providers I want to meet with while I’m there. I typically try to use larger educational events, like meetings with clinics over lunch, as my anchor point for longer trips. After I have that scheduled, I search for smaller clinics around the area where I can meet with providers 1:1. It’s all about maximizing your time.

Brandon Mizroch received his MD/MBBS from the University of Queensland/Ochsner Clinical School Program in November of 2016. Since taking over as the PEP/PrEP Provider Outreach Specialist at the Louisiana Department of Health in August, 2017, he has worked with hundreds of doctors statewide on HIV prevention best practice. Since then he has expanded his educational base and now serves as the head of the academic detailing department at the Louisiana Department of Health, Office of Public Health, STD/HIV/Hepatitis program. As the Provider Network Supervisor he has helped lead the provider Outreach for the state’s first-in-the-nation Hepatitis C Elimination program. From grand rounds presentations at LSU-Shreveport Hospital and Baton Rouge General, to state-wide symposia and conferences, to one-on-one counseling encounters at dozens of clinics all over Louisiana, he has helped spread awareness and education on HIV prevention, syphilis screening and treatment, and HCV screening and treatment through evidence-based care.
by Winnie Ho, NaRCAD Program Coordinator
Overview: The Cannabis Act went into effect in Canada in October of 2018. The legalization of a drug with strong potential for a myriad of clinical uses was followed by many questions from patients and providers alike about its effectiveness, its safety, and lack of previous research. The RxFiles have carried out a cannabinoid academic detailing campaign to address the demand for truth in a time where research has just begun to shed light on previous myths, misconceptions, and clinical promises.
Tags: Health Policy, International, Materials Development, Opioid Safety, Stigma, Substance Use

Zack: There’s an element of doubt in the information out there, because people have experienced misinformation before. People are often interested in the truth and that’s one of the most amazing things about academic detailing. There is also a desire for practical information that can be used to actually treat patients, and there’s a ton of overlap there. These things are important to these very, very busy providers who want the best for their patients.
NaRCAD: We know that your team is working on a cannabinoid campaign, which can be a nebulous topic. Can you discuss a little more about cannabinoid policy and conceptions in Canada?
Zack: We’re coming up on the one-year anniversary of recreational marijuana legalization, but medicinal cannabis has been legal for about two decades. With the legalization of recreational cannabis though, we’re seeing fairly rapid change in perceptions of what the truth is. It’s tough to keep up with.
With academic detailing, it was challenging to decide how to tackle it – can we just talk about the medicinal cannabis side? Or do we have to dive deeper? When we dug into it, it became clear that we also had to talk about the recreational side. For example, the people we provided our services to also wanted to know, “if I decline my patient cannabis prescriptions, what will they be able to get on their own?”

Zack: It’s coinciding with our work on pain, following our work on pain and opioids. In addition, because legalization was approaching, the providers had more questions because their patients were asking about cannabis as an alternative to opioids.
NaRCAD: How have provider responses been to the cannabinoid campaign so far?
Zack: It’s welcomed. Our information is usually welcomed. There’s some frustration over how little information there is out there. While frustrating, I think it’s kind of comforting to know that we’re not that far behind. It’s kind of mixed, but at the same time, they’re still happy to get information from a trusted resource. There's a lot of gray area information right now because it's a newer field.
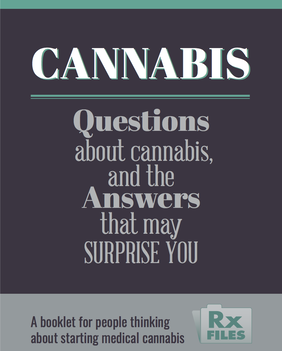
Zack: The evidence pyramid gives us the best approach for practical information, for people who are the interface of care. You want to find high quality, synthesized information. Whether its osteoporosis or COPD or pain or cannabis, you start with the guidelines and figure out what kind of information they are providing. We started with some recently published guidelines and it was a synthesis of systematic reviews, and made an attempt to summarize all the evidence of where cannabis was found to be of benefit. We also reviewed the bibliography with all the primary literature and metanalyses.
This process is pretty similar for any academic detailing topic. The other process is going to the people we provide services for, and asking what their patients are asking to treat with cannabis. They tend to ask about cannabis for pain, insomnia, or for things like tremors and that gives us some guidance in terms of what kind of literature we want to find. Of course, we are also looking into what the key messages are in the information we find and distribute. With cannabis, the interesting thing was the lack of information on the different conditions it could be used for. In some ways, it was easier, as weird as it sounds. We didn’t have as much reading to do on that topic.

