|
Curated By: Aanchal Gupta, Program Coordinator, NaRCAD Tags: ADvice, Program Management, Training Academic detailing program managers oversee and coordinate all aspects of an AD program to ensure its success, impact, and strengthen the detailing team. They have a crucial role in achieving team goals. In this edition of AD-vice, we’ll look into how program management in AD contributes to team and program success.  Team Building and Support:
 Recruitment and Training:
 Interprofessional Collaboration:
Effective program management plays a crucial role in the success and support of academic detailing programs. We hope the insights shared in this edition of AD-vice will help in navigating and implementing strategies of team building, recruitment, training, and more. As always, our NaRCAD team is here to support you and your detailing programs! Best, The NaRCAD Team Have thoughts on our DETAILS Blog posts?
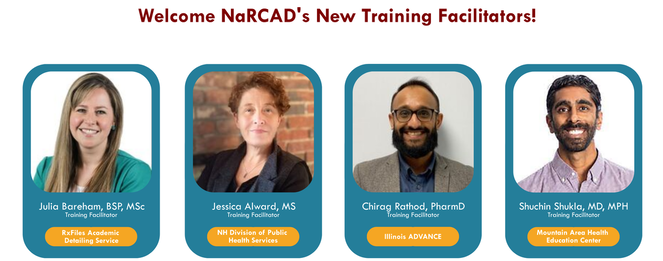
You can head on over to our Discussion Forum to continue the conversation!  Tags: Training, Detailing Visits We are proud to announce that our team at NaRCAD has trained over 1000 people in the techniques of academic detailing. We’ve conducted 60 trainings for detailers working on an amazing range of clinical topics since our first techniques training in 2011. Thank you for growing with us as we’ve expanded from two trainings a year to offering eight trainings in 2022. In honor of reaching this milestone, we’ve compiled testimonials from some of our trainees over the past 11 years. "Just the right amount of didactic, practice, then putting it all together—I'm ready to develop materials & try it.” “I now have the confidence to carry out a successful educational visit!" “The small groups were perfect for interacting, getting to know each other's backgrounds, and made conversations and learning enjoyable." “I came away with refined communication skills and improved clinical knowledge, thanks to the outstanding facilitators.” “This was fantastic! I learned so much and [am] definitely more comfortable with detailing. It was friendly and open to mistakes, and I really appreciated it.” “I walked away with great feedback, knowing my strengths and where I can improve.” “It gave me great insights on the skills I need to be a successful detailer!” “This training provides the opportunity to learn about AD in an interactive way that allows for growth though practice.” We’d like to thank our trainees for committing to improving patient outcomes through clinician education. We’d also like to thank all our past and current NaRCAD facilitators for providing our trainees with the skills needed to be successful and confident detailers. We’re excited to share that we’ve had the pleasure of adding four more training facilitators to our team this year. Welcome to the team, Chirag, Jess, Julia, and Shuchin! We look forward to continuing to work with all of you. Read more testimonials on our testimonial page or share your training experiences with us below!
-The NaRCAD Team  This series features tried-and-true practices from our AD experts. This week’s guest blogger is Zack Dumont, BSP, ACPR, MSPharm a NaRCAD Facilitator and Academic Detailer at RxFiles Academic Detailing Service. Curated by Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Detailing Visits, Stigma, Training  Model the compassion you expect from others. In recent years, the academic detailing community has been trying to recognize the harmful role of stigma in many clinical settings and to include stigma reduction in our detailing messages. In applying this framework, we encourage an empathetic view of people who experience stigma. They don’t choose to have addictions, exhibit certain behaviors, or to be ‘villainous’. We can all agree they don’t deserve harsh judgment and criticism. I invite you to bring forth your most charitable mindset for a moment and apply that same framework when you encounter stigma during a detailing visit. Imagine that the clinicians or people you detail hold stigma not because they want to stigmatize others, but for some more relatable reasons: they’re impressionable, they’re naïve, they’re vulnerable. In the same way that a clinician wouldn’t expect someone with a substance use disorder to suddenly recover if harshly confronted, we can’t expect the person who stigmatizes to respond to similar tactics. Be patient, be persistent (after all, you care and want them to be their best selves), and be persuasive with those that you’re detailing. You have a lot of natural talent, training, and experience to efficiently help people make informed decisions through detailing visits. Don’t limit it to therapeutic decision-making; extend it to the mental and emotional aspects of care, as well.  Balance and refine your self-reflections. Alone or with a colleague, find a quick and easy way to debrief after each visit – save the more intense feedback for quarterly or annual reviews. Maybe it’s asking two simple questions like, “What went well?” and “What could have gone better?” and taking a moment to reflect on each. And, just like AD visits which are 90% prep and 10% execution, the more the better when it comes to ‘prepping’ your self-reflection questions. So, “What went well?” could be more specific to one of your strengths:
Your “What could have gone better?” question could focus on an area of improvement unique to you:
This isn’t easy, but it’s low risk with the potential for big reward… so I encourage you to jump in! Want more tips? Stay tuned for the next installment in our Words of AD Wisdom series, and reach out to the NaRCAD team, subscribe to our network, or check out our discussion forum to hear more tips and ways to train your brain!  Biography. Zack is a clinical pharmacist with the RxFiles Academic Detailing Service in Regina, Saskatchewan, Canada and an expert facilitator for NaRCAD's training courses. He has been involved with the RxFiles since 2008, with experience in both academic detailing and content development of RxFiles’ evidence-based drug therapy comparison tools. Zack also serves as the Clinical Manager for the Saskatchewan Health Authority Pharmacy Department. His practice has largely been hospital-based, with more specialized experience in anticoagulation and heart failure. His professional interests include evidence-based medicine, information technology, and leadership. Zack graduated as a Pharmacist from the University of Saskatchewan in 2008. Following graduation, he completed a hospital pharmacy residency with the Regina Qu’Appelle Health Region. He also completed a Master’s degree in Pharmacy, with a focus on leadership, from the University of Cincinnati. By Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD An interview with Sandeep (Sonny) Singh Bains, PharmD, BCPS, Clinical Educator, Alosa Health. Alosa Health is a national leader in developing and implementing academic detailing programs to improve prescribing. Tags: Detailing Visits, Evidence-Based Medicine, Primary Care, Training  Anna: Hi, Sonny! It’s wonderful to connect with you today and hear about your work as a clinical educator at Alosa Health. What has your clinical pharmacist journey looked like to date? Sonny: I’ve been working for over a decade in hospitals and primary care. I completed my residency in hospital pharmacy, and as I continued to do administrative and clinical work in hospitals, my interests shifted more towards primary care and population health. I’m originally from California where it’s common to have pharmacy involved in primary care. When I moved to Pennsylvania, a lot of clinicians didn’t understand why a pharmacist would be in a primary care setting and were skeptical of me and my role within the clinic. Fast-forward 10 years, and almost every health system in Philadelphia has a pharmacist on their team within their primary care network. I’d like to think that I can take a little bit of credit for paving the way for pharmacists on primary care teams throughout our state! Anna: That’s definitely something to be proud of. How did you end up being a detailer?  Sonny: I’d been noticing a lot of overlap in the work being done in our primary care clinics by different members of the team. I ended up creating protocols to automate certain things for different chronic conditions and people would say, “Wow, this is brilliant.” It really wasn’t brilliant; I was using the same set of guidelines in the literature I was reading and was communicating that to clinicians to make workflows easier. I didn’t know about the strategy of academic detailing at the time, but I knew I needed to educate clinicians. I was fortunate enough to be connected with Alosa Health and I now work for them as a full-time consultant. I work as a detailer and also help hire, interview, train, coach, and mentor new detailers on the team. Anna: You were meant to be a detailer before you even knew what it was! Alosa has been working on diverse clinical topics over the years including, antiplatelets, atrial fibrillation, immunizations for elderly, serious illness conversations, chronic obstructive pulmonary disease (COPD), heart failure, dementia, atherosclerotic cardiovascular disease (ASCVD) prevention, diabetes, acute pain, chronic pain, and opioid use disorder. What have been some of the campaigns where you’ve felt you’ve made an impact? Sonny: It’s a lot of fun to be working on so many different campaigns. Many of the topics fit right into my wheelhouse with my hospital and primary care background. Diabetes has been my favorite topic. I’ve been able to make a large impact for patients and care providers. We’re able to improve lives of patients (prevention of stroke/heart attacks) and improve outcomes for providers and health systems (financial incentives, quality ratings, etc.). I’m also proud to be part of the pain modules. The opioid epidemic has impacted all of us in America and I’m glad to be able to do my part in helping to bring resources and evidence-based treatment to local providers in our community.  Anna: It sure sounds like you’ve been able to make an impact! How has your work with Alosa evolved over the years? Sonny: Alosa Health has been expanding and we have several new partnerships and collaborations throughout the United States. We started detailing only in the state of Pennsylvania and we’ve now expanded to numerous states. It’s been exciting to be part of the leadership team to help coach detailers, as well as create creative partnerships with local health systems to improve outcomes for patients. Anna: What challenges have come up as your program has continued to expand? Sonny: The biggest barrier we’ve experienced, like many detailing programs, has been access to clinicians and the ability to set up visits. I’ve had relationships with clinicians and clinic staff in the past where I could have walked into any office at any given time, but I’ve lost a lot of those relationships with COVID and staff turnover. I’ve been working hard to reestablish relationships in the field and teach new detailers how important strong relationships are to our work as detailers.  Anna: What approaches have you taken to reestablish relationships, as well as to gain access to new clinics? Sonny: I like to partner with colleagues that I’ve worked with previously. I recently connected with a former colleague who’s a VP at a large healthcare organization and we quickly realized we could help each other improve patient outcomes and reduce cost. From this connection, I was able to get buy-in at the administrative level and accessed hundreds of prescribers. They even gave their clinicians a monetary incentive to meet with our detailers. We’ve also benefited from connecting with administrators of health systems. We approach them like business partners; it takes a special skill to communicate and work with an administrator. It’s important to have team members who understand how to communicate with leadership effectively to get that buy-in. Anna: It might take more time to get buy-in from administrators, but it opens so many doors once it’s done successfully. As we wrap up, can you tell us some tips to help our readers be effective detailers and communicators? Sonny:
Anna: It’s so important to put the work in to build solid relationships with clinicians in order to be an effective detailer. Thanks for joining us on the DETAILS blog, Sonny - our AD community will gain a lot from the insights you’ve shared today! Learn more about Alosa’s work: alosahealth.org/clinical-modules Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Sandeep is a clinical pharmacist with extensive clinical leadership experience in both acute care and ambulatory healthcare settings. He completed post-graduate training at Einstein Medical Center in Philadelphia and has since worked in clinical pharmacy leadership with large healthcare systems in the greater Philadelphia area. He is also the principal consultant at Bains Rx, LLC, a healthcare consulting firm dedicated to improving outcomes while reducing costs. Supporting Clinicians in Utah: Working Together to Utilize Safe Opioid Prescribing Guidelines3/25/2022
