|
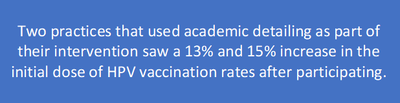
Overview: Dr. Nate Rickles, PharmD, PhB, BCPP, FAPhA is an associate professor pharmacy practice at the UConn School of Pharmacy with experience in developing AD programs, most recently for the CDC-funded CEDPP (Connecticut Early Detection and Prevention Program) project. Dr. Natalie Miccile, PharmD, MBA currently works as a retail pharmacy manager at ShopRite Pharmacy. She’s working with Nate to onboard pharmacies participating in the CEDPP program and working with the pharmacy students who are supporting the process of referring patients to screening, diagnostic, and prevention services. by: Winnie Ho, Program Coordinator Tags: Cancer, COVID-19, Detailing Visits, Health Disparities, Program Management  Winnie: We’ve been excited for a chance to speak with you both! Nate, you spoke on our Clinical Innovations in AD session at the NaRCAD2020 Conference, sharing your work to support underserved, and sometimes undocumented, women in accessing care. Thank you both for joining us today – can you tell us a little bit more about the program and the issues it addresses? Nate: CEDPP consists of two components: the Connecticut Breast and Cervical Cancer Early Detection Program (CBCCEDP) and the Well-integrated Screening and Evaluation for Women Across the Nation (WISEWOMAN). The services are offered free of charge with the goal of significantly increasing breast and cervical cancer services for medically underserved women. The Department of Public Health’s traditional outreach method of using clinical navigators at established WISEWOMAN sites could only reach a relatively small population. We received a CDC Innovation Grant to investigate the role that community pharmacies could play in increasing referrals to a free public health prevention program for vulnerable populations, as these pharmacies are accessible, front-line, and generally well-trusted in the community.  W: That’s an important goal to close this gap and to ensure more women can access the services they need. Why did your team feel that AD was a useful approach to address the lack of access to screening services? Nate: I’m very passionate about the notion that building relationships through 1:1 connections are going to be more powerful long-term in creating behavioral change. AD works so well because the techniques are very persuasive in dealing with common barriers like pharmacists believing there’s little time in their day, not enough staffing, or not the right financial incentive. Our project manager Peaches Udoma had sent out flyers and e-mails to local pantries and shelters, but we hadn’t received many referrals through this tactic. The predominant way we’re getting referrals is through 1:1 outreach with pharmacists and our students reaching out to the referred participants to connect them with services.  Winnie: Can you tell us more about how your intervention navigated the pharmacists’ barriers you described? Natalie: We had a lot of interest from pharmacists, especially when they learned about the impact they could have. However, for a full month, we weren’t seeing results. When I checked in, we learned that they were genuinely overburdened with their workflow, which wasn’t surprising. We had to think about who else in the office could do it – and it turned out to be the pharmacy technicians. They were often at the point of sale and would be more likely to know if patients were uninsured or underinsured. We began detailing the pharmacy technicians directly instead. Many of them were bilingual, which helped in distributing the right flyers to the right women. We worked with the pharmacy technicians on communicating the benefits our programs offered, with attention to utilizing accessible language and avoiding unnecessarily complicated healthcare terms. We learned that emphasizing key things like free gym memberships or free nutritional services provided was very useful in getting women to agree to be referred. Addressing the language barrier and slight language changes was key to us finally getting referrals. However, when COVID-19 hit, we had to reassess since we started getting zero referrals again. It made sense as few people want to wait around in a public space, and pharmacies also became overwhelmed. Our team pivoted to reaching out directly over the phone after receiving lists of potential contacts from the pharmacies. We wanted to show our partners that we could be resilient in this time and to not let this program fall through.  Winnie: Pivoting your intervention to have team members directly contact the women you were trying to refer instead of through the pharmacy technicians must have required your team to make adjustments to accommodate language needs. How did your team tailor the AD intervention to address language barriers? Nate: We noticed that we had many of the women we reached out to who spoke Spanish as a native language, and quickly realized we were probably losing a lot of patients because of the language barrier. We onboarded a pharmacy student, Isabella Hernandez, who, in addition to being a very dynamic, charismatic, and outgoing person, also spoke Spanish. Once Natalie onboarded her and shared the main concepts around the screening and referral, Isabella was quickly able to pull in over 80 referrals; we didn’t have even half or a third of that through our prior efforts. We’ve been closely tailoring our work since, with flyers in Spanish, Portuguese, and in Arabic. We have also Arabic speakers to communicate with Arabic-speaking patients, and we have the capacity to expand into other languages.  