Zack: One, you’re going to have your conversations about stigma. There isn’t a perfect picture of who uses cannabis and it could be absolutely anyone. You’ve got to have the conversation about stigma and get to know your own biases.
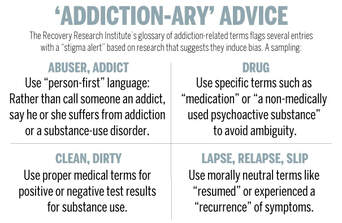
In the same vein, we thought about how important word choice and language is. We thought about whether or not we call it cannabis, marijuana, pot, or cannabinoids. Do we call it a medication or a product? All of those words and the considerations that we’ve given opioids - do we call them "addicts", or is it "dependence", and what are the differences between addiction and dependence? The third piece would be that you’ve got to talk to your providers in your local area and find out what their main questions are.
Your job is to provide a service, and if you can find out what their wants and needs are, you’ll provide a far more satisfying service for them and could establish strong relationships that you can build on. There will be a lot of information out there and you will need a lot of leads to help you sort through it all. This won’t be the last time we're addressing this.
NaRCAD: Thank you for taking the time to speak with us, and for leading the charge in bringing cannabinoids to the conversation about treatment for pain.

Zack Dumont is an clinical pharmacist with the RxFiles Academic Detailing Service in Regina, Saskatchewan, Canada and a new expert facilitator for NaRCAD's training courses. He has been involved with the RxFiles since 2008, with experience in both academic detailing and content development of RxFiles’ evidence-based drug therapy comparison tools. Zack maintains clinical practices for inpatient internal medicine, with more specialized experience in anticoagulation and heart failure. His professional interests include teaching evidence-based medicine, knowledge translation, development of clinical decision supports, collaboration, and leadership.
Zack graduated as a Pharmacist from the University of Saskatchewan in 2008. Following graduation, he completed a hospital pharmacy residency with the Regina Qu’Appelle Health Region, where he currently serves as a Clinical Support Pharmacist, with involvement in training new staff, precepting pharmacy residents and undergraduate students, and providing clinical support to various health region committees and working groups.

As we reflect on the two major public health topics we’ve been focusing on as we’ve traveled to public health departments across the United States, we’re learning that the public health detailers we’ve been training are discussing much more than just evidence with the clinicians they’re meeting. When we train new health educators on the methods of interactive, 1:1 education, we’re asked most often to customize our curriculum to cover two of the most highly stigmatized topics today: the opioid crisis, and HIV prevention. As the topic of stigma has come up at every straining we’ve implemented this year, our training team has added dedicated time to our trainings to discuss ways to address clinician stigma that arises during 1:1 detailing visits.
Thanks for reading, and please share your thoughts and experiences in the comments section below!
The NaRCAD Team
Optimism for the Opioid Crisis: Addressing Stigma and Disseminating Evidence to Clinicians
4/30/2019
by Kayland Arrington, MPH, Program Manager at NaRCAD
Tags: Opioid Safety, Stigma
 Don Teater role playing at an academic detailing training in Ware County, GA
Don Teater role playing at an academic detailing training in Ware County, GA Don: I was trained as a primary care physician, and my wife, Martha, is a behavioral health specialist. The two of us had an integrated-care model, where we did a lot of addiction treatment. I wanted to address that more specifically. An important part of my practice has always been to help those who couldn’t otherwise get help. I did medical work in Honduras, and then I realized that we had a large population of migrant farm workers where I lived in North Carolina. Most of these farm workers didn’t speak English or have a way to receive healthcare. With the help of others, I then opened a free clinic.
As far as addiction, I realized that so many patients initially became addicted from my colleagues and me prescribing opioids. The opioid crisis is a public health issue, and medical school doesn’t train you for public health work. Medical thinking addresses what is going on right now, but public health is so much bigger than that. I decided to get a master of public health degree at the University of North Carolina, and I completed that in 2017.

