|
NaRCAD's Interview Series: Public Health Detailing Program at New York City Department of Health and Mental Hygiene (DOHMH) Featuring Michelle Dresser, MPH, Senior Manager, Programming & Strategy Tags: Detailing Visits, Diabetes, Evaluation, Obesity, Program Management, Smoking Cessation, Training  Thanks for taking the time to share the great clinical outreach education work that’s being done by the NYC Department of Health and Mental Hygiene, Michelle! Tell us a bit about yourself and how you got involved in public health, specifically public health detailing. Michelle: Thank you for the opportunity to speak about the Public Health Detailing Program. I have over 20 years of public health experience in both the non-profit and government setting, with the last 12 here at the New York City DOHMH. Throughout my professional career, my specialty has been in healthcare marketing and provider education, emphasizing how providers and consumers can better communicate with each other by tailoring complex messages using health literacy principles.
 An excerpt from DOHMH's obesity pocket guide. An excerpt from DOHMH's obesity pocket guide. It’s essential our reps have excellent selling and communications skills, so when they engage providers and get their buy-in, providers are then equipped to get their patients “on board”. One-on-one provider engagement helps them understand how important it is to have a 2-way communication with patients. How can an outreach representative encourage providers to “get on board” and think about care as a dialogue? Michelle: Let’s use obesity as an example. With obesity, both providers and patients are frustrated, for different reasons. Providers may be frustrated that patients’ comorbid conditions are being exacerbated or don’t have the same kinds of tools to treat obesity as they do other conditions; patients might feel that providers aren’t using great communication techniques, like motivational interviewing (MI), to help them set goals and take small steps towards the goal. If a patient is only told, “You need to lose weight,” which is such a broad and overarching goal, they’ll be frustrated, and frankly, non-adherent. I know I would be. 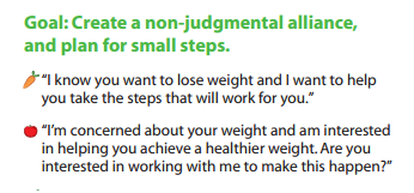 Example of a coaching script created by DOHMH. Click to learn more. Example of a coaching script created by DOHMH. Click to learn more. Encouraging providers to have specific dialogues using a customized approach for each patient is important. This kind of dialogue takes into account patients’ literacy beyond the written and spoken word—it looks at scientific, fundamental, health and cultural literacy, too. We work on “coaching scripts”, which take the key recommendations and reframes them in order to custom-tailor the conversation for each patient.
One thing that’s unique about public health detailing is that we detail the whole team through one-on-one interactions. Evidence shows these types of interactions with providers and staff are more effective at changing behavior; however, sometimes due to the makeup of the practice we must conduct group presentations. It’s not ideal, but it still allows us to get the messages and materials out there.
 A coaching guide designed by the NYC DOHMH to aid clinicians in smoking cessation support for patients. A coaching guide designed by the NYC DOHMH to aid clinicians in smoking cessation support for patients. So when an outreach representative goes into an office, they detail...everyone? Michelle: If there are 15 people who work in an office, we’re going to detail all 15 of them. It’s a lot! Sometimes, the person who is the champion of a new behavior or workflow isn’t going to be the provider. We see the front desk staff as instrumental; they’re interacting with all of the patients. We work with our teams to ensure even the front desk staff receives the materials and information, rather than seeing them merely as a “gatekeeper” to get to the providers. Sounds like a lot of training goes into preparing for your campaigns, and for thinking about the entire process of effective outreach. Tell us more about your trainings, and about how you prepare outreach representatives on disease content training, as well as in marketing and communications skills.  Click to view more Public Health Action Kits (copyright of NYC's DOHMH) Click to view more Public Health Action Kits (copyright of NYC's DOHMH) Michelle: On average, our trainings are about 5 days in length and take place the week prior to launching a new campaign. About 40 percent of the training is disease content, so we work with our internal Health Department experts, as well as external experts, where we learn about prevention strategies, treatment strategies, epidemiology and the landscape around the key recommendations chosen based on the evidence of that topic. We need to know the ‘why’ behind the campaign. Once we have that under our belt, we shift to sessions on how to frame the issue, how to promote the materials, figuring out the “features and benefits” as well as the “barriers and objections” and finally “gaining a commitment”, which are phrases that come from pharmaceutical marketing. We’re “selling” and promoting public health interactions, so we work on those skills. We also do a great deal of role playing, including videotaped analysis of each rep. We look at body language, what communication skills are effective, we do knowledge assessments, quizzes—we make sure our team is well-prepared to go out and detail. We take this seriously—they’re representing the New York Department of Health and Mental Hygiene.
 What’s a major barrier your program has faced, and how have you tackled it? Michelle: A big challenge, when starting a detailing program, is access. The landscape of healthcare systems in NYC has drastically changed over the past few years. As an example, several years ago, the majority of our Brooklyn territory was almost entirely made of up of small practices where access wasn’t an issue. What’s changed since then? Michelle: Now, many of these sites have become part of larger institutions, so there’s corporate buy-in that needs to happen for people to come in and talk to the staff. As I mentioned before, although we try and limit group presentations, this has proven to be an effective strategy when entering into a new relationship. Once they get to know us and recognize the value of the program, they’re engaged in having us come back to conduct 1:1 visits on the follow-up and subsequent campaigns. How do you know when a campaign is working and becoming successful? Michelle: Evaluation is always on the top of our priorities, and can be a challenge for any program to evaluate effectiveness. For every campaign we conduct an initial and follow-up visit where we assess provider practice. This allows us to see if there has been a change in practice from the initial to the follow-up visit. Additionally, we rate what providers intend to adopt in terms of the key recommendations and supporting tools and resources. We also collect a large amount of qualitative data because it's also critical to gaining a more complete picture of the campaign’s success, especially when reporting on barriers, access and materials.
You can scale this up or down, depending on your need and organizational priorities. Our program focuses on where there’s the greatest need and potential for greatest impact. Programs should make sure to look at their organization’s agenda and goals. It’s important to look at the data and plan the best course of action within the capacity you have. Biography: Michelle Dresser. Michelle Dresser is the Senior Manager of Programming and Strategy for the Public Health Detailing Program within the Bureau of Chronic Disease Prevention and Tobacco Control at the New York City Department of Health and Mental Hygiene. In this role, she oversees the overall programmatic direction and strategy of the program. This includes, campaign strategy and timing, campaign content, training and economic incentive development, provider selection, identification of targets to ensure the greatest impact on populations most in need, and identification of “new needs” opportunities to expand program reach and achievement of program goals. She also oversees internal and external strategic relationships to enhance programmatic objectives.
1 Comment
|
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|