Natalie: I originally worked with the lists of contacts we received and tried to engage directly. However, because we recognized our bilingual pharmacy students were able to better engage with these women, my role now is to oversee our callers, get their referrals, and help touch base with site navigators to ensure referrals are being processed, and how we can improve our screening process. We’re prioritizing language accessibility because our first encounters are first impressions. Our patients matter, and we want to make things as smooth as possible for them. We’re even at a point where Isabella is running trainings with our other callers, so she can give them hints on how to be more flexible in the conversation to fit our clients’ needs. Winnie: This is a really outstanding demonstration of flexibility and tailoring a program to address barriers to practice change. We hope that other programs continue to follow your example of integrating best practices to communicate with patients from diverse communities! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Nathaniel ("Nate") Rickles is an Associate Professor in the Department of Pharmacy Practice at the University of Connecticut School of Pharmacy. He received his B.S. in psychology and chemistry from Dickinson College, Pharm.D. from the University of the Sciences in Philadelphia, M.S. and Ph.D. in the Social and Administrative Sciences from the University of Wisconsin-Madison. Dr. Rickles also completed a psychiatric pharmacy practice residency and is board certified in this area. He was inducted as a Fellow of the American Pharmacists Association. His primary research interests are to develop, implement, and evaluate intervention programs that improve pharmacist communication with patients and/or other team members and subsequently to improve medication adherence and patient safety. Primary teaching interests involve courses on communication skills, mental health, health behavior change, cross-cultural health care, and research methods. Dr. Rickles is an active researcher with several grants and publications involving enhancing the role of pharmacists in changing patient and provider behaviors.  Natalie Miccile received her PharmD from the University of Connecticut School of Pharmacy in Storrs, CT and MBA from the University of Connecticut School of Business in Hartford, CT. Her MBA concentrations include Digital Marketing and Strategy and Investment Analysis. She works as a consultant for UConn School of Pharmacy on research initiatives that involve enhancing the role of pharmacists in the community setting and is pharmacy manager at Shop Rite Pharmacy in Milford, CT. Dr. Miccile is MTM certified and an active member of the Connecticut Pharmacists Association. An interview with Lisa Gruss, MS, MBA, Practice Transformation Project Lead, Quality Insights. Quality Insights is a non-profit organization that is focused on using data and community solutions to improve healthcare quality. The organization is based out of West Virginia and operates in Delaware, Pennsylvania, Virginia, and New Jersey. Quality Insights has developed an innovative academic detailing campaign to increase human papillomavirus (HPV) vaccination rates across Delaware. by Anna Morgan, MPH, RN, PMP, NaRCAD Program Manager Tags: Cancer, Detailing Visits, Vaccinations  Anna: Hi Lisa! We’re looking forward to learning about your academic detailing work as a multi-state non-profit, and your important work around HPV vaccination rates. We know these vaccinations are critical in preventing HPV, which can lead to many types of cancers. Can you tell us a little bit more about your current role and how it relates to academic detailing? Lisa: I’m focused on new business operations, science, and innovation. I implement new contracts that we receive through the Department or Divisions of Public Health, or any other funding sources. I also work with our Information Technology (IT) team to set up databases, work through any compliance issues, and define metrics. Additionally, I help manage the AD components of our contracts.  Anna: You’ve had great success with many of your academic detailing campaigns, specifically your HPV campaign that you’ve been working on. Can you walk us through how the topic was chosen? Lisa: We originally received a pilot grant through the Delaware Division of Public Health in 2018. The project was co-sponsored through their immunization program and the Delaware Cancer Consortium to improve the HPV vaccination rate in Delaware. According to the National Immunization Survey-Teen, the HPV vaccination rate for the initial dose in Delaware in 2018 was 73.9%. The Division looked at the relationship between cancer rates and low vaccination rates and saw a huge opportunity. Per the Centers for Disease Control and Prevention (CDC), 90% of the 34,800 HPV-related annual cancer cases in the United States could have been prevented with the HPV vaccination. The pilot was small but successful. In the spring of 2019, we received additional expansion of funding and added the academic detailing component. We’ve been working with practices to implement various services that tie in with academic detailing. We review data, work on evidence-based workflow modifications, provide HPV vaccination resources for staff and patients, and offer technical assistance.  