Don: Academic detailing can help by having more people with lived-experience do the detailing. In Wisconsin, people with lived experience are either going out with a detailer as a team or doing the detailing themselves. There is also a shortage of people treating OUD. AD is a great program for sharing how to get waiver trained to prescribe buprenorphine for OUD. AD lends itself well to the opioid crisis because it’s an area where little changes can make a big impact.
 Source: Harvard Gazette
Source: Harvard Gazette Don: I hear a lot from other clinicians that they don’t want “those people in my waiting room.” They are picturing someone who is all strung out on heroin on the street corner. We don’t get any education on addiction in medical school and the whole concept is overwhelming to clinicians. The best way to overcome stigma is for clinicians to have interactions with more people with OUD. I think that can be done by clinicians prescribing buprenorphine. I had to deal with my own stigma. For example, I had patients on opioids for chronic pain. I then found out they got arrested or were getting drugs from somewhere else, and I would just fire them from my practice. I saw them as bad people. Once I got trained to prescribe buprenorphine, I listened to their stories. I had made the same choices as many of my patients, yet they became addicted because of their personal history, social history, and genetics.
There’s also the importance of language. A lot of the older language around OUD identifies with bad choices and bad people. For example, relapse is associated with a fault of the person. When we are talking about a person with OUD, we are talking about someone with a disease and relapse is a natural course of the disease. When a patient’s blood sugar goes up, we don’t call it a relapse. Just like people with diabetes, we will never cure a person with OUD, but we help them manage.

Don: There is so much data that shows the first and best treatment for OUD is MAT. There are 11 criteria for OUD, and they are all behavioral. Once people get on the medication, they meet zero of the criteria for OUD. We don’t have many medications for other diseases that can do that. France had a big problem with heroin, and by making buprenorphine more readily available, overdose rates dropped by 80% in 2 years.

Don: We need to prescribe fewer opioids. A lot of our medical education is still driven by pharmaceutical companies. AD can help by disseminating the evidence on the appropriate treatment of pain. It was only in 2016 that the CDC first came out with guidelines saying opioids should not be the first line of treatment for people with chronic pain. It typically takes 17 years for research to become routine care, and there has already been a lot of uptake with this. Next, we should have all clinicians prescribing buprenorphine, like what France did. We also need to change our criminal justice system to reduce penalties for being found with a controlled substance, including heroin. I am optimistic about each of these things, and think they are all likely to be done in our lifetime – hopefully in the near future.
Don Teater, MD, MPH
Founder
Teater Health Solutions
Don Teater is a family physician who has lived and worked in western North Carolina since 1988. His work in the southern Appalachian Mountains made him aware of the problems with opioid pain medications years ago. In 2004 he started a clinic to treat those addicted to opioids in his primary care practice. From 2013 to mid-2016, he worked as Medical Advisor at the National Safety Council addressing the national epidemic of opioid abuse, addiction, and overdose. Dr. Teater was lead facilitator for the expert panel discussion during the development of the CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. Dr. Teater has also served on the World Health Organization Committee addressing drugged driving that met in Mallorca Spain in December 2015. Since June 2016, Teater has worked for Teater Health Solutions to concentrate on educating prescribers and others on the science of opioids and how that should influence treatment and policy decisions. Currently he contracts with the Center for Disease Control on the academic detailing of prescribers to educate them on the appropriate use of opioids for the treatment of pain.He continues to work one day per week treating those afflicted by the disease of addiction at Meridian Behavioral Health Services in western North Carolina.
Tags: Detailing Visits, Health Disparities, HIV/AIDS, Sexual Health, Stigma