An interview with Parveen Ghani, MBBS, MPH, MS, Health Program Specialist III, Division of Professional Licensing, State of Utah. by Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Opioid Safety, Evidence Based, Training  Anna: Hi Parveen! You’re one of our training alumni who’s built a strong program over the past few years. We’re thrilled to be able to catch up with you! Can you tell us about yourself? Parveen: I’m trained as a physician and have always wanted to work in public health. It was important to me to be able to make a difference in people’s lives. I currently work in the Division of Professional Licensing at the Department of Commerce in Utah. I've been working as an academic detailer since my NaRCAD training a few years ago. Anna: It sounds like the rest is history! Are there other detailers on your team who are helping you meet your program goals? Parveen: I’m a full-time detailer for our AD program along with my colleague, Marie Frankos. We work with many of the same prescribers over multiple detailing visits and build strong connections with them.  Anna: Can you talk to us about your detailing work in overdose prevention? Parveen: Opioid overdose in the State of Utah is exceptionally high. We’re currently working with prescribers on the safe prescribing of opioids. Our state’s prescription drug monitoring program is called the Controlled Substance Database Program (CSD). The CSD includes both a Patient Dashboard and Prescriber Dashboard. The Patient Dashboard is an electronic clinical decision-making tool that grants prescribers access to information regarding controlled substance prescriptions for individual patients. It contains records of a patient’s poisoning or overdose and any violations associated with a controlled substance. The Prescriber Dashboard, on the other hand, tracks each clinician's prescribing patterns and CSD utilization behavior. Anna: We’ve seen a lot of success with detailing programs who work with clinicians to navigate their state’s prescription drug monitoring program, like your CSD. Does your state require prescribers to look at this database?  Parveen: Yes. According to the Utah Controlled Substances Act, (a) A prescriber shall check the database for information about a patient before the first time the prescriber gives a prescription to a patient for a Schedule II opioid or a Schedule III opioid. (b) If a prescriber is repeatedly prescribing a Schedule II opioid or Schedule III opioid to a patient, the prescriber shall periodically review information about the patient in: (i) the database; or (ii) other similar records of controlled substances the patient has filled. Anna: It’s so important to support prescribers in using a database like this, especially when there are mandates in place. What is the overall goal of your AD program? Parveen: The goal of our AD program is to provide recommendations to prescribers regarding best practices in the utilization of the CSD per the Controlled Substance Database Act. This includes identifying individual prescriber’s prescribing and dispensing patterns of controlled substances, identifying prescribers who are prescribing in an unprofessional or unlawful manner, and identifying polypharmacy, doctor shopping, poisoning, or overdoses. Anna: It sounds like your AD program is working hard to support clinicians in CSD utilization. What kind of resources have you developed for clinicians that work towards your program’s overall goal, and how do you make these materials accessible? 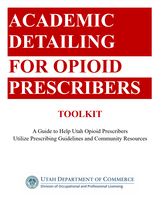 Parveen: We’ve created a toolkit that acts as a guide to help clinicians utilize the database and different resources within the community. During our in-person visits, we provide hard copies of materials that include screenshots of how to create a CSD account, reset CSD account passwords, and navigate the dashboards within the CSD. During our virtual AD sessions, we send these materials electronically. Additionally, we provide our contact information for further technical assistance, including our personal phone number, work phone number, and email address. We've made our toolkit available on our website along with prescriber FAQs. We’re continuing to update our website with helpful materials for clinicians. Anna: Making resources like this so accessible is key. Can you share some reflections on visits where you felt like you made a difference or were able to offer technical assistance? Parveen: I love helping prescribers, even if it is something as simple as walking them through the log-in process or resetting a password. I’ve had clinicians bring their entire medical team in for a detailing visit so that I can show everyone in the office how to use the database. One prescriber even told me after a visit that they would be sharing my name with a colleague and that I should expect a call to schedule a detailing visit. It’s lovely to get these types of referrals from the clinicians. Anna: Prescribers feeling thankful and impressed with your 1:1 support enough to refer you to their colleagues is a huge success! Let’s wrap up with one more question - what’s one tip you’d give to another academic detailer? Parveen: Find ways to collaborate. We can’t do it alone! Start working together with other programs and share information, especially community resources. We can really make a difference if we work together. Anna: I couldn’t agree more. Making community connections and sharing information allows for great success in accomplishing goals for both small and large initiatives. Our AD community will be able to glean a lot from your program’s successes, and we look forward to sharing more of your team’s expertise in the future. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Parveen Ghani has over eight years of work experience in public health. She obtained her Master in Public Health degree (MPH) from Walden University (Minneapolis, Minnesota). Following this, she worked for four years with the Office of Minority Health for the Nebraska Department of Health and Human Service. Parveen relocated to Idaho Falls in 2015 with her husband and began to pursue her career in bioinformatics. She obtained her master’s degree in Biomedical Informatics from the University of Utah in May 2018. Shortly after graduation, she started working as an Academic Detailing Specialist with the Division of Professional Licensing (DOPL), Salt Lake City, Utah. Before moving to the United States, Parveen earned her medical degree (MBBS) from Dhaka Medical College, Bangladesh. While not licensed in the United States, Parveen has worked as a physician in Bangladesh, Ireland, and Australia. Parveen enjoys working with the prescribers on the safe prescribing of opioids. Parveen loves to exercise, walk, read, play the piano, and play with her pet kitty in her leisure time. An interview with Karen Curd, Program Manager, Midwest AIDS Training and Education Center in Indiana (MATEC-IN). by Anna Morgan, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: HIV/AIDS, PrEP, Training 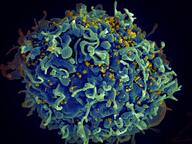 Anna: Thank you so much for joining us today, Karen. We're excited to learn more about you and your program. Can you start off by telling us a little bit about your professional background and how you ended up in your current role? Karen: Thanks for having me! I stumbled into public health by accident. I majored in kinesiology in college and interned with a health promotions department at a local hospital after graduation. That’s what really got me interested in health education. I ended up meeting somebody who worked at the local county health department in STI prevention. She encouraged me to apply for an open position as a disease intervention specialist; that ended up being both a challenging and rewarding job. It taught me so much about public health and I was hooked! I moved on to work as the STI screening and surveillance coordinator, which allowed me to interact more with healthcare providers. Nearly a decade went by of working in STI prevention before I joined the Midwest AIDS Training and Education Center-Indiana (MATEC-IN) team as the training coordinator. I now work as a program manager at MATEC-IN.  Anna: We’re so happy you ended up in public health! Can you share more about your current role as program manager and about MATEC-IN as a whole? Karen: MATEC is part of the national network of AIDS Education and Training Centers. MATEC houses 10 states across the region, and I work at a local partner site in Indiana. We provide training and technical assistance to healthcare providers throughout the state, primarily focusing on HIV and increasing their comfort and capacity to provide HIV care. For those outside of the field, I usually explain my role as part health educator, part event planner, and part networking and resource specialist. A lot of what we do is connect healthcare providers to all the amazing organizations and individuals who provide support and care for people living with HIV. We spend a lot of time talking to people, finding out what information or resources they need, and connecting them. We also develop new tools and trainings as needed. Anna: Your team is doing such incredible work supporting and connecting healthcare providers. How do you see the strategy of academic detailing fitting into this work? Karen: The Ending the HIV Epidemic (EHE) initiative aims to reduce new HIV infections in the United States by at least 90% by the year 2030 through activities focusing on four pillars. The four pillars are: diagnose, treat, prevent, and respond. At MATEC-IN, we hope to focus our EHE efforts on the diagnose and prevent pillars by encouraging and engaging primary care providers throughout our state. We want to be recruiting these community providers to increase routine HIV testing, and to become comfortable recommending and prescribing pre-exposure prophylaxis, or PrEP, to their patients. We hope to use academic detailing to educate these busy providers. We see AD as another great tool in our toolbox.  Anna: You recently partnered with us for a customized academic detailing virtual training and successfully recruited 18 trainees. Can you tell us a little about what that process was like and what tools you used to recruit those trainees? Karen: We planned our training as a regional MATEC opportunity and opened recruitment to our entire 10-state region to any organization funded by EHE. We first hosted an introduction to academic detailing session for our other MATEC sites which gave them an opportunity to learn about what academic detailing was and begin thinking about who they might want to recruit from their state for the 3-day NaRCAD training. Because the training is extremely interactive and is limited as far as size, we wanted to make sure that we were recruiting the right individuals. Our director, Malinda Boehler, developed a recruiting tool that we shared with the different site directors in our region. We then asked each site to recruit two to three individuals from their state and have the individuals complete a short questionnaire that we developed prior to registering for the training. Anna: You did a thorough job recruiting detailers and it shows; we had an amazing training with you all because you selected such engaged and passionate trainees. Do you have any tips you would share with other folks who are looking to recruit a large number of trainees for a customized training? Karen: Set expectations. I would stress the importance of clearly defining training expectations as far as what attendees should and should not expect to learn over the 3 days. We wanted to make sure that it was clear to trainees that the NaRCAD training would not cover the day-to-day of how an academic detailing program would be rolled out at their specific institution, but rather the communication techniques used during an academic detailing visit. We had a lot of conversations with trainees before they came to the training and I think that helped to set those expectations. Anna: That’s a great tip! You were in a unique position where you were able to observe the training. What were some of your key takeaways?  Karen: I’m so thankful to have had the opportunity to observe. Even though I technically wasn’t a participant who engaged in role play, I found that learning from other trainees was the most valuable. The training facilitators were also excellent. They provided a very safe and structured environment for learning and role playing. Not only did the participants have the opportunity to practice and role play, but they were also encouraged to offer feedback to peers. We had a range of folks in our small group; some had been working in the field for years and some were brand new to the field. It was amazing to see them learn from each other. One participant shared with me that the training provided them with persuasive communication skills that will be useful in situations outside of a detailing visit, like an interaction with a client, a patient, or partner organization. Anna: The skills you learn at an academic detailing training can be applied to so many situations, including those with family and friends! Is there any additional advice you would share with others who are looking to become a detailer or support a detailing program? Karen: Be flexible. When our team initially began looking for information about academic detailing, we were looking for existing materials that we could adapt for our state and do the detailing ourselves. After meeting with your team at NaRCAD and learning more about the process, we realized that we needed to redirect our efforts to recruiting trainees from EHE funded sites within our region to broaden our reach. I would also recommend starting recruitment efforts early to allow plenty of time to find the right recruits in order to build a successful training cohort! Anna: That's great advice, Karen. What does the future look like for this group of trainees and how do you plan to continue to support them across state lines? Karen: Our region has hired an EHE coordinator who plans to engage frequently with the training cohort. We want to bring these folks together through monthly check-ins because we know that detailing can be isolating. Not all the trainees are doing the same exact work, but we think getting them connected with folks who are doing detailing in other states on the same topic will be beneficial. We’ve also been spreading the word about academic detailing at our health department in Indiana since our state doesn’t have a structured AD program like some other states do. We hope to get more folks trained from our state in the future and use academic detailing across diverse topic areas. Anna: How exciting! We’re thrilled to continue to partner with you as academic detailing expands throughout your state and region. We look forward to future trainings and hearing about your team’s successes! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Karen Curd is the Program Manager at the Midwest AIDS Training and Education Center (MATEC) in Indiana. She has worked in public health for nearly two decades, starting her career as a Disease Intervention Specialist for the Marion County Public Health Department (MCPHD) in Indianapolis, Indiana. She also served as Screening and Surveillance Coordinator for MCPHD before transitioning to the role of HIV/MAI Training Coordinator at MATEC Indiana in 2011. In her current role of Program Manager, Karen oversees several MATEC initiatives focused on providing training and technical assistance to healthcare providers throughout Indiana. Karen received her BS in Kinesiology from Indiana University in Bloomington, Indiana. An interview with Carla Mena, Capacity Building Manager at Hands United of the Latino Commission on AIDS. by Aanchal Gupta, NaRCAD Program Coordinator Tags: HIV/AIDS, Training, Program Management  Aanchal: Hi Carla, thank you so much for joining us today! We’re excited to delve into Capacity Building Assistance (CBA), as well as feature Hands United of the Latino Commission on AIDS on our blog. How did you get started in this line of work, and could you describe your current role as a capacity building manager? Carla: I worked at a Duke University hospital in North Carolina for 7 years as a bilingual research coordinator in both local and global studies. I have research experience in hepatitis C, HIV, immigration, LGBTQ+, childhood obesity prevention, neonatal vaccinations, reproductive health, and the intersection of these areas. I also did some leadership development work, as well as community organizing. I had the opportunity to connect with teams and individuals on how to work with underserved populations, and taught them about social determinants of health, cultural humility, and health equity. At Hands United, I began as a capacity building specialist, and have now transitioned to a capacity building manager. I make sure that we’re thinking within our funding guidelines while also highlighting the intersections of folks living with HIV or who may be at risk of acquiring or transmitting HIV. As a manager, there's the administrative side of supervision, following up on tasks, and so on. The other aspect of it is to continue to provide technical assistance (TA) to our jurisdictions. For example, if someone is interested in implementing an HIV self-testing program in a non-clinical setting, I can assist with that. I enjoy the fact that, although I'm not a specialist anymore, I still provide TA with the team. Both of our directors also provide TA, which I think is unique.  