Anna: Academic detailing dovetails so nicely with other interventions and services, creating more opportunities for impact and care improvement. It sounds like clinicians have been mostly amenable to the program—have any barriers come up throughout your HPV campaign? Lisa: To say we’ve had no barriers with access wouldn’t be true. We consider ourselves to be vendor neutral and ambassadors of the evidence - we don’t align and promote directly with any pharmaceutical company or insurance company. When looking at the broader scope of our work, it’s certainly complementary to what pharma might do, but we’re able to offer a broader menu of interventions beyond a vaccine. We’ve had some difficulty during the pandemic, like many AD programs, but we’ve found leveraging our past relationships to be key.  Anna: I’m sure those existing relationships have helped with building new ones. Have the practices that you’ve visited been involved in your program’s other academic detailing campaigns? Lisa: It’s a mix. The family medicine practices have been involved in a lot of our other projects, like opioid safety, cancer screening, prediabetes, diabetes, and maternal health campaigns. The clinics that specialize only in pediatrics, where we’ve also been implementing the HPV intervention, are new to academic detailing but have been extremely receptive to this campaign. Anna: I recently saw your team’s work on your HPV project published in the Delaware Journal of Public Health. Can you briefly describe the results? Lisa: Sometimes, it takes a small change to make a huge impact, and that is absolutely what we found with our project. For our engaged practices, we saw in a one-year span that the initial dose of HPV increased 8.1%. It’s important to note that practices usually picked more than one intervention. For example, some chose academic detailing along with workflow modifications, like nurse reminders or scheduling the patient for their next vaccine before leaving the office. Anna: Those are significant results, especially in such a short timeframe! What’s one thing you’d want our detailing community to take away from this project? Lisa: We found that practices were most successful when they chose an intervention, stuck with it, and set attainable goals. Some practices were at a 50% HPV vaccination rate and wanted to be at 80%. In those situations, we sat down with them and asked them to think about something more attainable, like a 5% increase in 6 months. Practices that committed to smaller increases not only met their goal, but slightly outperformed it. We’re excited to continue our work around this topic! Anna: Setting attainable goals and following through is so important for all projects. We’d love to hear more about your future work and how this campaign continues to grow and succeed! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Lisa is a Practice Transformation and Quality Improvement Project Leader with nearly 20 years of experience in the healthcare and managed care industries, with the leadership and skills to serve as a Program Manager. She is an expert in population health management, data analysis and audits, and customer engagement across payers and customer types, including Medicaid and Medicare and underserved and rural populations. She has applied leadership and project management skills to improving population health, quality results, and data integrity in Accountable Care Organizations (ACOs), Patient Center Medical Home (PCMH), and new business development and reporting. She's well versed in data analysis including Healthcare Effectiveness Data and Information Set (HEDIS) and National Quality Forum (NQF) measures, population health management tools, as well as internal Quality Insights reporting tools and state run database reporting. In the past 5 years, she has successfully managed multiple projects and people to meet deliverables and deliver value to customers.  Guest Blogger: Joseph Leishman Academic Detailer/Masters in Public Health Candidate Center for Clinical Management Research, Ann Arbor VA The University of Michigan School of Public Health NaRCAD Training Alumnus Tags: Cancer, Detailing Visits, Materials Development, Training  NaRCAD: How did you get into AD? What were you doing before? Joe: I’m a graduate student at The University of Michigan School of Public Health studying epidemiology. As a student I started working at the Ann Arbor VA Center for Clinical Management Research on a lung cancer-screening project. Our project involves 8 different VA sites across the country. As we shifted into an implementation phase, academic detailing was selected as an implementation method. I transitioned to an academic detailer role because of my background in epidemiology, my understanding of lung cancer screening (LCS), and my ability to communicate these principles. I attended the NaRCAD academic detailing techniques training and things took off from there! 