Mary Nagy: I was an ER nurse for five years. During that time I worked all over the country in lots of different settings, but I noticed the same patterns playing out no matter what city I was in. I was seeing patients daily who were either in the last hours of their lives or needing immediate life-saving interventions as a result of medical problems that might have been avoided entirely through basic services or preventative medicine. The longer I worked ER, the more clearly I saw the effect of systemic forces and environment on health, their unequal distribution across society, and the more I wanted to find a way to work towards health equity.
I decided to study public health, and earned my master’s degree in Environmental Health Science at the University of Michigan. In addition to giving me the opportunity to design and carry out my own research, the program I did had a strong health policy component, which helped me add to the understanding of healthcare delivery I formed during the time I spent at the bedside.
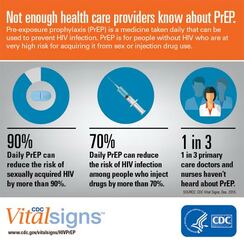
Mary Nagy: I saw the job posted and was immediately interested in it because I think detailing, especially on the topic of pre-exposure prophylaxis (PrEP), is a really effective way to strengthen prevention infrastructure and affect health outcomes. Clinicians are under a lot of pressure and I was drawn to the idea of being a source of relevant, high quality, trusted information.
The detailing program here in Michigan is comparatively young and its development is ongoing. Fortunately for me, lots of folks have been willing to help! I've drawn from a broad range of sources has been really helpful during detailing visits, because the needs of providers are so diverse; folks are asking about billing and coding for PrEP visits, standing orders, HIV risk assessment, nuts and bolts of services offered by our state lab, STI screening and trends, and financial supports for PrEP, best practices with PrEP initiation and follow up, and more. I’ve been working hard to broaden my knowledge base, but also to identify resources for questions I don’t know the answers to and topics I’m weaker on.
 Image from UNAIDS
Image from UNAIDS Mary Nagy: Even though I’m very new to the field, I think it’s a very exciting time to be doing this work because I do believe it is possible to end the HIV epidemic in the US within the next few decades. Racial and ethnic minorities continue to be underrepresented in PrEP utilization and overrepresented in new HIV diagnoses, and I want my work to contribute to correcting this. I think PrEP can be a tool for health justice and being part of that is valuable to me.
Mary Nagy: I think that’s where my mind goes, because I’ve seen the powerful effect of environment on health, and this is certainly true on a population level. I never want to diminish the power and agency of individuals, but everyone operates under multiple layers of forces. Examples of this include policy, especially the persistent legacy of overtly racist housing policies; the “war on drugs” and resulting mass incarceration; or a justice system that data shows us doesn’t work in the same ways for everyone.
These systemic forces, applied to millions of people over many decades, result in the disparities we see in HIV rates, overall health, wealth, and many other areas. Increasing access to PrEP means we can mitigate some risk for folks who might have more exposure due to the environmental context in which they live.
For Michigan, one of the ways detailing can help make PrEP easier to access is increasing geographic availability. A large portion of our state is rural, and many counties do not currently have a known PrEP provider. Another challenge is, of course, cost. The cost of PrEP and associated visits and screening tests is a policy issue, and while we hope and expect to see cost come down in the future, in the current landscape, it's important to prioritize educating providers and their staff on available financial supports and how to apply them, so cost doesn’t keep people who can benefit from PrEP from getting and maintaining access.
 Image: University of New Mexico
Image: University of New Mexico
Mary Nagy: Stigma around HIV and other STIs is a big issue. We know that when providers talk openly with patients about their sexual health, they’re better able to accurately assess risk for HIV and STIs and screen and treat appropriately, but those conversations are not happening with enough regularity. Rates of STIs like gonorrhea, chlamydia, and syphilis have been rising, and continue to increase, so there's a lot of opportunity there.
NaRCAD: How has detailing been received overall? Are providers open to education on PrEP?
When I think about why detailing is important and why I’m doing it, the first thing that comes to mind is a recent survey of primary care providers MDHHS carried out in Southeast Michigan. Providers were asked which supports would best help them to incorporate PrEP into their practice, and "education" was by far the most frequent answer. In addition to the research I’ve seen indicating detailing is an effective intervention to change provider behavior, it's clear that the providers themselves agree that education is important. If we can work with providers to make PrEP available and easy to initiate and maintain, the protection it offers from HIV can improve health outcomes for patients at high risk.

