|
Curated by: Aanchal Gupta, Program Coordinator, NaRCAD Tags: ADvice, Harm Reduction Harm reduction has gained significant traction, especially as an area of focus in AD, with campaigns encouraging clinicians to provide preventive care, discuss harm reduction services with their patients, and connect their patients to related community initiatives. In this edition of AD-vice, we explore the evidence supporting harm reduction strategies, the broader approach that shifts the narrative from stigmatization to inclusivity, and the crucial role of clinician-patient communication.  EVIDENCE & IMPACT OF HARM REDUCTION STRATEGIES
 HARM REDUCTION APPROACH
 CLINICIAN-PATIENT SUPPORT & COMMUNICATION
We hope these insights inspire you to consider harm reduction approaches in your detailing work. If you’re interested in learning more, join us at our 2nd annual AD Virtual Summit where we will dive into these areas further!
Best, The NaRCAD Team By Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD An interview with Adriane Apicelli, MSW, Project Manager, Harm Reduction Projects, University of New Hampshire, College of Health and Human Services. Tags: Harm Reduction, Detailing Visits, Evidence-Based Medicine  Anna: Hi, Adriane. Harm reduction is deeply meaningful to many individuals – can you share why harm reduction is meaningful to you? Adriane: The core principles of harm reduction, such as self-determination, mutualism, and self-advocacy, resonate with my personal and professional values. I firmly believe that individuals are the experts in their own lives, and it’s essential that people have access to the necessary resources, materials, and support systems to ensure their safety and well-being. Harm reduction also offers a powerful framework that facilitates a shift within communities that moves away from moralization and stigmatization of individuals who use drugs. It’s easy to blame individuals for their behavior, but it’s far more challenging to critically reflect on how systems and decisions put people in those circumstances in the first place. Anna: By embracing harm reduction principles, people within our communities can foster empathy and understanding for those facing challenges with substance use. Everyone deserves the same dignity, respect, and access to necessary resources. Can you tell me about the harm reduction detailing project you’ve been working on in collaboration with the National Association of County and City Health Officials (NACCHO)? Adriane: We’re currently focused on detailing elected officials in the State of New Hampshire, including city counselors, mayors, and senators. The opinions and decisions of elected officials shape the harm reduction service landscape – they make decisions that either enable or constrain available resources. Anna: Recognizing the influential role of elected officials is crucial when working on public health initiatives, including harm reduction. What is the overall goal of your current detailing project?  Adriane: We want to empower elected officials to make informed decisions that increase capacity of harm reduction services based on the needs of their communities. We’re currently encouraging elected officials to establish direct connections with individuals who use drugs so they can integrate the expertise from those with lived and living experience into decision-making processes regarding laws, policies, and resource allocation. Anna: Actively listening to those with lived and living experience helps to better understand how to support specific populations. How did your team decide to focus on encouraging elected officials to directly connect with people who use drugs? Adriane: During the development of our detailing project, we consulted with local syringe service program (SSP) participants and asked them how they think elected officials can better understand substance use and harm reduction. The overwhelming response was for direct communication between individuals who use drugs and elected officials, or having elected officials spend the day with them to understand their experiences firsthand. We’re trying to figure out how we can facilitate these approaches to ensure the safety and ethical treatment of SSP participants. We’ve also been exploring the possibility of forming advisory committees to incorporate the perspectives of individuals who use drugs in the decision-making process in a safe and supportive environment.  Anna: Advisory committees certainly help to ensure that voices and perspectives are heard and valued. Let’s transition to thinking about all of your detailing work to date – what makes you most proud to be a harm reduction detailer? Adriane: The people I detail. We shouldn’t underestimate how hard it is to change our minds, our attitudes, or our behaviors. It takes so much humility and effort to receive and integrate new information, especially when it counters your social values and beliefs. It’s an honor to work through that learning process with those that I detail. Anna: Do you have a specific example of that learning process that you can share? Adriane: I detailed someone who was initially hesitant to publicly announce that she prescribes buprenorphine because she was worried how that information would affect her patient panel. We ended up having a conversation about substance use stigma and its implications. We discussed that openly sharing that she prescribes buprenorphine serves as a powerful signal to patients, assuring them that she provides a safe environment to seek treatment. It also sends a message to other clinicians about the importance of prescribing this medication to patients who need it.  