Aanchal: Wow, you have such an extensive background in public health and sounds like it has informed your current work! Tell us more about the Hands United program as well as the importance of capacity building assistance. Carla: The Hands United of the Latino Commission on AIDS is a capacity building technical assistance program (CBA). The CHANGE (customized, holistic, analytical, network-building, grassroots, evaluatory) model is an approach developed by the Latino Commission on AIDS. Hands United is one of the two programs available. It combines community-based organizations, health departments, or any other social service organizations to optimally plan, integrate, implement, and sustain prevention programming and services. CBA improves the performance of the HIV prevention workforce by building individual-level competencies and technical expertise while also strengthening organizational capacities. We serve 19 jurisdictions in the southern region of the United States including, Arkansas, Alabama, Delaware, D.C., Florida, Georgia, Kentucky, Maryland, Louisiana, Mississippi, North Carolina, South Carolina, Oklahoma, Tennessee, Texas, Virginia, and West Virginia. An organization will contact us about various topics related to HIV prevention such as recruitment for HIV testing, referrals for HIV medical care, referrals for PrEP, nPrEP, STIs, hepatitis C, or TB screening. Our role is to help them figure out what resources they need. Then we can support them with webinars or resources such as literature reviews, marketing samples, and successful stories.  Aanchal: Thanks for providing some context on the program and intervention. It’s always great to know that there are resources like this out there for organizations to utilize. Could you describe how CBA relates to academic detailing? Carla: Detailing is very fundamental for the work that we're doing because it teaches effective social and personable skills that organizations can take out in the field. Sometimes health departments reach out to us and say that they are not sure how to recruit for providers to refer or prescribe PrEP in primary care settings. These are times when we discuss academic detailing and how it can be useful for them. Although we’re not detailing, we’re able to provide information in a way that makes sense to those who need it. We ask them questions to better understand their program and help programs figure out exactly what they need. We ask questions like, “What is part of your package?” “What are the questions you're asking clinicians?” “What is your elevator pitch?” “Is there capacity and effort from the staff?” We might even say, “You need detailing, but you don’t have enough staff to be able to detail all the primary care providers in your county.” When this happens, we provide assistance on developing a recruitment plan that’s feasible for the requestor.  Aanchal: Those are all important questions for programs to consider as they brainstorm what it is that they need. Is there something that your program was able to accomplish during this past year that you’re proud of? Carla: We were able to work with your team at NaRCAD and host a training this past July. This was a highlight for us because we were able to have a good representation and engagement from the jurisdictions. A community was created through the participation of the trainees. We gained a lot of knowledge that we needed in order to provide TA or CBA services to our programs. Aanchal: That’s so nice to hear! Speaking of the training, I’d love to hear about your experience, particularly as you’re someone who was not planning to be a detailer. Carla: For me, it was a great training because all the training facilitators were so welcoming of feedback and even role played to include our specific experiences. They took time to understand our roles and built a sense of community. Additionally, it was very hands-on, and I enjoyed having the opportunity to role play a detailing visit. Walking in the detailer’s shoes helped me understand exactly what could be happening to them during a visit or where they may be challenged. Fusing my own lens with the lens of the detailer was very helpful.  Aanchal: I agree -- the trainings provide a practical space for trainees to share their unique experiences while practicing the communications techniques necessary to carry out a 1:1 detailing visit. Is there any advice you would give to someone who may be hesitant about attending an academic detailing training if they ‘re planning to be a program manager rather than a detailer? Carla: I would say, go for it! Although we may not be detailers, being able to walk through what a detailer does has made me a better CBA specialist and manager because I understand the processes through the eyes of the detailer. Watching webinars or reading resources on academic detailing was helpful and effective, but attending a training gave the opportunity to put it all into practice. Aanchal: That is great advice! Thank you so much, Carla, for speaking with us and it was a pleasure having you at our training. We look forward to working together in the future. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography: Carla is the Capacity Building Assistance Manager for Hands United at the Latino Commission on AIDS. Prior to joining the Hands United at the Latino Commission on AIDS team, Carla worked at Duke University Hospital, as a bilingual research coordinator working with studies that were both local and global. Carla has extensive research experience in several fields including hepatitis C, HIV, immigration, LGBTQ+, childhood obesity prevention, neonatal vaccinations, and sexual and reproductive health. In addition, she has experience training people and partnerships on how to work with under-represented and under-served populations in the US. Some of those trainings include exploring social determinants of health, cultural humility, and health equity. She graduated from Meredith College with a BS in biology. Carla is a certified Culture Facilitator, Diversity to Belonging Facilitator and Culture Assessor. Overview: Loren Regier, a NaRCAD Expert Training Facilitator, joins us to reflect on nearly 25 years of his AD career, his experiences in learning AD for the first time, and his role in being a mentor to a new generation of academic detailers. Loren is a hospital pharmacist by training and has served with the RxFiles Academic Detailing Program and the Centre for Effective Practice, both longstanding Canadian AD programs. by Winnie Ho, Program Coordinator Tags: Detailing Visits, International, Program Management, Sustainability, Training  Winnie: We’re delighted to hear more about your AD journey, especially about the ways in which you continue to be a leader and supporter of the AD journeys of many others. Can you tell us a little bit about how you got started in this field? Loren: I was a hospital pharmacist doing a lot of work related to clinical decision-making, public speaking, and education. The Director for our Saskatoon Health Region (SK, Canada) had come across academic detailing from a colleague in Vancouver, and was interested in piloting something similar to what is now the British Columbia Provincial AD (BC PAD) Service. Our region needed someone who would take on this project and build something from scratch. Only partly knowing what I was in for, I said “yes”. To train and learn more, I had the chance to shadow Terryn Naumann in June of 1997. Terryn was the pioneering solo detailer in North/West Vancouver. What was initially a 1-year project for us, became a 2-year, and then a 3-year project, eventually morphing into an ongoing AD service that expanded to cover our province of Saskatchewan.  W: That’s incredibly fortuitous that you had Terryn to turn to for help! We’ve gotten to interview her before at DETAILS and know that she was a trailblazer for AD across Canada. Before I ask you about your experiences now as a mentor to others, I would love your reflections on your experiences as a mentee back in the days when you were learning AD as a new trainee with Terryn as your guide. L: There are both good days and difficult days to think back to – it involved a lot of hard work, but I was fortunate to have an awesome mandate and the opportunity to see another successful service in operation. Most importantly, I was able to see what a successful visit looked like. I joined Terryn for 7 visits over 2 days. After each visit, we reflected on how the visit went, what we liked, and if there was anything one might handle differently. The opportunity to shadow Terryn instilled in me the vision that academic detailing was about both relationship and service, and that clinicians could find both aspects valuable and enjoyable.  W: We do encourage a lot of new people starting AD for the first time to try and find someone to tag along with. You were especially lucky with Terryn because she had had a few years to build up her network and relationships in her community. L: Relationships are key in AD – and witnessing those relationships and the resulting AD conversations – was educational and inspiring. W: Is there a particularly strong piece of advice or a mentorship experience that sticks with you to this day? L: One of the things I recall is that she said, “One day, when you have a tough visit, I want you to call me, because I’m one of the only people who will understand what you’re going through.” Well, the day came when I had to call Terryn and we were able to debrief on a challenge I had faced. That was a critical moment that served to propel me forward with greater insight and confidence.  W: You bring up something important – our work is focused on creating safe learning spaces for providers in order to enact change. What we’ve been able to expand on are the connections between individual members of the detailing community. Luckily, the field has grown and new detailers have many more role models and teachers to learn from. Let’s also talk about this vulnerable moment, because it requires a lot of trust to go to someone when something goes wrong.  L: The mentorship process ideally involves deep, authentic discussions about being a detailer. Being a detailer involves constantly putting your best self forward. Trust allowed both of us to open up to each other with lots of safe space to discuss our different approaches and experiences. Trust is essential for effectively exploring differences of opinion, and how to turn challenges into opportunities. Without it, you don’t get to understand where someone is coming from or to truly grow and learn. In addition, I need to mention Frank May who also became valued mentor over the years. Frank helped pioneer academic detailing in Australia. His thoughtful conversations and leadership were instrumental in my growth in AD, as well as my eventual role in helping train and mentor new detailers.  W: I have definitely seen the large and small ways that mentorship has propagated through the AD community. In the process of learning and educating others in this field, we never truly stop being mentors or mentees – it’s not a binary. It’s a great lifelong process. Let’s flash forward to now: given your experiences, how have you continued to integrate mentorship into your current work? L: A big part of my role these days has been training, mentoring, and supporting others - both academic detailers and those who are moving into program leadership. It’s important to recognize that the world needs more people to do this kind of work and that we need to pass the baton. That involves coming alongside their journey, having good discussions, and being able to dig deep into those critical ingredients for success.  It has meant being transparent about my decisions and leadership so that my team can not only see how I’m thinking and processing things, but also provide their own input and ideas. Being a mentor to me means modeling the approach of learning together and working enthusiastically and collaboratively when pursuing opportunities. W: You’re in a capacity now where you’re training future leaders in AD. You provide an important link and opportunity to reflect on where AD has been, but also the space to give new AD folks a chance to figure out where AD may go next. The people you mentor now will likely go on to mentor others, just as Terryn and Frank did for you. What advice would you give to those who are seeking to be strong mentors?  L: People can sense if they are respected and valued. If they know you care and are interested in their growth, they will open up, share the important stuff, and work together to address the challenges of academic detailing. If you add some fun and enjoyment along the way, the process serves as a model of what will eventually happen between the detailer and those they detail. W: That’s wonderful advice, because one of the best things you can do for someone who is learning is to fully believe in their potential and strengths. They’re already a part of your team – they’re there for a reason.  L: Somebody once asked the coach for Bobby Orr, one of the greatest Canadian Hockey players of all time, “How do you coach Bobby Orr?” and the reply was, “You don’t coach Bobby Orr, you give him room to play the game.” There’s some truth in applying that to leadership and in AD. You need to appreciate where your team members excel and empower them. It means coming alongside, supporting their input, and also giving them the freedom to make their own mistakes and learn from them. Give people the support they need to do best. They’ll show you what they’re capable of. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  LoLoren Regier is a Pharmacist and Consultant Editor with RxFiles Academic Detailing Service in Saskatoon, SK, Canada. Loren has guided the development of this provincial academic detailing service since the first “ground breaking” pilot project began in 1997. Loren is active as a member of the Canadian Academic Detailing Collaboration and provides training and consultation to various programs and initiatives. Loren’s interests cover the practical application of evidence to practice and the ongoing development of multifaceted interventions that support academic detailing. Additionally, Loren serves as a faculty facilitator for NaRCAD’s Academic Detailing Techniques trainings. Loren is co-editor of the RxFiles Drug Comparison Charts – 10th Edition and a contributor/reviewer for Geri-RxFiles and the RxFiles – Bringing Evidence to Practicesection of Canadian Family Physician journal. Loren obtained his degree from the University of Saskatchewan, College of Pharmacy in 1988 which he followed with a hospital pharmacy residency. He serves as a lecturer, instructor and preceptor in the areas of evidence informed drug therapy decision making, educational outreach and chronic pain management in a wide variety of professional settings This interview features Carla Foster, MPH, who leads the conceptualization, implementation, and evaluation of Public Health Detailing as an Epidemiologist within the Bureau of Alcohol and Drug Use Prevention, Care and Treatment (BADUPCT) at the New York City Department of Health and Mental Hygiene (NYC DOHMH). She is currently activated for the COVID-19 emergency response as Lead Analyst managing the Reporting Unit within the Integrated Data Team of DOHMH’s Incident Command System. By Winnie Ho, Program Coordinator Tags: Data, Detailing Visits, Evidence-Based Medicine, Health Disparities, Program Management, Stigma, Substance Use, Training  Winnie: Hi Carla! You’ve certainly had a lot on your plate with so many diverse campaigns. Can you walk us through the conceptualization process for your detailing campaigns, and how your team came to choose cocaine use as your current detailing topic? Carla: We can start with some data on this. In 2018, more New Yorkers died from drug overdose than from homicide, suicide, and motor vehicle crashes combined. Cocaine – in both crack and powder forms – has played an increasingly prominent role in this crisis. The mortality rate from overdose deaths involving cocaine more than doubled between 2014 to 2018, amounting to 52% of all drug overdose deaths in NYC. Some of the associated risks are serious - increased exposure risk to fentanyl, cardiovascular disease events and death.  