Mary Nagy, MPH, RN/BSN
Public Health Detailer, HIV Care & Prevention Unit
Michigan Department of Health and Human Services
Mary is the public health detailer for the State of Michigan and conducts direct outreach with medical providers to support HIV prevention strategies and stigma reduction statewide. She received her master’s degree in Environmental Health Science from the University of Michigan School of Public Health where as a Graham Sustainability Fellow her research focused on municipal water quality and affordability. Mary also has several years of experience working in as an Emergency Department RN in trauma centers across the US and her work in health equity is informed by her time as a frontline health worker.
Exercising Empathy, Planting Seeds: An Interview with the Manchester, NH Academic Detailing Team
10/26/2018
Jill MacGregor, APRN, Catholic Medical Center, & Katie Sawyer, LICSW, MLADC, Director, Integrated Treatment of Co-Occurring Disorders, Network4Health/Mental Health Center of Greater Manchester
Interview by Isabel Evans, Fellow, NACCHO, in partnership with NaRCAD
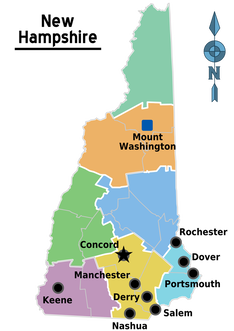
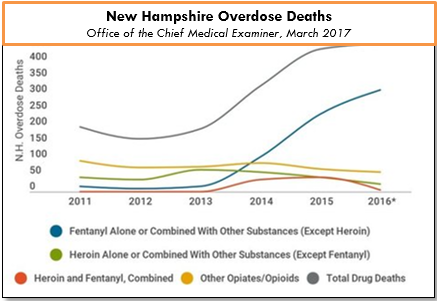
EDITOR'S NOTE: Manchester, New Hampshire, was the third site of four selected for a 2018 pilot program of the CDC (Centers for Disease Control and Prevention), NACCHO (the National Association of County and City Health Officials), and NaRCAD (The National Resource Center for Academic Detailing). This exciting pilot program focused on community-level work with local public health departments to develop customized interventions to reduce opioid overdose and death. Four sites experiencing significant public health problems related to opioids were selected to be trained in academic detailing; those trained health professionals then conducted 1:1 field visits with front line clinicians to impact behavior around prescribing, treatment referrals, and patient care, with Manchester’s team focusing primarily on access to Medication Assisted Treatment [MAT]. As year 1 comes to a close, we’re showcasing successes from the field.
Carol: Tim Soucy, from the Manchester Department of Health, contacted representatives at each of our organizations and gave a little bit of information about the training. He asked if our organizations had particular people that might be interested, and my supervisor thought of me, since I was in the middle of developing a MAT program for my organization. I jumped at the chance to participate.
Jill: My organization received the same email, and as the primary care lead nurse practitioner, I was considered the most appropriate to participate.
Katie: The invitation came from the site that received the CDC grant (City Health Department). The invitation was disseminated among a number of local human service/health agencies who are part of a Network of agencies as a result of our 1115 Waiver partnership.