Anna: Having those types of honest conversations with people you detail is imperative to changing behaviors and reducing stigma at the individual and community level. Is there anything else you’d like to add before we wrap up today? Adriane: Remember that it’s much easier to build harm reduction capacity in collaboration with others. Last year, I collaborated with individuals from the public health department, a local hospital, the New Hampshire Harm Reduction Coalition (NHHRC), and a community volunteer to address a concern raised by a business owner regarding improperly discarded sharps on their property. We formed an informal work group and created a proposal aimed at piloting an anonymous syringe disposal project, installing two disposal units in the community. The disposal units were proposed to be on city property, so we needed buy-in from City Council to be able to do this. We recognized the power of engaging elected officials and presented our proposal to the City Council. Our proposal received unanimous support and it’s currently being piloted in the community. Collaborative advocacy and engagement with members of the community and elected officials can bring about positive change and enhance the health of all. Anna: We often have more power than we think when we collaborate with others who have similar goals. Detailing is an effective approach for encouraging collaboration and connection with experts in the community, including experts with lived and living experience. Thanks for joining us today, Adriane! We look forward to continuing to hear about your inspiring harm reduction work in New Hampshire. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Since 2020, Adriane Apicelli has served as the Project Manager and primary academic detailer of the University of New Hampshire (UNH), Department of Nursing’s Harm Reduction Education and Technical Assistance (HRETA) project. She holds a Master of Social Work (MSW) from Boston College, where she also earned a Certificate in Management. In addition to her role with the HRETA project, Adriane serves as a nonprofit strategic planning consultant and has previously served as an adjunct professor for the Department of Social Work at UNH. Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Opioid Safety, Harm Reduction  The NaRCAD team is back on the road! We had the privilege of attending the 2023 Rx and Illicit Drug Summit in Atlanta, Georgia, where we joined a diverse learning community of over 3,000 participants. We heard about best practices in prevention, treatment, and recovery for those affected by the opioid epidemic and engaged with experts from various fields who have developed innovative strategies to combat the crisis. We attended presentations, poster sessions, and booths from a wide range of professionals, including clinicians, law enforcement personnel, public health officials, lawmakers, attorneys, families, and individuals in recovery. It’s clear that we need to continue to work together across disciplines to reduce opioid use disorder and opioid overdoses within our communities.  While we were in Atlanta, we saw folks from our AD community who are working on opioid-specific academic detailing projects, including our colleagues at Alosa Health! If we didn’t catch you while we were there, please reach out to us at [email protected] and tell us about your experience in Atlanta! NaRCAD also had the opportunity to present with our colleagues from Comagine Health to share about our own collaborations and findings from a recent project, a 15-month clinic-based intervention called Improving Pain and Opioid Management in Primary Care (PINPOINT). The PINPOINT intervention was implemented in 36 clinics in Oregon and combined the Six Building Blocks, academic detailing, and practice facilitation approaches to improve pain management, opioid prescribing practices, and treatment of opioid use disorder in primary care settings.  A baseline survey of clinical staff and prescribers was conducted to assess knowledge, attitudes, and behaviors regarding opioids. The survey results suggested differences between clinical staff and prescribers in behaviors and attitudes about opioid therapy for treatment of chronic pain, familiarity with opioid prescribing best practices, and opioid-related policies and procedures. The participants who attended the conference session were eager to learn about how they could implement academic detailing programs in their own communities. We’re excited to share about the importance of academic detailing at future conferences and continue to learn and grow alongside all of you. Interested in submitting a proposal with the NaRCAD team at a future conference? Email us at [email protected]! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation! By Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD An interview with Lindsey C. Beardsley, Individual in Recovery. This month, we’re looking through the lens of the patient experience, something that all detailers and clinicians work so hard to improve. We’re pivoting to an interview with a person with use disorder, her experience with use and recovery, and the ways in which the patient experience can encourage detailers and clinicians to continue working together to improve outcomes for those who struggle with substance use. Tags: Harm Reduction, Opioid Safety  Anna: Hi, Lindsey! We’ve never featured a patient’s experience on our DETAILS blog - thank you for sharing space with me and telling a vulnerable story. Let’s dive right in. Can you tell me about your background? When were you first introduced to substances? Lindsey: I was brought up in Cape Cod, Massachusetts with two loving parents and a lot of friends. I had a typical childhood, but I always knew I was different. I was extremely impulsive. I loved food – that was my first addiction. Then it was dance, then soccer, then horses. I did everything to excess. I was first prescribed opioids after a knee surgery at 13 years old, and again after a second knee surgery at 14. Something clicked in my brain when I used those medications, and it opened a door that I couldn’t close. I was shut off to all emotion and it felt good to not feel anything. My use progressed from taking prescribed medications for pain to using heroin and becoming homeless, struggling to meet my most basic needs. Using drugs gave me a false sense of power that I wasn’t like any of my peers and that I could do what I wanted because I was different.  