W: That’s stunning data. Especially in the midst of the opioid crisis, it’s important that we don’t lose sight of other substance use issues going on right now. I’d love to learn a little more about the challenges and lessons that your team has learned by detailing on cocaine use. C: First, we have to be aware that fentanyl, a powerful opioid 50 to 100 times stronger than morphine may be found in many substances, including cocaine. We’re very concerned about fentanyl and cocaine because people who use cocaine do not have tolerance to opioids and are at even higher risk for overdose. It’s also important to address the perception of who is most impacted by high mortality rates. There’s this idea that cocaine use is more prominent in younger populations, but our data show that it’s actually impacting an older population more than many might expect. In particular, residents age 55-84 in the Bronx Borough have experienced the largest increase in cocaine overdose death rates in New York City from 2014 to 2018.  That’s why it’s critical for us to raise awareness in an effort to mitigate misconceptions and stigma around risky use and those who may have a substance use disorder (SUD). In addition to shame, there are still very real potential socioeconomic and legal consequences from disclosing substance use, which can deter folks from even seeking help. We take into account the unjust consequences of policies applied unevenly according to race, and how this impacts implicit biases in terms of which patients are thought to use substances, which types of substances they might use and even more critically, which type of treatment, if any, they are offered. Implicit biases combine with the effects of systemic racism to compound these consequences. It’s important to note that it’s not race that drives poor health outcomes, but racism.  W: Challenging stigma is one of the most powerful ways that detailing campaigns can combat the damage done by the War on Drugs, because stigma can make the difference of whether or not people receive dignified care. With a campaign so focused on addressing stigma and with a topic this important, how do you prepare your detailers for this task? C: We devote a significant amount of time towards training our detailing reps – a week-long training, 8 hours a day. We spend a large amount of that time talking in detail about stigma as related to cocaine use. It’s critical to us that our detailers are comfortable and knowledgeable when speaking about this topic, because it sets the tone for the providers who then set the tone for their patients. We ensure that our representatives are prepared to respond to a wide range of questions or comments, because this builds the provider-detailer relationship and enhances the value of the detailing visit. We’ve found during our follow-up visits that this support has led to high provider engagement with the campaign and providers reporting incorporation of the key recommendations into their daily practice, which is the aim of our public health detailing campaigns.  W: How have providers responded when detailed on a topic that carries so much stigma? C: The good news is that we’ve found NYC healthcare providers to not only be receptive to our work on substance use, but they’re eager to partner with us to support their patients once they learn about the severity of the issue. Our team provides statistics that relate to the provider’s specific neighborhoods and specialty, giving them real-time pictures of what’s happening with the patients they see. We know that it’s still a difficult topic to bring up, so we help address this with our action kit resources on stigmatic language and counter-top brochures that signal to patients that the provider’s office is a safe place to discuss these issues.  W: It gives me tremendous hope to hear about that there’s been enthusiastic response from providers. It means that things are changing. Let’s also talk a bit about program sustainability. Your team has worked extensively on campaigns across multiple topics. What have you learned from implementing past campaigns? C: Each public health detailing campaign is different, but we’ve learned some key strategies that support the growth and success of subsequent campaigns: 
Our overall goal is to do everything we possibly can to improve the health of our fellow New Yorkers. I like to remind our detailers of this James Baldwin quote that informs our public health detailing mission: “Not everything that is faced can be changed, but nothing can be changed until it is faced.” Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Carla Foster, MPH is an Epidemiologist at the New York City Department of Health and Mental Hygiene (NYC DOHMH). Her research focuses on the implementation and evaluation of public health detailing campaigns across New York City with the aim of reducing overdose mortality. Prior to joining the NYC DOHMH, she led development of clinical practice guidelines at the American Urological Association. She received dual Bachelor of Arts degrees in Africana Studies and Neuroscience from Wellesley College. Carla also obtained her Master of Public Health Degree in Epidemiology from Columbia University. An interview with Sarah Ball, PharmD, Research Assistant Professor, Division of General Internal Medicine, Medical University of South Carolina and Megan Pruitt, PharmD, Clinical Pharmacy Consultant, SCORxE Academic Detailing Service and Assistant Professor, Department of Clinical Pharmacy and Outcomes Sciences, Medical University of South Carolina by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: COVID-19, Opioid Safety, Stigma, Substance Use, Training  Anna: Hi Sarah and Megan- thanks for taking the time to chat! Can you tell us a bit about your program, SCORxE, and how your AD work has concentrated on improving opioid safety? Sarah: SCORxE began in 2007 as an academic detailing service at the South Carolina College of Pharmacy and is now part of the Medical University of South Carolina (MUSC) College of Pharmacy. Our current efforts are around addressing the opioid epidemic. We’re fully funded by the South Carolina Department of Health and Human Services, and our agreement talks about bringing together quality initiatives for safer opioid prescribing and expanding access to MAT. We’ve been able to effectively bring together quality initiatives from different state agencies that span prevention and treatment. This braiding has been a unique experience for our academic detailing service. Regardless of the specific topic, our detailers promote opioid risk reduction strategies, help recruit and support MAT providers, and work to reduce stigma around MAT. We’re currently shifting our focus from chronic pain to acute pain. We’ll be detailing both primary care providers and surgeons on post-surgical pain. Anna: Detailing surgeons is a unique approach – we’d love to hear about the results of that process in the future. And you’re working on other topics outside of opioid safety, too – tell us more. Sarah: Our providers always welcome new topics. While our focus is on the opioid epidemic, we try to expand our content reach when possible. We recently detailed on depression and anxiety screening, and touched on alcohol use disorder in our topic on naltrexone. We’ve always offered CME credits and our current strategy is shorter and more focused visits that offer a half hour of CME credit, as opposed to one or two hours of credit. This allows us to have multiple visits with each provider and to individualize next topic selection. Megan: As a detailer, it’s helpful to have a menu of shorter topics that providers can choose from – it makes our visits more flexible.  Anna: Speaking of flexibility - how are you continuing to detail and run your program given the current COVID-19 pandemic? Sarah: We haven’t previously engaged in virtual visits or e-detailing. We’re planning to reach out to our network of academic detailing colleagues who’ve had e-detailing visits in the past to see what their experience has been like. It’s times like these that show how valuable it is to have a network of academic detailing services. Being able to share ideas and find out what other folks have done will help us determine what will work best in our state. Megan: We’ve been using the past few weeks to work on creating materials and scripts for upcoming topics. It’s been a good time to refresh on a lot of our content and update various internal documents. I’m going to begin reaching out to providers within the next few weeks and gauge their interest and comfort level in using a virtual platform. Sarah: We know this is a difficult time for primary care providers, so it’s important for us to be compassionate in how we go about scheduling visits. We want to be sensitive to our providers’ time and respect what they’re going through, while still offering our detailing service around topics related to the opioid epidemic.  Anna: You’re not alone in figuring out this balance! You also mentioned that peer learning is an important component to a successful intervention. Can you tell us about your own peers on your team, and how they enhance your overall detailing service? Sarah: Our program is under the College of Pharmacy, so we’ve recruited all our detailers from there and they’ve all been clinical pharmacists. We’re fortunate to have pharmacists because they’re well-respected among providers we visit. We have two full-time detailers, which is a privilege, and they’re very passionate about their work. Being able to have two people fully commit to detailing is far greater than the number implies. Both of our detailers have different personalities and different experiences to share – I think they complement each other very well! Detailing can be lonely, though. When you have more detailers in your program that add up to two full time equivalents, what we have had in the past, you have more people sharing experiences during debriefs and more people to bounce ideas off; there are pros and cons to both scenarios.  Megan: My colleague, Lauren, and I come from different clinical backgrounds. When we work on our content development and role playing, we’re able to help each other consider things differently. It’s been fun to work with somebody who differs so much from me! Anna: It sounds like you balance each other out well. How are the detailers in your program trained? Sarah: All of our detailers have gone through pretty intense academic detailing training on the marketing of evidence-informed clinical ideas. Our most recent hires have gone through NaRCAD training, but before there was a NaRCAD, our pharmacists went through a training developed by a group in Australia. That training gave us a step up on everything when we first started our program, as NaRCAD also does with programs just getting started. We garnered our baseline of how we develop content, how we develop our supporting materials, and essentially how we put together our whole intervention. Anna: It sounds like the detailers in your program are trained well and prepared for the field. Do you have certain strategies for getting in the door? Are there key stakeholders who your program has connected with that have helped you to do this? Megan: Showing up at the office has repeatedly proven to work for us. We bring a letter to share with the first gatekeeper at the front desk, so that we can get face-to-face time with the providers for introductions. We’re usually able to schedule a meeting fairly easily after that. If we can’t meet with the provider face-to-face, we try to speak with the Office Manager. Recently, we’ve been leveraging our group presentations at clinics to get more 1:1 visits. We try to promote our detailing visits during our presentations and grab contact information from providers afterwards. We’ve also found that it’s been helpful to stay in the break room at an office after a visit - we might stay there all day and introduce ourselves to a number of providers who end up wanting to either schedule a visit that day or in the future. We’ve found great success in being present for providers when they’re ready.  Sarah: When you can get face-to-face with the providers for a brief introduction, it’s a beautiful thing-it’s how we’ve gotten most of our visits over the years. When we first started, gaining access happened in different ways. We had champions in the area that supported what we were doing, and we could use that to get our detailers in the door. Our program was also previously part of a demonstration project where providers were required to have an academic detailing visit as part of the initiative. I would say that our cold calls became “warm calls” during that time because all the offices and providers knew we were coming. Anna: I’m sure having providers in the area know about your detailing service has helped to build your program. Can you tell us more about how your program is working towards sustainability? Sarah: We’re more sustainable than we’ve been for a while. Part of that is due to the funding that we have for opioid-related topics, but it’s also been due to the effort our program has put into effectively bringing together different quality initiatives over the years. We’ve had funding come in from multiple sources in that process. One agency asked us to take on the topic of naloxone for pharmacists--our ability to respond to such requests helps up strengthen relationships, and may help us with future sustainability. It is also important that our interprofessional teams at MUSC see value in academic detailing. Additionally, our detailers help us with sustainability through their visit documentation and tracking. The data they collect is included in our reporting and helps illustrate the value of academic detailing. Our clinical pharmacists are amazing people, and they both bring so much to what we do in the academic detailing world– programs are only as sustainable as the strength of their individual detailers!  