Carol: I’m a naturally shy person who dislikes being the center of attention, so I was incredibly nervous about the role plays during training. The turned out to be invaluable, since I use the skills I developed through practicing and receiving feedback during every visit. The role plays prepared me so well for meeting with providers, and I go into the conversations feeling confident and comfortable. When they ask questions, I feel that I know how to answer, or where to turn for more information, such as the wonderful handouts available on the NaRCAD website.
Jill: For me, learning how to hold a discussion as a detailer was the most important element of the training. I learned how to frame a conversation using open-ended questions, which allows the discussion to progress. Understanding how to simultaneously get a provider’s perspective, while also giving them the information they need, is a critical detailing skill.
Katie: We were able to role play, which has proven very helpful out in the field to stay focused, on topic, and empathetic to the position of each clinician that I speak to. The handouts that NaRCAD provided have easy to read information and great graphics, so they have also proved useful for staying on track with the key messages during detailing visits, along with providing supplemental information.
Carol: Clinicians can be a little skeptical at first, since they’re often expecting that I’m going to try to “sell them” on something. When I focus on listening to their experiences and their concerns, I’m able to gently address those concerns and give resources or suggestions. Even just having a discussion can help clinicians to feel that you’re interested in how they feel, and that you genuinely want to help them – I would describe some clinicians as “dumbstruck” from our conversations, because they’re preparing to do battle with me, but they instead come to see me as a resource, and are more willing to meeting with me.
As for challenges, we deal with a fair amount of stigmatization of substance use. It’s a major barrier, and we’ve had to spend a lot of time addressing that in my organization. Another barrier for clinicians is a preconceived notion that providing MAT is an onerous process, and too time-consuming to add into their schedules. And these two barriers really complement each other in a bad way – I often get providers saying that MAT is too much work and that their MAT patients will just end up using opioids again and ending up back in the emergency room. Breaking down these misconceptions about MAT and getting to the root of the stigma against MAT is a big challenge.
However, we’re approaching these challenges with education and lots of conversations, since we’ve found that helping our staff to get a better sense of addiction as a disease is really invaluable to making them more open to MAT and treating people with opioid use disorder. The timing of the academic detailing initiative couldn’t have been better for my organization, because having conversations about addiction leads well into having conversations about MAT, and vice versa. Engaging in academic detailing has opened up a whole new avenue of clinician education for me.
Jill: Because of my role at my health system, I talk to providers about many different topics and they’re used to me approaching them, which has definitely helped give me and automatic “in” and bring up sensitive topics. My institutional knowledge helps too, since I can answer questions specific to my organization and our various programs or resources around opioids.
Providers will come to conclusions without getting the right education, and I find that they often “change their tune” when I give them more information. Providers are also hesitant about writing a prescription for a MAT patient if there isn’t someone in their office who can talk to the patient about addiction itself. Right now, we’re working on integrating behavioral health clinicians into primary care, which I’m hopeful will help with this very real concern.
Katie: There has been some hesitation in sharing with detailers, in regards to professional experience, as I believe most clinicians are on edge in trying to do the best that they can to address patient needs, while also supporting alternatives to typical or historical use of prescribed opioids. With an empathetic and interested stance, I’ve found that most clinicians are open with their experience and struggles.
There are a number of themes among clinicians for challenges that I’ve noticed, including a limited behavioral health workforce to support what they view as an ideal MAT protocol, which would include individual and group counseling, regular urine toxicology screens, and wraparound services along the continuum of care. In addition, there is a concern among providers about the potential diversion of Buprenorphine by patients.
|
"I would tell new detailers to take a deep breath and know that you’re ready for this. NaRCAD does such a good job of training us as detailers, and you just feel ready." -Carol Furlong, Academic Detailer |
What have been some of the best visits you‘ve had when you’ve met with clinicians 1:1?
Carol: A rewarding moment for me was hosting a small dinner for any staff member interested in hearing about MAT, because nine people from across the organization attended! There was a level of excitement that was really amazing, and everyone who attended left the dinner ready to get waivered, and to get their friends involved too. Other than that, I’ve had really memorable exchanges with clinicians who start out skeptical, but then become very open and grateful when they discover that my primary goal is to listen to them and their needs. They can be dumbstruck that I truly want to help them, and to find them the resources for them to be successful. |
Carol: I would tell new detailers to take a deep breath and know that you’re ready for this – NaRCAD does such a good job of training us as detailers, and you just feel ready.
Jill: I would say to recognize that everyone has a natural process for adapting to new ideas. You’ll get some providers who are ready and energized, some who will want to watch others in action before they jump in, and some who simply may not be interested. It can be frustrating when providers aren’t interested in your topic or resources, but understand that this is natural, and don’t take it personally! Every visit will be different, and that’s okay.
Katie: My advice is to remember that success is not defined as “convincing” someone that the topic of your detailing visit is “the right answer”. In fact, trying to convince another person of anything is essentially walking against waves. Instead, be open to listening to that person and their experiences, and then value the experience that they have had. This is more likely to open the conversation to allow you to share your wealth of information and experiences. It’s all about planting seeds.
Highlighting Best Practices
We highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond.
Search Archives
by Topic:
All
ADvice
Autism
Cancer
Cardiovascular Health
Chronic Illness
CME
Conference
COVID 19
Data
Deprescribing
Detailing Visits
Diabetes
Director's Letter
E Detailing
Elderly Care
Evaluation
Evidence Based Medicine
Expert Trainer Insight Series
Harm Reduction
Health Disparities
Health Policy
Hepatitis C
HIV/AIDS
International
Jerry Avorn
LOOPR
Materials Development
Medications
Mental Health
Obesity
Opioid Safety
Pediatrics
Podcast Series
Practice Facilitation
PrEP
Primary Care
Program Management
Rural AD Programs
Sexual Health
Smoking Cessation
Stigma
Substance Use
Sustainability
Training
Vaccinations