Anna: We hear many stories from patients about substance use starting after pain medications are prescribed during adolescence. Despite the power that you felt when you used, were you ever worried about the health effects of your drug use? Lindsey: I dated someone in my teenage years, and we often used together. Cape Cod is a small community and within a few weeks of dating him, my mom heard that he had Hepatitis C. My entire family was devastated, but I didn’t care at all – I couldn’t see how it would affect me. I think back to all the times I shared needles and drug supplies. Even if I tried to use new needles, everything looked the same and would get mixed up in the rush of using with other people. I would always have a little fear inside of me that I would overdose on my first time using again after being in treatment, but that fear never stopped me.  Anna: We know that substance use disorder is a medical condition and patients need professional support. When you felt ready to address that fear and seek treatment, were there healthcare resources or community supports that helped guide you towards recovery? Lindsey: I’m lucky to be in a state like Massachusetts where we have a lot of resources that the rest of the country doesn’t have. I was a frequent flyer at our detox facilities. When I was admitted, I was always paired with a peer that was in recovery. I often knew the peer; it gave me hope to hear the stories of recovery from people I knew and previously used drugs with. I was assigned a counselor, and we would discuss my treatment goals and next steps. The counselor would walk through every community resource within several miles of me, like partial hospitalization programs, sober homes, Narcotics Anonymous (NA) meetings, 12-step programs, and syringe exchange programs. We also have a mobile harm reduction center in my community. Before it existed, a woman in recovery started a needle exchange program out of her home. She sparked a need and desire for our community to learn more about harm reduction.  Anna: Many people don’t have access to substance use resources in their community, especially harm reduction services. Here at NaRCAD, we’re trying to encourage primary care clinicians to be able to provide those linkages to care and harm reduction services. What does harm reduction mean to you? Lindsey: I was against harm reduction for a long time because I was very involved in a 12-step fellowship where the primary purpose was complete abstinence from drugs. Harm reduction was a shift in mindset for me, but it’s pretty cut and dried. We’re reducing harm, saving lives, and preserving a sense of family and community. When we reduce harm, we allow a mom to be a part of her family again, we allow her to get a job, we allow her to get off the street and out of harm’s way. Harm reduction can allow people to return home. Anna: It’s valuable to know that a 12-step program and harm reduction can co-exist. What message about harm reduction would you want to share with members of your community? Lindsey: Harm reduction doesn’t enable drug use – use is going to continue until the person is ready to seek treatment. A simple approach to harm reduction, like syringe exchange, prevents the spread of infectious diseases and reduces needles in public and community spaces. It prevents someone from contracting Hepatitis C when they use drugs. Anna: We know that harm reduction plays a huge role in preventing drug-related deaths and offering access to services. There are many approaches to harm reduction and even using just one approach reduces so much harm. Let’s transition to talking about patient care. How would you want your care to look, or not look, when seeking help for substance use from a clinician?  Lindsey: I’d want to seek care in a safe space where I could share what drugs I use and how I use them without being punished, judged, or arrested. I would also want a space to discuss what’s going on in my life with someone who is educated enough to help me. I honestly wouldn’t want to listen to a clinician tell me about treatment options while I can sense that they’re judging me. A lot of clinicians have been through at least one training on substance use, but those trainings don’t change core beliefs and morals. Those trainings don’t change the way a clinician looks at you when you tell them you use substances. Anna: That’s true – having a trusting relationship with a clinician where you can share openly and not be judged is critical to effective care. How could clinicians have meaningful conversations with patients about substance use, especially if they have preconceived notions? Lindsey: Clinicians need to learn to have open, non-judgmental, inclusive discussions. That starts with asking all patients about their mental health and substance use history. Educators can provide clinicians with scripting tools if they feel uncomfortable having these conversations. Also, including peer support in the plan of care can help take some of the stress off of the clinician. This can include reviewing community resources and continuing the conversation with patients, while also educating the clinician on substance use through sharing personal experiences. We need to support patients, peers, and clinicians in doing this work and doing it as a team. Anna: I’m hearing you talk about so many elements that clinicians can use to improve patient care, like scripting tools and peer support. We’re continuing to work on ways to support educators and clinicians – your ideas will certainly help guide us. Thank you again for sharing your insights and being open to this conversation. We look forward to connecting with you again in the future! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Lindsey C. Beardsley, an individual in long-term recovery, was born and raised in Cape Cod, Massachusetts. She was involved in many different sports growing up – gymnastics, soccer, and dance – but riding and working with horses quickly won over her time and heart from a young age. After many years of struggling with addiction, Lindsey walked into a treatment facility in August of 2018 and made the decision to stop using drugs one day at a time. Lindsey has been in recovery since September 21, 2018. By Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD An interview with Meghan Breckling, PharmD, BCACP, Ambulatory Care Pharmacist and Academic Detailer, University of Arkansas for Medical Sciences and Arkansas Department of Health. Tags: Detailing Visits, Opioid Safety, Harm Reduction, Evidence-Based Medicine 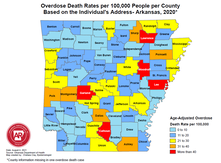 Overdose Deaths Rates per 100,000 people per County, Arkansas 2020 Overdose Deaths Rates per 100,000 people per County, Arkansas 2020 Anna: Hi, Meghan. Thanks for joining me on DETAILS today! Your team has done extensive work on pain management detailing, and you recently completed a pilot project on harm reduction in collaboration with the National Association of County and City Health Officials (NACCHO). Can you tell me a little more about this project? Meghan: Thanks for having me! We decided to target rural counties in Arkansas that have both high drug overdose deaths and naloxone administration rates. We previously created broad pain management materials for our other opioid safety detailing projects; this project took those materials to the next level. We looked at how we could better support clinicians in caring for their patients with substance use disorder (SUD) through a harm reduction lens. We provided clinicians with screening tools to help identify patients with mental health conditions and SUD to determine who could benefit from additional services. We even created a local resource guide for clinicians to easily connect patients to community services. The clinicians found that these accessible tools helped them have open conversations with patients.  Anna: I can imagine having something tangible to give to patients makes clinicians feel more equipped to have these conversations. What other resources were you able to share with clinicians? Meghan: We encouraged clinicians to utilize a new, free mental health resource called AR ConnectNow. This program provides immediate virtual care to all Arkansans dealing with mental health and substance use disorders. Clinicians were grateful for AR ConnectNow because mental health services are scarce in rural Arkansas; they’ve been sharing it with their patients frequently. Anna: You must have been proud to be part of a project that had such an impact on both patients and clinicians. How did the harm reduction lens inform your detailing visits for this project compared to your prior pain management-focused visits? Meghan: Many visits centered on communication with patients. Communication and empathy are two huge pieces to consider with this topic. We spent a lot of time asking clinicians about the conversations they have with patients and the types of questions they ask about substance use. We really wanted to understand what was going well and where there were gaps that we could help fill with resources and support. We also focused on naloxone prescribing and administration. We gave out free naloxone kits to all clinicians that they could either keep in the clinic or give to a patient who was having trouble accessing it. Clinicians were open to the idea of prescribing naloxone to patients who were at risk of overdose and open to keeping kits in their clinic in the event of an overdose. Our team had a lot of clinicians say during follow up visits that they felt more comfortable prescribing naloxone and were prescribing it more to patients and family members.  Anna: It’s impressive how you were able to clearly shift your focus from opioid prescribing to harm reduction and prioritize the relationship between the clinician and patient. Did you receive any pushback from clinicians on harm reduction? Meghan: Clinicians understood the need for harm reduction services but were more inclined to refer patients out rather than providing services within their clinics. For example, we found that a lot of clinicians were resistant to prescribing Medications for Opioid Use Disorder (MOUD), either because they were uncomfortable with the steps to do so, or they were told by leadership that they should not prescribe MOUD at their practice. It can sometimes take an hour or more for patients in rural areas to access specialty services that offer MOUD. We’re looking at future projects where we can utilize pharmacists to increase MOUD prescribing in partnership with primary care providers. For instance, a primary care clinician could diagnose SUD and prescribe MOUD, while a pharmacist could monitor the patient throughout treatment. It would take a lot of burden off the clinicians and could possibly make them less resistant to prescribing it.  