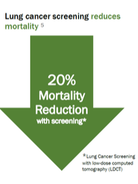 NaRCAD: Why is AD for lung cancer screening so important? Joe: Lung cancer screening can be more complex and complicated compared to other preventative services, and most primary care physicians have very limited time to discuss lung cancer screening with patients. There are a number of potential downsides to screening – false positives, overdiagnosis, invasive procedures, and complications from invasive procedures. The benefits of the screening outweigh the challenges, and we have developed a tool for doctors to quickly evaluate a patient’s lung cancer risk, facilitate shared decision making, and make personalized screening recommendations. NaRCAD: Tell us about the lung cancer screening detailing aid and related tools that you made with NaRCAD’s support. How was the process of developing the detailing aid? Joe: Our detailing aid contains background information on lung cancer screening and some of the key evidence behind our tool. It also outlines some of the reasons and benefits behind using this risk-based approach. We tried to keep the detailing aid simple enough that doctors could quickly understand the concepts with little or no additional explanation. This was our group’s first attempt at making something like this. We worked with NaRCAD during the creation of the detailing aid to improve the clinical content, layout, and language. There was a lot of trial and error to create the detailing aid. We ended up going through 10 versions before it was finalized.  NaRCAD: How did you decide what information was most important to put on your detailing aid? Joe: Initially, we started out with too much information. It was too complicated and wordy to effectively communicate our message. We tested it out with our team to see if our message was clear. It was obvious when sections of detailing aid didn’t work well. We really had to focus on narrowing down the main evidence and messages we wished to convey. We used the primary lung cancer screening evidence from the US Preventative Task Force and the National Lung Screening Trial. Our tool goes a step beyond screening eligibility to look at individual risk, life expectancy, and patient preferences, which help providers get past some of the difficulties and complexities of lung cancer screening.  NaRCAD: How does your website complement the detailing aid when you are 1:1 detailing? Joe: A link to the tool is embedded in the Computerized Patient Record System (CPRS), the EMR system that the VA uses. However, it can be also accessed outside the VA with a URL. What I typically do is I have PCPs pull up the website in their workspace after going through the detailing aid. I have providers role play with a sample patient, and I demonstrate how the tool could be used for that specific patient. Using the actual web tool in a detailing meeting really helps to reinforce our message. We feel like it increases the likelihood that it’ll be adopted in an actual clinical practice. NaRCAD: How have clinicians been responding to your campaign? Joe: So far there has been a decent response from the doctors we have worked with. Some of the doctors in the VA have met with detailers before which makes the initial contact easy. However, the most majority of the doctors I have met were receptive to my visits. We’ve been tracking the use of our tool before and after academic detailing at a site level. We don’t have exact numbers, but there has been an increase between before and after AD. We’d be happy to share more complete data in a future blog post.  NaRCAD: That'd be terrific, we'd love to share that when it's ready! What other reflections do you have from this process that you'd like to share with our community? Joe: Academic detailing is a new approach for our group. It has been a real learning experience for discovering what does and doesn’t work and how to best address provider needs. For me, going through this process has been a lot of fun. I love talking with doctors about their struggles and being able to offer a tool that can help them better handle lung cancer screening with their patients.  Tags: Cancer, Cardiovascular Health, Diabetes, Training We travelled to Boise, Idaho on March 10th, 2016, joining forces with the Idaho Department of Health and Welfare (IDHW) on a new academic detailing initiative. On March 11th, we facilitated a 1-day workshop for 14 active academic detailers working on two public health priorities: promoting diabetes screening and management tools as part of their Diabetes, Heart Disease, & Stroke Program, and increasing colorectal cancer screening across the state as part of IDHW’s Comprehensive Cancer Control program.
 The session emphasized the importance of determining strong, specific, and actionable key messages, and helped the academic detailers practice delivering those messages clearly. Exercises in small groups focused on preparing for the inevitable obstacles that arise during a visit, anticipating different types of pushback or questions, and developing strategies for effective responses. Using roleplay, workshop participants practiced conveying their program’s goals in a dynamic, clear, and interactive way while continuously assessing the clinician’s specific needs.
We’re looking forward to reporting back on the successes and growth of the Idaho Department of Health and Welfare’s academic detailing programming to improve health outcomes by increasing colorectal cancer screening and effective diabetes diagnosis, prevention, and management throughout the state. Interested in learning more about our trainings or workshops? Learn more here, or contact us and tell us about your program's needs.