Biography. Sarah Ball, PharmD is a Research Assistant Professor in the Division of General Internal Medicine at the Medical University of South Carolina (MUSC), with a focus on patient-centered care, patient safety, and educational outreach. She has had direct involvement with academic detailing for over twelve years, beginning with the development and implementation of the SCORxE Academic Service under the SC College of Pharmacy in 2007. Current efforts include the integration of research and programmatic opportunities to identify interventions that change prescriber behavior to reduce the risk of opioid overuse, misuse, abuse, and overdose. Dr. Ball is currently leading the MUSC team partnering with the South Carolina Department of Health and Human Services for the provision of drug utilization review (DUR) services, which includes educational outreach to primary care providers and surgeons. Dr. Ball has twenty plus years with a career focus on improving patient care through the application of technology and effective communication of clinical knowledge, information, and data-derived findings. She is a graduate of the Medical University of South Carolina, where she received both a B.S. in Pharmacy and Pharm.D.  Biography. Dr. Megan Pruitt is a South Carolina Offering Prescribing Excellence (SCORxE) clinical pharmacy consultant and assistant professor in the Department of Clinical Pharmacy and Outcomes Sciences at the Medical University of South Carolina in Charleston, South Carolina. She received her bachelor of science in health science from Clemson University and her doctor of pharmacy from the South Carolina College of Pharmacy. She has published an Amazon ebook, Catalyst (pharmD): The Next Generation Pharmacy Student, and has previous experience as a community pharmacist at Federally Qualified Health Center in South Carolina. In her current role as a SCORxE clinical pharmacy consultant, she provides academic detailing visits to primary care providers on monitoring practices to promote safe opioid use and to reduce the risk of misuse and abuse in South Carolina. An interview with Brandon Mizroch, MD, MBBS, Provider Network Supervisor, Louisiana Department of Health by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Hepatitis C, HIV/AIDS, PrEP, Rural AD Programs, Sexual Health, Stigma, Training  Dr. Mizroch participating in a NaRCAD training Dr. Mizroch participating in a NaRCAD training NaRCAD: Thanks for chatting with us today, Brandon! We’re excited to be catching up with you. Can you tell us about your program at the Louisiana Department of Health and the work you’re currently doing? Brandon: Absolutely. I was hired to do work around PrEP and PEP, detailing providers across the state of Louisiana, in 2017. Since then, my role has expanded and I promote education for providers about syphilis, congenital syphilis, and Hepatitis C. Our department now has 3 detailers, including myself. Louisiana became the first state in the country to undergo an incredibly revolutionary Hepatitis C Elimination Plan, which has caused my detailing focus to shift. There’s been huge advancements in the drugs that treat Hepatitis C, but they’ve been inaccessible to much of the population due to cost. We negotiated a fixed rate price for Hepatitis C treatment and can now treat 100% of the population, compared to the 3% of the population we could treat previously. There’s been a big push to identify and train providers who’ve never previously treated patients with Hepatitis C. I’ve been leading the charge by getting the word out, running symposiums, and working with the marketing team that’s creating our statewide campaign.  NaRCAD: Wow, that sounds like innovative and exciting work. Can you explain your program’s approach a bit more? Brandon: I try to blend a few different approaches together. I attended the NaRCAD training during my first year as a detailer. NaRCAD built the foundation of detailing for me. I always use the NaRCAD methodology to get my foot in the door and identify providers who can be champions within their practices. I find it much easier to follow up and do longer didactic sessions about complex clinical topics when I use the techniques of academic detailing during my first face-to-face visits with providers. I connect with about 20 providers in this 1:1 model each month. I also work with residency programs, hospital systems, and present at Grand Rounds to expand my reach. There’ve even been instances where I’ve attended dinners for physicians that are hosted by pharmaceutical companies to network and identify new clinics that would benefit from detailing. NaRCAD: We’re happy to see that you’re blending academic detailing with other approaches. Do you provide follow-up to providers after your visits? Brandon: Follow-up is incredibly important, no matter what approach is being used. I like to send an email after each visit that includes digital resources for both providers and patients. I also offer providers the ability to call, text, or email me because of the apprehension that exists around topics where the knowledge base is still growing. Maintaining relationships with providers also ensures that we have a strong provider network that we can continue to educate on other clinical topics down the road.  NaRCAD: Building a connection with providers is imperative, especially as you move into different clinical topics. Your program spans the entire state. Do you find that there’s a difference when you provide clinical outreach education in rural vs. urban communities? Brandon: Yes, there’s certainly a difference. The providers in urban areas tend to have a higher knowledge base when it comes to PrEP and syphilis, perhaps due to marketing efforts or higher patient loads. This makes starting the conversation a bit easier. Additionally, urban communities have access to navigators, who help with non-medical aspects, like transportation issues, lack of health insurance, and long commute times that all prevent folks from getting the treatment they need. Providers in urban areas are also busier and easily distracted during 1:1 visits, which can make detailing a bit difficult. On the other hand, rural communities are quite the opposite. Providers tend to have more time in their schedules and are excited to sit down with somebody from the state office. They’re eager to learn, but there’s typically less of a knowledge base, making it slightly more difficult to start the conversation. I’ve also learned about patient barriers as well, which affect access and provider care. Patients in rural areas are often friends or family with those throughout the community, including those who work at clinics. The notion that you would know the receptionist or provider at a clinic is enough to deter folks from seeking medical care around a topic like sexual health. To encourage access, our state has created a TelePrEP program that offers PrEP services to anyone via telemedicine. Consultations take place over the phone, labs are obtained at third party lab companies, and medications are mailed right to the front doors of patients. It was originally created to help folks in rural communities who face stigma-related barriers, but we’ve expanded the program across the entire state of Louisiana. It’s a great referral service that I can share with providers.  NaRCAD: It’s wonderful that you’re able to identify these challenges and have resources and tools to address them. What’s one piece of advice you’d give to folks who are detailing on a similar clinical topic or have a large geographical region to cover? Brandon: It’s important to have several different ways of presenting information to the providers you’re detailing and to use varied approaches depending on the barrier(s) they’re facing. I typically focus on emotional connection, financial concerns, and the evidence and science behind the key messages I’m delivering. I’m also ready for provider resistance, and am prepared to address it, which is something I learned from NaRCAD. When it comes to detailing over a large and diverse geography, it’s always necessary to plan ahead. My general rule of thumb is that however many hours it takes to drive to a location, that’s how many providers I want to meet with while I’m there. I typically try to use larger educational events, like meetings with clinics over lunch, as my anchor point for longer trips. After I have that scheduled, I search for smaller clinics around the area where I can meet with providers 1:1. It’s all about maximizing your time.  Biography. Brandon Mizroch received his MD/MBBS from the University of Queensland/Ochsner Clinical School Program in November of 2016. Since taking over as the PEP/PrEP Provider Outreach Specialist at the Louisiana Department of Health in August, 2017, he has worked with hundreds of doctors statewide on HIV prevention best practice. Since then he has expanded his educational base and now serves as the head of the academic detailing department at the Louisiana Department of Health, Office of Public Health, STD/HIV/Hepatitis program. As the Provider Network Supervisor he has helped lead the provider Outreach for the state’s first-in-the-nation Hepatitis C Elimination program. From grand rounds presentations at LSU-Shreveport Hospital and Baton Rouge General, to state-wide symposia and conferences, to one-on-one counseling encounters at dozens of clinics all over Louisiana, he has helped spread awareness and education on HIV prevention, syphilis screening and treatment, and HCV screening and treatment through evidence-based care. Wearing Multiple Hats at Alosa Health: Detailing Clinicians, Managing Programs, and Training Staff1/22/2020 An interview with Tony de Melo, RPh, Director of Clinical Education Programs, Alosa Health by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Detailing Visits, Opioid Safety, Program Management, Training  NaRCAD: Tony, thanks for chatting with us today about your role at Alosa Health! What’s been the most exciting part of the work that Alosa has done this year? Tony: Our partnership with Aetna, a managed health care company and health care insurer. We’ve been working with them to provide educational outreach to providers on chronic pain, acute pain, and opioid use disorder (OUD); supporting them in managing pain using non-opioid drug options; appropriately dosing opioids when they need to be used; tapering down patients who are on existing high doses of opioids; and helping to identify patients that may have opioid use disorder. We’re now working in Pennsylvania, Virginia, West Virginia, Ohio, Illinois and Maine. NaRCAD: That collaboration does sound exciting! Now, let’s talk a little about your role at Alosa. You actively detail, you manage academic detailers in the field, and you lead trainings at Alosa. Which aspect of your role is your favorite, and why? Tony: When I’m training and managing detailers, I see myself more as a coach than a trainer. I’ve always liked educating and teaching—I enjoy helping others develop their skills and seeing them improve. Training folks and coaching them in the field is rewarding to me because I feel that I’m impacting what they’re doing in their own communities. It brings me happiness to see others succeed. NaRCAD: As a coach, how do you know when your work has been impactful? Tony: When I work with detailers in the field, I can see firsthand that they are able to be impactful with the providers because they are bringing about behavior change with their message delivery and confidence. We can also measure how impactful our work is by reviewing our Salesforce data. I can see from the detailer’s visit notes when providers have agreed to a behavior change, and this is a true measure of our work being impactful.  NaRCAD: With success comes challenges. What are some of the major challenges you see academic detailers face in training and in the field? Tony: The major challenge is teaching detailers to have a conversation with clinicians rather than a lecture. Making the visit more conversational doesn’t often come as naturally as presenting the information in a lecture format, but the conversation must be about understanding where the provider is now, what their needs might be, and how to deliver content to make behavior change. In the field, the major challenge is access to providers. Many health systems have regulations and restrictions for those who want to meet with providers, because representatives in the pharma industry have bombarded and overloaded providers throughout the years. As a result, we’re often seen as an outside influence or an outside visitor, so we aren’t always given the opportunity to meet with a provider. NaRCAD: With these challenges in mind, how do you instill confidence in academic detailers as a trainer and as a manager? Tony: We spend a lot of time practicing and providing feedback during trainings. We practice individually, with partners, and with outside folks who are playing the role of providers. Practicing multiple situations, multiple times, over multiple days, builds confidence. We also videotape the trainees so that they can see what they’re doing well and what they can improve upon. As a manager in the field, it’s quite similar. I usually sit down with each detailer after a visit and discuss what worked well and what they could do differently in their next visit, so that each visit becomes a learning opportunity. Providing feedback and being a mirror for the detailers helps them to build confidence and skills as time goes on. I also offer the detailers my perspective; having spent time doing this myself and observing others, I can share the tricks, skills, and wording I’ve heard throughout my time with the detailers.  NaRCAD: Those are all great ways to build confidence among detailers. What’s one piece of advice that you would give to academic detailers? Tony: Don’t be afraid to ask for a specific behavior change, and remember to follow up to make sure that the behavior change occurs. One thing that I find to be hard for academic detailers is the “ask”, where detailers are asking for commitment or behavior change from a provider at the end of the visit. I always tell detailers to frame it as, “based on what you’ve heard today, what is one thing you’d do differently?” Follow-up then ensures that providers are committed to change and holds them accountable for what they said they would do. NaRCAD: That’s extremely helpful advice for detailers. What’s the best thing a program manager could do to maintain high levels of engagement among detailers? Tony: As a manager who’s coaching or guiding others, it’s important to build trust between yourself and the folks you’re coaching or managing. It can be lonely when you’re in the field detailing by yourself, so managers need to have touchpoints with their detailers. Building trust and having your detailers know you’re all working together helps them stay self-motivated; it makes them want to go out into the field and do a good job because they know someone is backing them up. NaRCAD: Thank you for taking the time to chat with us today. We value your unique perspective on detailing, managing, and training!  