Anna: Using pharmacists as an integral part of the care team is an excellent idea – you’ll have to let us know if you receive additional funding for this work! Let’s wrap up with a final question. If another program decided to do a detailing project on harm reduction, what advice would you give them before they went out into the field? Meghan: You need to take a step back and remember that there isn’t going to be instant behavior change among clinicians. For a topic this complex, it’s critical to have follow-up visits and continue to be a resource and support for clinicians. Also, be understanding of clinicians and their experiences. They’re dealing with a lot and it’s not easy to change things all at once. Building a relationship and getting a clinician to commit to just one key message is a huge win. Want to learn more? Read about the harm reduction key messages used for this project and the development of those messages on our previous blog post. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Dr. Meghan Breckling is an Ambulatory Care Pharmacy Specialist at the University of Arkansas for Medical Sciences (UAMS) and is a trained Academic Detailer through the National Resource Center for Academic Detailing (NARCAD) within the Center for Health Services Research (CHSR) at UAMS’ Psychiatric Research Institute (PRI). She previously completed a PGY1 Pharmacy Residency and PGY2 Ambulatory Care Residency at the Central Arkansas Veterans Healthcare System (CAVHS). Currently, she is a part of a multidisciplinary academic detailing team comprised of a pharmacist, physician and physical therapist that provide evidence-based solutions, tools and support for chronic pain management to primary care providers across the state of Arkansas. By Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD An interview with Shuchin Shukla, MD, MPH, Faculty Physician, Mountain Area Health Education Center (MAHEC), NaRCAD Training Facilitator Tags: Harm Reduction, Detailing Visits, Evidence-Based Medicine, Opioid Safety  Anna: Welcome to the DETAILS blog, Shuchin! You wear many hats - you’re an addiction medicine physician, an academic detailer, and an academic detailing trainer. Tell us how you got started with academic detailing. Shuchin: I had an interest in marginalized populations and did my residency in the Bronx in New York City. I was a clinician in HIV care for several years before moving with my family to Western North Carolina. Soon after we moved, I began working at our Area Health Education Center (AHEC) and it was evident that addiction was the primary public health and clinical issue that was causing the most harm in my community. Fast forward a few years and one of my colleagues received a Centers for Disease Control and Prevention (CDC) grant and asked if I could attend a NaRCAD training to learn more about AD. The medical board and one of our pharmacists at the Department of Public Health were very interested in using AD for overdose prevention. We started with a pilot where we detailed 10 clinicians and slowly built our program. We now have multiple AD grants we’re working on, including one on adverse childhood experiences (ACEs) and one on harm reduction.  Anna: We often tell programs to start with a small pilot before growing their programs so that they can identify what went well and where there are opportunities for improvement, especially on new detailing topics like ACEs (e.g., key message adoption, clinician response, etc.). You do a lot of education around substance use disorder and mentioned that your team received a harm reduction grant for AD – what does harm reduction mean to you? Shuchin: The goal is, simply enough, to reduce the level of harm that a person may be facing. Harm reduction means having no expectation of a person's behavior and accepting the reality of what people live and do without judgement. It’s about being open with patients so that they’re more likely to come back for a visit where you can continue to have a conversation with them about getting a little bit healthier. There’s evidence to support harm reduction. The research shows that providing harm reduction services, whether it's naloxone or syringe exchange, reduces harm, but also decreases substance use and helps people engage in substance use care and treatment. Anna: Do you see harm reduction being used with other topics beyond substance use disorder?  Shuchin: There are tons of examples of harm reduction that are built into everything we do. Seatbelts, masks, fire escapes, smoke detectors, vaccines, and the FDA regulatory agency are all forms of harm reduction. As a society, we’ve never looked at substance use through this lens because using drugs is so stigmatized. Anna: I imagine it’s difficult to have detailing visits with clinicians because of the type of stigma associated with it, such as thinking that it’s some sort of moral failing. How have clinicians responded to detailing visits on harm reduction? Shuchin: Most of the teaching about harm reduction is unlearning all the inaccurate information we've been taught. We're taught if you use drugs, you're a bad person and you should be penalized. I remember watching the show Cops growing up and there was always a person of color laid out on a car resisting arrest. Law enforcement would pull out a bag of cocaine from the car and say they’ve saved the community. None of this is right, but I saw that on TV as a middle school kid. It’s easy to generate a lot of negative energy about substance use disorder and substances in general from these shows, and clinicians are part of that thinking too. Asking clinicians to talk to their patients about harm reduction is a lot different than asking them to check their Prescription Drug Monitoring Programs (PDMPs) to ensure that patients aren’t receiving multiple prescriptions for controlled substances. Having a conversation with a patient takes empathy and thoughtfulness, whereas checking a PDMP does not. We’ve found that clinicians who have been the most resistant to harm reduction are those who have family members with substance use disorders. They are often angry, and rightfully so.  