 Trainee Update Series: Where Are They Now? Bevin K. Shagoury, Communications & Education Director Tags: Cancer, Detailing Visits, Practice Facilitation, Training Hi, Emily! We’re happy to reconnect with a NaRCAD trainee, and to feature your current work on this month’s blog. Can you tell us a little about yourself and how you ended up working at the National Colorectal Cancer Roundtable? I’ve worked in public health for 12 years, and in seven of those years I’ve focused on cancer screening and prevention. I got to know NaRCAD while working at the Washington State Department of Health, where I designed their approach and curriculum to coach primary care clinics and health systems on quality improvement strategies to increase colorectal cancer screening. Then last summer I joined the American Cancer Society as the National Colorectal Cancer Roundtable’s new associate director. In this role much of my work is still focused on developing educational resources for providers, but I’m also involved in efforts to increase colorectal cancer screening through other channels, such as public education and policy. I learned so much about effective methods for conducting clinical education from the NaRCAD Academic Detailing training that I participated in back in October 2012. I’m grateful to have the opportunity to reconnect with NaRCAD, and thank you for the opportunity to share an update on my work! Tell us a little bit about background and goals of the Roundtable. The Roundtable, established by the American Cancer Society (ACS) and the Centers for Disease Control and Prevention (CDC) in 1997, is a national coalition dedicated to reducing the incidence of and mortality from colorectal cancer in the U.S., through coordinated leadership, strategic planning, and advocacy. Today, the Roundtable is a collaborative partnership with more than 100 member organizations across the nation. Through the efforts of several task groups, the Roundtable advances initiatives that focus on provider education, public education, health policy, quality and disparities issues. Thanks in part to the work of many of our members, colorectal cancer incidence and mortality rates have dropped by over 30% in the U.S. among adults 50 and older in the last fifteen years, with a substantial fraction of these declines due to screening. Yet, despite the good news, colorectal cancer remains the second-leading cause of cancer death in the U.S. when men and women are combined.  The Roundtable is focusing on a great initiative called “80% by 2018.” What’s the story behind this movement? To accelerate efforts to increase colorectal cancer screening, the Roundtable launched the 80% by 2018 initiative in March of 2014. 80% by 2018 is a movement in which hundreds of organizations have committed to substantially reducing colorectal cancer as a major public health problem and are working toward the shared goal of reaching 80% of adults aged 50 and older screened for colorectal cancer by 2018. To date over 650 organizations – including medical professional societies, academic centers, survivor groups, government agencies, cancer coalitions, cancer centers, payers and many others – have signed a pledge to make this goal a priority. If we can achieve 80% by 2018, 277,000 cases and 203,000 colorectal cancer deaths would be prevented by 2030. You can learn more about 80% by 2018 and pledge your organization’s support on our 80% by 2018 webpage.  A trainee role-plays at a NaRCAD 2-day techniques session. A trainee role-plays at a NaRCAD 2-day techniques session. You attended a NaRCAD Academic Detailing Training a few years back to practice skills in clinical outreach education. Can you tell us a little bit about the highlights of your experience? Academic detailing and practice facilitation are relatively new fields, so when I first accepted a job that included these skills I felt a little in over my head! I was up for the challenge, though, since I saw provider education and training as a way to move further upstream in making substantive and sustainable changes that would positively affect public health. It can take a while for new clinical findings to get implemented in primary care, so I saw that academic detailers and practice facilitators serve a key role in getting these findings into clinical practice. My two-day Academic Detailing Training with NaRCAD taught me practical skills to work in this role, and gave me the confidence to know I could be effective without a clinical background. The highlight was the role-playing and one-on-one feedback from experienced academic detailers. Their personal feedback was not something I could have found in a book or online training. What tools from the training do you think are most relevant to active detailers in the field? Some of the most valuable tools I took from the training were the interpersonal skills needed to be effective as an academic detailer. The tips on how to solicit buy in after sharing a practice change was incredibly useful, such as asking: “does this sound like something you’d be willing to try in your practice?” It was also really helpful to learn how to approach sharing a clinical update that could potentially make a provider feel as though they had been delivering inappropriate care. The training taught me how to navigate these discussions by saying that while something might be common practice it’s no longer supported by the latest clinical evidence. In my experience, providers were very receptive to learning new clinical updates when it was shared in such a way that they did not feel they were being reprimanded for not knowing already knowing the latest evidence. Thanks for chatting with us. We’re happy to help get the word out about “80% by 2018” and looking forward to hearing the results of the initiative. Thank you for the opportunity! I enjoyed reconnecting with you and reflecting on how my training with NaRCAD has enriched my work in clinical education. I’d like to encourage any readers that are interested in 80% by 2018 and efforts to increase colorectal cancer screening to learn about the campaign. And there are lots of great tools and resources in the provider education section of our website that might be of particular interest to academic detailers.  Emily Butler Bell is the Associate Director of the National Colorectal Cancer Roundtable. In this role she manages a number of projects that support the 80% by 2018 initiative, a movement in which hundreds of organizations are working toward the shared goal of reaching 80% of adults aged 50 and older screened for colorectal cancer by 2018. Prior to joining the Roundtable, Emily served as the Cancer Screening Quality Improvement Consultant for the Washington State Department of Health, where she designed their approach and curriculum to coach primary care clinics and health systems on quality improvement strategies to increase colorectal cancer screening. Prior to that, Emily worked with the American Cancer Society in Austin, TX as a Cancer Information Specialist and later as a Health Insurance Specialist, where she gained insight into the access and affordability issues surrounding colorectal cancer screening. She holds a Master’s in Public Health from Boston University and a B.A. in Psychology from the University of California, Santa Cruz. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|