Biography. Tony de Melo manages field staff and leads academic detailer trainings at Alosa Health. He attended Massachusetts College of Pharmacy and Health Sciences in Boston, where he received a BS in Pharmacy with a minor in Business Administration. This business interest led him to work for several pharmaceutical companies as a sales representative, account manager, training manager, district/regional manager, associate director of managed markets training, head of sales training, and development & marketing product manager. He has also worked for smaller businesses that were looking to grow their sales and marketing programs. Throughout his career, Tony has successfully sold, marketed, trained, led, designed, developed and executed solutions to meet business objectives.  Director's Letter | Mike Fischer, MD, MS, Director of NaRCAD Tags: Director's Letter, HIV/AIDS, Opioid Safety, Training As NaRCAD enters its 10th year as the only national resource center dedicated to clinical outreach education, we’re ready to take our collaborations with you to the next level. The strength and sustainability of NaRCAD has grown from the hard work we’ve done together with you, our community members in the field. We’re committed to continuing to provide the technical assistance you need to make your programs innovative, efficient, and successful. As we kick off 2020, our entire team at NaRCAD invites you to join us in leading our field forward through strategic partnerships, resource-sharing, and peer learning, all to implement important initiatives that will have a significant impact on clinicians and their patients. The nature of our role as a resource center has continued to grow in parallel with increased recognition of the importance of academic detailing as a strategy to address multiple clinical challenges. We’ve been especially excited to see the effectiveness of AD enhanced when aligned with other initiatives to improve the quality of care. Responding to this growing demand, we’ve dramatically expanded our reach, conducting 20 trainings in 15 different states across the US in the past two years alone, and 2020 looks to be no different. With the increased demand for AD technical assistance, we have a busy year ahead of us, from capturing your successes and sharing them via our DETAILS Blog to training your detailers to be ready for field work (and troubleshooting challenges along the way.)  Along with continued trainings across the US to improve opioid safety in partnership with states supported by the CDC’s Overdose Data to Action (OD2A) grants, we’ll also continue the important work of training new detailers to educate clinicians about using HIV PrEP to reduce the risk of new HIV infections, also through CDC-funded programming. We’re equally excited to have launched a new CDC research grant in collaboration with the Oregon Health Authority to rigorously evaluate the impact of their OD2A intervention and to develop a model for pragmatic assessment of similar efforts in other states. If you’re also interested in evaluating the impact of your AD program, reach out and let us know—we’re eager to hear from you.  Although we have been conducting more trainings recently, we see the demand for them continuing to grow at an even faster pace. As we grow, so does our core team, and all of us are dedicated to amplifying the impact of the important work you do. We’re already starting to plan for NaRCAD2020, our 8th annual conference, and we invite you to consider submitting your ideas and innovations when we start accepting submissions on March 1, 2020. But you don’t need to wait until then—we’re here to offer you customized support to strengthen your program, as you plan for success in 2020 and beyond. Happy New Year! -Mike Biography.
Michael Fischer, MD, MS, Director, NaRCAD Dr. Fischer is a general internist, pharmacoepidemiologist, and health services researcher. He is an Associate Professor of Medicine at Harvard and a clinically active primary care physician and educator at Brigham & Women’s Hospital. With extensive experience in designing and evaluating interventions to improve medication use, he has published numerous studies demonstrating potential gains from improved prescribing. Read more. Guest Blog Interview: David O’Riordan, MPharm, MPH, PhD Senior Pharmacovigilance Officer Pharmaceutical Care Research Group University College Cork, Ireland Tags: Detailer Visits, International, Training  NaRCAD: Thanks for speaking with us, David! Tell us a bit about your professional background in healthcare, and how you became involved in academic detailing. David: I am a pharmacist by training, and a couple years ago I decided to carry out a PhD in Clinical Pharmacy at the University College Cork. As part of the PhD, I completed a systematic review examining how pharmacists can be utilized to optimize prescribing in primary care, including through academic detailing. After finding NaRCAD’s resources through a Google search, I registered for the NaRCAD conference in Boston. Dr. Fischer, Dr. Avorn, and all the other attendees at the conference were very encouraging. I left the conference determined and enthused to lead an academic detailing intervention back home. Dr. Avorn and Dr. Fisher put me in touch with Eimir Hurley, a PhD scholar in Ireland, who formerly worked in academic detailing at Alosa Health, and who ended up being a great help in executing the intervention.  NaRCAD: That’s terrific—it sounds like you had a great team at your disposal to begin this work. Can you tell us a little about the unique characteristics of the Irish health system? David: Ireland has a public and private health system. Public patients are more likely to wait longer for appointments. Private insurance is a substantial cost to individuals, though. The health care system is quite fractured unless you’re a private patient. Pharmaceutical drug representatives are also allowed to visit primary health practices here. NaRCAD: In April, you published a study titled “Pharmacist-led academic detailing intervention in primary care: a mixed methods feasibility study” in the International Journal of Clinical Pharmacy. Why did you choose urinary incontinence as a clinical topic? David: As this was a feasibility study, I decided to use one topic as part of the intervention. I organized a meeting with a group of general practitioners (physicians) who would be involved in the academic detailing intervention. The topic of urinary incontinence was chosen by the physicians because they highlighted that it was a topic not discussed regularly among themselves, and currently their only source of information is provided by pharmaceutical drug representatives.  NaRCAD: What barriers to success did you come across in your feasibility study? David: For this project, I was the only academic detailer. I started detailing after going to the two-day Basics Academic Detailing Training in Boston in May 2016. In some cases, during the roll out of the intervention I found it difficult to get past the practice manager, but luckily I had learned strategies on getting in the door in Boston that were useful in my effort. On a few occasions, the practice managers didn’t follow through on connecting me with the physicians. I got around this by utilizing physicians I knew in other practices to gain access to their practice. A lot of it came down to how well you know the physicians. I was lucky that they trusted me when I spoke to them. When I did get to meet with physicians, they all seemed very enthusiastic. NaRCAD: Can you talk a bit more about how receptive physicians were to academic detailing? David: Absolutely! This was a mixed methods study, so my colleague Eimir Hurley carried out focus groups after my detailing sessions to evaluate the feasibility of the intervention. Eimir conducted the focus groups on my behalf to reduce bias. The physicians liked that I wasn’t from a pharmaceutical company and that the sessions only lasted 10-15 minutes. They liked that local physicians had chosen the topic, and I wasn’t coming with my own agenda. NaRCAD: How are you or others going to use your feasibility study results to implement across the country? David: I am currently not involved in academic detailing, but I hope to be again in the future. If someone from another part of Ireland read my paper, they would recognize that physicians are very willing to take part in academic detailing. From my experience physicians didn’t feel threatened and really enjoyed the interaction. They liked the interactive style of the visits, and the way that that the evidence was delivered. My study provides a platform for other researchers to detail to a wider group of physicians in Ireland. NaRCAD: Anything else? David: I am very grateful for the NaRCAD team for providing the academic detailing training. I knew literally nothing about academic detailing, and through meeting their team members Sarah Ball, Amanda Kennedy, Mary Liz Doyle-Tadduni, and others, I felt encouraged to go back and detail. I was the only person from Ireland at the training, and the NaRCAD team gave me some useful feedback. I really enjoyed academic detailing, and I was especially proud when my paper was published. I discovered there is an appetite for this educational intervention in Ireland.  Biography David O’Riordan, MPharm, MPH, PhD Senior Pharmacovigilance Officer Pharmaceutical Care Research Group University College Cork, Ireland David holds a Masters in Pharmacy (MPharm), Masters in Public Health (MPH), Post Graduate Certificate in Teaching and Learning in Higher Education (PG Cert) and a PhD in Clinical Pharmacy. He has extensive experience as a community pharmacist. He previously worked as a Lecturer in Clinical Pharmacy in University College Cork (UCC). While there, he contributed to and assisted in the delivery of research-led teaching at undergraduate and postgraduate level. He also supervised on a number of research projects. He was a clinical trials pharmacist involved in the Thyroid Hormone Replacement for Subclinical Hypo-Thyroidism Trial (TRUST). This was a randomised placebo controlled clinical trial comparing levothyroxine to placebo in community dwelling older adults (≥65 years) with subclinical hypothyroidism (SCH). He is also a tutor on the Irish Pharmacy Union (IPU) Academy. This educational initiative was developed by the IPU to support pharmacist engagement with Continuous Professional Development (CPD). He is currently the Senior Pharmacovigilance Officer at the HRB-Clinical Research Facility, UCC.  Tags: Conference, Training Summer's officially here, and we're excited for what lies ahead in public health, especially when it comes to what clinicians can do to improve their patients' health. Here at NaRCAD, our work encourages front line care providers to think differently when it comes to opioid safety, sexual health and STI prevention, cancer control, reducing overmedication for the elderly, and much more. For health educators who provide 1:1 outreach to clinicians, NaRCAD provides hands-on, intensive training, so that these educators can make an impact when bringing the best evidence to front line staff. If you haven't been to one of our trainings, we've just opened registration for our September 23 & 24th, 2019 session here in Boston, where you'll spend 2 days with us, learning how to effectively and persuasively communicate with doctors, nurses, and pharmacists, helping them to increase the chances that their patients will have better health outcomes.  Space fills up fast, so register today, and join other health professionals from across the US who are looking to strengthen clinician care in their communities. After the training, you can bring the interactive interpersonal communications skills of academic detailing back to your health system or local health department to roll out interventions to support chronic disease management, substance use disorder, HIV prevention, and many other critical clinical topics. And if you're already in the field doing this important outreach work with providers, we want to hear from you, and feature you on the DETAILS Blog. Better yet, join us this November 7 & 8, 2019 at our 7th Annual International Conference on Academic Detailing and share your work with our community. Meet others who are advancing the field, infusing clinical care with the best evidence-based tools and approaches in health care.  Want to hear from our community members? And keep your eye on our Twitter feed, and check our News & Media Center for our latest e-news and CoRE Podcasts, or browse the DETAILS archives to the right for more stories from the field. For our part, we'll be adding new stories this summer on successes and challenges in implementing academic detailing in partnership with our colleagues at CDC and NACCHO to support patients dealing with opioid use disorder and pain management. and we'll be hitting the road to train new detailers in Kansas this August. Stay tuned! Happy Summer! The Team @ NaRCAD Share your work in public health with us. What's happening in your community around the opioid crisis? HIV prevention? Patient education? Have an idea you'd like to hear more about on our next Podcast? Want to share new ideas or challenges related to public health detailing? Sound off below.  An Interview with Johnathan Goree, MD Director of Chronic Pain and Opioid Stewardship University of Arkansas for Medical Sciences NaRCAD Training Alumnus by Kristina Stefanini, Program Coordinator at NaRCAD Tags: Detailing Visits, Opioid Safety, Training NaRCAD: Thanks for talking with me today! Can you tell me a little bit about yourself and how you ended up in pain management? Johnathan Goree: I’m from Arkansas originally. After completing college at Washington University in St. Louis, medical school and residency at Cornell, and a pain medicine fellowship at Emory, I was recruited to start the chronic pain division at the University of Arkansas for Medical Sciences – 2 miles away from where I went to high school. I’m proud to work in Arkansas; Arkansas is such a poor and rural state, so we don’t often have the resources that other states have.  I went into anesthesiology because I wanted to be the best prepared doctor for an emergency, but I moved into pain medicine because I missed the 1-on-1 patient contact and longitudinal patient care. Here are some other things that lead me into pain medicine. After getting my wisdom teeth removed, I was given too much fentanyl during the procedure resulting in being given Narcan to wake up. That was the first time in my life I experienced 10/10 pain. It allowed me to understand how pain can completely dominate someone’s consciousness. I am also passionate about pain management in minority communities. Many in those communities feel that their pain is undertreated, and evidence backs that up. NaRCAD: As a physician, what are some of the barriers that detailers may have talking to clinicians about pain management? How can these be navigated? Johnathan Goree: Every physician will say the number one barrier is time. While most physicians are excited to learn about anything that will improve patient care, unfortunately, physicians are usually not in control of their schedule.
NaRCAD: How can clinicians act as champions in an academic detailing campaign? Johnathan Goree: One way physicians can help is with the crafting of educational materials. Physicians know how physicians think and can help by crafting a message that may better catch attention. Another is by dedicating time to answer follow-up questions from detailers and other clinicians. In my field of chronic pain management, detailers that don't have a clinical background may not know how to answer questions on specific off-label situations or treatment of specific pains. A follow-up visit or call with a clinician can help with that. NaRCAD: Anything else you’d like to add for our readers? Johnathan Goree: More praise for you guys – your course is excellent! Really understanding the science and method behind academic detailing made me excited to be a part of it. I hope more physicians engage both as detailers and as champions. I think it’s really important. Biography.
Johnathan Goree, MD, Director of Chronic Pain and Opioid Stewardship University of Arkansas for Medical Sciences Board certified in anesthesiology and pain medicine, Dr. Johnathan Goree received his Bachelor of Arts in biology from Washington University in St. Louis. He then moved to New York City where he completed both his medical degree and a residency in anesthesiology at the Weill College of Medicine at Cornell University. Following his time in Manhattan, he completed a fellowship in chronic pain medicine at Emory University Hospital in Atlanta, Georgia. In 2014, Dr. Goree returned home to Little Rock, Arkansas to join the faculty at University of Arkansas for Medical Sciences where he serves as the Director of the Chronic Pain Division and an Assistant Professor in the Department of Anesthesiology. He primarily focuses on the treatment of chronic pain conditions using opiate sparing, minimally invasive techniques. His specific research interests include complex regional pain syndrome, neuromodulation, and the effects of opioid education initiatives on patient outcomes. An Interview with Victoria Adewumi, MA, Community Liason, City of Manchester Health Department NaRCAD Training Alumna by Kayland Arrington, MPH, Program Manager at NaRCAD Tags: Detailing Visits, Opioid Safety, Program Management, Training  Victoria @NaRCAD2018's panel on AD for the opioid crisis. Victoria @NaRCAD2018's panel on AD for the opioid crisis. NaRCAD: How did you get into AD? How was the Manchester team formed? Victoria: I was very interested in community outreach and improving the health and well-being of families! I had cursory experience with substance use disorder management and had to jump in with both feet. It really helped having other detailers on the team that NaRCAD trained that I could lean on. The other detailers constantly provided support, and one helped open the door for me at her health system to speak with clinicians. She even provided me talking points that previously worked for her so I could walk into my first appointment feeling confident.  NaRCAD: What has your experience been as a detailer who does not have clinical experience but who does have public health expertise? Is someone able to be effective as an academic detailer without as much prior clinical training? Victoria: My experience has been extremely positive! I care about community, and I thought this was a great opportunity to gain new expertise in this field. I’ve always felt that a community perspective is needed for us to be able to leverage our impact in this field. The NaRCAD Academic Detailing techniques training was fantastic in helping me build tools to be able to speak well and motivate clinicians around medication-assisted treatment (MAT). My goal as an individual detailer is always to present myself as being on the same team as clinicians. I really see detailing as having a solution for clinicians, rather than simply trying to sell them an idea.  Manchester is located in Hillsborough County, NH Manchester is located in Hillsborough County, NH NaRCAD: Was there a time when a clinician presented pushback or obstacles that made it difficult to get your message across? Victoria: Some clinicians seemed to have already decided whether they were going to be on board or not before I even met with them. I had to feel strong and confident in the skills that I have. When I meet with a clinician, I always frame it as “I’m coming in as a representative of the community. There’s a crisis in our community, and you, as a provider, are a key part of the solution. How can we get you involved?” and “What kinds of things can you tell us that we haven’t even thought about before?” We need everyone’s participation if we’re going to change the tide of the city of Manchester, and clinicians are a vital part of that.
NaRCAD: You have mentioned the power of the team of detailers--can you tell us how the Manchester AD came to be so strong and effective? Victoria: I didn’t know any of the other detailers before the project. The NaRCAD training was great as an introduction to the work and to each other. We all had a sense of hope that was immediately apparent. We have the privilege of doing work that helps save lives and because of this attitude, there was a sense of camaraderie right away. We’ve been effective because our AD team is strong, and it was strong because we were intentional about building bonds. During the implementation period, we never went more than a month without checking in with each other, and sharing successes and challenges. I don’t think I would have enjoyed the process as much if I didn’t have this amazing AD team of colleagues. We’ve had incredible success in building a team of detailers who are all committed to and excited about the work of connecting with frontline clinicians to improve patient care around opioid safety.  NaRCAD: How would you recommend other programs go about recruiting those people that are equally committed and excited? Victoria: That’s a great question! I didn’t necessarily have an opioid response background, but I’ve always cared about communities. That desire to help others makes a great detailer. The trainings can teach the clinical content, but that element of wanting to improve people’s lives is the anchor of a strong AD team, and will resonate with the providers you’ll be detailing. I would then advise new sites to do the important work of helping their detailers to build strong relationships and a sense of teamwork right from the beginning. Those relationships will support everything, from good communication with clinicians, to a renewed sense of purpose in doing the work, which shields against burn out moving forward. Consistent opportunities to check in and connect between AD team members can’t be overemphasized—it truly made me feel that I was never in this alone; I was always working as part of something bigger than myself.  Biography Victoria Adewumi, MA Community Liaison City of Manchester Health Department Victoria Adewumi is a Community Liaison with the Manchester Public Health Department. Victoria primarily helps coordinate and staff programming of the Manchester Community School Project, a model that facilitates better health for Manchester residents through place-based interventions. Victoria serves Manchester residents by linking them to partners in the health, social service, business, non-profit, and faith communities and by engaging community members in resident leadership and equity activities. Victoria also participates in efforts to serve refugees and newcomers in New Hampshire through both direct service and community-building initiatives. Victoria holds Bachelor and Master of Arts Degrees in Political Science from the University of New Hampshire. Kayland Arrington, MPH, Program Manager at NaRCADTags: HIV/AIDS, Opioid Safety, LOOPR, Training This New Year, NaRCAD has new staff, new partnership sites, and will be addressing critical topics in health. We’ve had a successful 2018, and we’re already working hard to improve patient health through clinician education in 2019.  One of the main topics we provide support on is HIV prevention for high-risk patients. While it is true that rates of HIV are declining in some populations, other groups are still very much at risk for developing HIV. According to the Centers for Disease Control (CDC), half of all black men who have sex with men will contract HIV in their lifetime. These statistics are staggering, and NaRCAD is doing everything we can to help by engaging directly with frontline providers who can communicate best options for prevention directly to their patients. We do this by training academic detailers to meet with clinicians to offer tailored, evidence-based clinician recommendations.  Image Credit: AIDS Coalition of Nova Scotia Image Credit: AIDS Coalition of Nova Scotia In December, we traveled to Las Vegas to facilitate an AD training to increase prescriptions of Pre-exposure prophylaxis (PrEP). PrEP is a daily medication prescribed to people with a high risk of developing HIV. The CDC reports that PrEP reduces the risk of getting HIV from sex by more than 90%; it also reduces the risk of contracting HIV from injection drug use by more than 70%. NaRCAD is continuing our work in 2019 to train health educators to talk to frontline clinicians about the benefits of prescribing PrEP to their high-risk patients. Our first training of 2019 is in February at the PrEP Public Health Detailing Institute in San Francisco, hosted by our partners at the San Francisco Department of Public Health.  We’ve also added on 2 new sites to our county-level LOOPR Partnership! We will be traveling to St. Francois County, Missouri and Ware County, Georgia in March. The CDC has identified 220 counties (5% of counties in the nation) that are at highest risk of HIV and/or Hepatitis C as a result of the opioid crisis. St. Francois County, MO is ranked 69 out of those 220 counties. Ware County, GA is located in the southeast corner of the state and doesn’t have as much access to resources as counties more centrally located. NaRCAD is excited to join both of these high-burden counties in their efforts to reduce harm from the opioid crisis.  One element that is a common thread with both HIV and the opioid crisis is the fact that these are both highly stigmatized clinical topics. Along with community stigma, clinicians themselves may be inadvertently biased against patients with substance use disorder and/or those at high risk for developing HIV. As the result of a fear of stigma, it’s also common for patients to refrain from sharing high risk behavior with their providers. To ensure that front line clinicians increase PrEP prescribing and work to treat pain in safer ways, the academic detailers we train this year will also explore ways to address clinician stigma. Along with our county-level support, we’ll also travel to Tennessee, Oregon, and Maryland this year. And as always, we’ll hold our usual Boston home trainings in May, July, and September before our year comes full circle at our 7th Annual International Conference on Academic Detailing in November. No matter how we connect in the year ahead, our entire team is looking forward to supporting you in 2019—let us know how we can help, and stay tuned for more updates here on the DETAILS Blog.  Biography Kayland Arrington, MPH | Program Manager, NaRCAD Kayland earned her Master’s Degree in Public Health from Boston University, with concentrations in Health Policy and Law and Maternal and Child Health. She has experience coordinating suicide prevention and awareness programs. She also has experience in health promotion and education on topics ranging from substance use disorder to sexual violence. Kayland is passionate about improving access to resources, supporting population health programming, and is an advocate for evidence-based medicine. Read More. Exercising Empathy, Planting Seeds: An Interview with the Manchester, NH Academic Detailing Team10/26/2018 Featuring: Carol Furlong, LCMHC, MAC, MBA, Director of Substance Use Disorders, Elliot Hospital Jill MacGregor, APRN, Catholic Medical Center, & Katie Sawyer, LICSW, MLADC, Director, Integrated Treatment of Co-Occurring Disorders, Network4Health/Mental Health Center of Greater Manchester Interview by Isabel Evans, Fellow, NACCHO, in partnership with NaRCAD 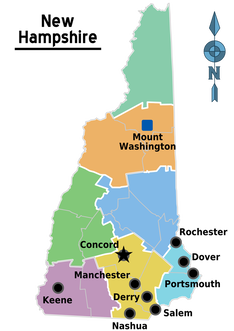 Tags: LOOPR, Opioid Safety, Stigma, Substance Use, Training EDITOR'S NOTE: Manchester, New Hampshire, was the third site of four selected for a 2018 pilot program of the CDC (Centers for Disease Control and Prevention), NACCHO (the National Association of County and City Health Officials), and NaRCAD (The National Resource Center for Academic Detailing). This exciting pilot program focused on community-level work with local public health departments to develop customized interventions to reduce opioid overdose and death. Four sites experiencing significant public health problems related to opioids were selected to be trained in academic detailing; those trained health professionals then conducted 1:1 field visits with front line clinicians to impact behavior around prescribing, treatment referrals, and patient care, with Manchester’s team focusing primarily on access to Medication Assisted Treatment [MAT]. As year 1 comes to a close, we’re showcasing successes from the field. Thanks for talking with us about your work in Manchester, New Hampshire. Can you tell us about your team? How were detailers chosen to represent the health department for this pilot project? Carol: Tim Soucy, from the Manchester Department of Health, contacted representatives at each of our organizations and gave a little bit of information about the training. He asked if our organizations had particular people that might be interested, and my supervisor thought of me, since I was in the middle of developing a MAT program for my organization. I jumped at the chance to participate. Jill: My organization received the same email, and as the primary care lead nurse practitioner, I was considered the most appropriate to participate. Katie: The invitation came from the site that received the CDC grant (City Health Department). The invitation was disseminated among a number of local human service/health agencies who are part of a Network of agencies as a result of our 1115 Waiver partnership.  The NaRCAD team came to your site back in March, 2018, helping you get ready to be ‘in the field’ and talk to clinicians about the opioid crisis. Tell us how that went, and how you applied what you learned in training. Carol: I’m a naturally shy person who dislikes being the center of attention, so I was incredibly nervous about the role plays during training. The turned out to be invaluable, since I use the skills I developed through practicing and receiving feedback during every visit. The role plays prepared me so well for meeting with providers, and I go into the conversations feeling confident and comfortable. When they ask questions, I feel that I know how to answer, or where to turn for more information, such as the wonderful handouts available on the NaRCAD website. Jill: For me, learning how to hold a discussion as a detailer was the most important element of the training. I learned how to frame a conversation using open-ended questions, which allows the discussion to progress. Understanding how to simultaneously get a provider’s perspective, while also giving them the information they need, is a critical detailing skill. Katie: We were able to role play, which has proven very helpful out in the field to stay focused, on topic, and empathetic to the position of each clinician that I speak to. The handouts that NaRCAD provided have easy to read information and great graphics, so they have also proved useful for staying on track with the key messages during detailing visits, along with providing supplemental information. 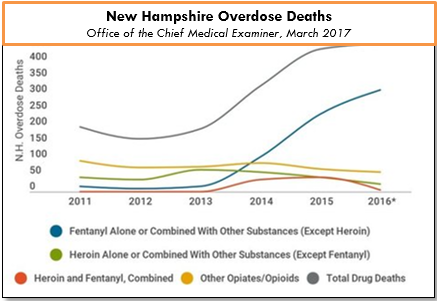 The opioid epidemic has affected many communities in unique ways. How have local clinicians responded to your visits? What do clinicians in Manchester see as major barriers to improving health for their patients struggling with this issue? Carol: Clinicians can be a little skeptical at first, since they’re often expecting that I’m going to try to “sell them” on something. When I focus on listening to their experiences and their concerns, I’m able to gently address those concerns and give resources or suggestions. Even just having a discussion can help clinicians to feel that you’re interested in how they feel, and that you genuinely want to help them – I would describe some clinicians as “dumbstruck” from our conversations, because they’re preparing to do battle with me, but they instead come to see me as a resource, and are more willing to meeting with me. As for challenges, we deal with a fair amount of stigmatization of substance use. It’s a major barrier, and we’ve had to spend a lot of time addressing that in my organization. Another barrier for clinicians is a preconceived notion that providing MAT is an onerous process, and too time-consuming to add into their schedules. And these two barriers really complement each other in a bad way – I often get providers saying that MAT is too much work and that their MAT patients will just end up using opioids again and ending up back in the emergency room. Breaking down these misconceptions about MAT and getting to the root of the stigma against MAT is a big challenge. However, we’re approaching these challenges with education and lots of conversations, since we’ve found that helping our staff to get a better sense of addiction as a disease is really invaluable to making them more open to MAT and treating people with opioid use disorder. The timing of the academic detailing initiative couldn’t have been better for my organization, because having conversations about addiction leads well into having conversations about MAT, and vice versa. Engaging in academic detailing has opened up a whole new avenue of clinician education for me. Jill: Because of my role at my health system, I talk to providers about many different topics and they’re used to me approaching them, which has definitely helped give me and automatic “in” and bring up sensitive topics. My institutional knowledge helps too, since I can answer questions specific to my organization and our various programs or resources around opioids.  A major challenge I face is that providers don’t think they have the time and resources to implement MAT into primary care, and they don’t feel they have the behavioral health support to do so successfully. However, I’ve found that this is often based around a lack of knowledge, since when I ask more probing questions about MAT, it’s often clear that they don’t really know much about it! Providers will come to conclusions without getting the right education, and I find that they often “change their tune” when I give them more information. Providers are also hesitant about writing a prescription for a MAT patient if there isn’t someone in their office who can talk to the patient about addiction itself. Right now, we’re working on integrating behavioral health clinicians into primary care, which I’m hopeful will help with this very real concern. Katie: There has been some hesitation in sharing with detailers, in regards to professional experience, as I believe most clinicians are on edge in trying to do the best that they can to address patient needs, while also supporting alternatives to typical or historical use of prescribed opioids. With an empathetic and interested stance, I’ve found that most clinicians are open with their experience and struggles. There are a number of themes among clinicians for challenges that I’ve noticed, including a limited behavioral health workforce to support what they view as an ideal MAT protocol, which would include individual and group counseling, regular urine toxicology screens, and wraparound services along the continuum of care. In addition, there is a concern among providers about the potential diversion of Buprenorphine by patients.
Katie: It has been rewarding to meet with each clinician for different reasons – I would view success as learning more about the clinicians that are already on board and excited to pursue getting a waiver, as it gets them talking and feeling a renewed energy to share with others. I view my conversations with clinicians who are not interested in pursuing a waiver as equally rewarding, since it allows for both of us to share and hear the other’s perspective. We can agree that the work is needed and challenging, no matter how we decide to go about addressing the needs of our patients. Lastly, what advice would you tell new detailers? What do you wish you knew when you started out? Carol: I would tell new detailers to take a deep breath and know that you’re ready for this – NaRCAD does such a good job of training us as detailers, and you just feel ready. Jill: I would say to recognize that everyone has a natural process for adapting to new ideas. You’ll get some providers who are ready and energized, some who will want to watch others in action before they jump in, and some who simply may not be interested. It can be frustrating when providers aren’t interested in your topic or resources, but understand that this is natural, and don’t take it personally! Every visit will be different, and that’s okay. Katie: My advice is to remember that success is not defined as “convincing” someone that the topic of your detailing visit is “the right answer”. In fact, trying to convince another person of anything is essentially walking against waves. Instead, be open to listening to that person and their experiences, and then value the experience that they have had. This is more likely to open the conversation to allow you to share your wealth of information and experiences. It’s all about planting seeds. Ideas? Comments? Questions? Sound off on this blog in the comments section below!
 Guest Blogger: Joseph Leishman Academic Detailer/Masters in Public Health Candidate Center for Clinical Management Research, Ann Arbor VA The University of Michigan School of Public Health NaRCAD Training Alumnus Tags: Cancer, Detailing Visits, Materials Development, Training  NaRCAD: How did you get into AD? What were you doing before? Joe: I’m a graduate student at The University of Michigan School of Public Health studying epidemiology. As a student I started working at the Ann Arbor VA Center for Clinical Management Research on a lung cancer-screening project. Our project involves 8 different VA sites across the country. As we shifted into an implementation phase, academic detailing was selected as an implementation method. I transitioned to an academic detailer role because of my background in epidemiology, my understanding of lung cancer screening (LCS), and my ability to communicate these principles. I attended the NaRCAD academic detailing techniques training and things took off from there! 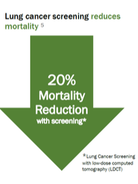 NaRCAD: Why is AD for lung cancer screening so important? Joe: Lung cancer screening can be more complex and complicated compared to other preventative services, and most primary care physicians have very limited time to discuss lung cancer screening with patients. There are a number of potential downsides to screening – false positives, overdiagnosis, invasive procedures, and complications from invasive procedures. The benefits of the screening outweigh the challenges, and we have developed a tool for doctors to quickly evaluate a patient’s lung cancer risk, facilitate shared decision making, and make personalized screening recommendations. NaRCAD: Tell us about the lung cancer screening detailing aid and related tools that you made with NaRCAD’s support. How was the process of developing the detailing aid? Joe: Our detailing aid contains background information on lung cancer screening and some of the key evidence behind our tool. It also outlines some of the reasons and benefits behind using this risk-based approach. We tried to keep the detailing aid simple enough that doctors could quickly understand the concepts with little or no additional explanation. This was our group’s first attempt at making something like this. We worked with NaRCAD during the creation of the detailing aid to improve the clinical content, layout, and language. There was a lot of trial and error to create the detailing aid. We ended up going through 10 versions before it was finalized.  NaRCAD: How did you decide what information was most important to put on your detailing aid? Joe: Initially, we started out with too much information. It was too complicated and wordy to effectively communicate our message. We tested it out with our team to see if our message was clear. It was obvious when sections of detailing aid didn’t work well. We really had to focus on narrowing down the main evidence and messages we wished to convey. We used the primary lung cancer screening evidence from the US Preventative Task Force and the National Lung Screening Trial. Our tool goes a step beyond screening eligibility to look at individual risk, life expectancy, and patient preferences, which help providers get past some of the difficulties and complexities of lung cancer screening.  NaRCAD: How does your website complement the detailing aid when you are 1:1 detailing? Joe: A link to the tool is embedded in the Computerized Patient Record System (CPRS), the EMR system that the VA uses. However, it can be also accessed outside the VA with a URL. What I typically do is I have PCPs pull up the website in their workspace after going through the detailing aid. I have providers role play with a sample patient, and I demonstrate how the tool could be used for that specific patient. Using the actual web tool in a detailing meeting really helps to reinforce our message. We feel like it increases the likelihood that it’ll be adopted in an actual clinical practice. NaRCAD: How have clinicians been responding to your campaign? Joe: So far there has been a decent response from the doctors we have worked with. Some of the doctors in the VA have met with detailers before which makes the initial contact easy. However, the most majority of the doctors I have met were receptive to my visits. We’ve been tracking the use of our tool before and after academic detailing at a site level. We don’t have exact numbers, but there has been an increase between before and after AD. We’d be happy to share more complete data in a future blog post.  NaRCAD: That'd be terrific, we'd love to share that when it's ready! What other reflections do you have from this process that you'd like to share with our community? Joe: Academic detailing is a new approach for our group. It has been a real learning experience for discovering what does and doesn’t work and how to best address provider needs. For me, going through this process has been a lot of fun. I love talking with doctors about their struggles and being able to offer a tool that can help them better handle lung cancer screening with their patients. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|