Anna: It’s imperative to be empathetic during detailing visits, especially on a topic that affects so many people. Let’s explore harm reduction from a different angle. How do your patients respond when you bring up harm reduction during your clinic visits? Shuchin: These are certainly challenging conversations to have, so you need to start off by letting patients know that they aren’t going to get in trouble for sharing this information and you need to acknowledge the trauma and stigma that surrounds substance use. Patients seem grateful that I approach conversations in a straightforward way that doesn’t stigmatize their use of drugs. I’ve never had a patient be offended or confused about why I was talking to them about harm reduction. Their eyes usually widen when I ask them things like how they use their drugs, how they cook their drugs, or where they get their drugs from. They often say, “I’ve never had a doctor like you.” Anna: You must spend a lot of time building trusting relationships with patients so that you can have these conversations. Shuchin: I do. It also helps that the organization I work for, our county commissioners, and our sheriff are all on board with harm reduction. There’s a lot of focus on Naloxone distribution among members of our community, such as law enforcement, first responders, and other clinicians. Our clinic prescribes a lot of medications for opioid use disorder, specifically buprenorphine, which is also a form of harm reduction. We have peer support specialists who meet patients where they’re at and start the conversation about harm reduction with them before they even have their first visit with me.  Anna: It’s definitely critical to have a community that supports the way you practice, as well your program’s AD messaging. Can you share a final tip for other detailers who are working on harm reduction? Shuchin: Harm reduction is an emotional topic for a lot of people, especially folks who are in frequent contact with people who use drugs, like emergency room clinicians or people with lived experience in their families. With this topic, paying attention to the emotions of the clinician you're detailing and acknowledging those emotions before jumping into your key messages is much more important than any other topic I’ve worked on. Be patient and empathetic – every visit counts toward making a change. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Shuchin Shukla, MD, MPH, was born and raised in New Orleans, Louisiana. He completed medical school and public health school at Tulane University and completed a residency in family medicine at Montefiore Medical Center in the Bronx, New York. He worked in the South Bronx for 5 years following residency, providing primary care for adults and children, as well as for adults living with HIV. He also served as medical director for Montefiore Project INSPIRE, a primary care-based Hepatitis C treatment program. He then moved with his family to Asheville, North Carolina, where he currently serves at Mountain Area Health Education Center (MAHEC) as faculty physician and Clinical Director of Health Integration. He is an associate clinical professor of medicine in the Department of Family Medicine at the School of Medicine, University of North Carolina in Chapel Hill, and is a Diplomate of the American Board of Preventive Medicine, Board-Certified in Addiction Medicine. Additionally, he is a Robert Wood Johnson Clinical Scholar. He leads on various initiatives and projects around addiction, HIV, Hepatitis C, homelessness, and the criminal justice system. His main experience as a detailer has been focused on improving evidence-based provider interventions related to opioids, pain, and addiction. Honest Conversations: Supporting Clinicians in Linking Patients to Harm Reduction Services11/14/2022
By Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Primary Care, Opioid Safety, Evidence Based Medicine, Harm Reduction  Our team at NaRCAD has been working on an exciting new project developing harm reduction key messages for primary care clinicians in collaboration with the National Association of County and City Health Officials (NACCHO), Centers for Disease Control and Prevention (CDC), and consultants from Boston Medical Center. The Substance Abuse and Mental Health Services Administration (SAMHSA) defines harm reduction as an approach that aims to prevent overdose and infectious disease transmission, improve physical and mental health, and offer options for accessing treatment and other health care services for people who use drugs. Various harm reduction approaches have been proven to prevent overdose and death, injury, infectious disease transmission, and substance misuse. For instance, there is nearly 30 years of research that has shown that syringe services programs decrease transmission of viral hepatitis, HIV, and other infections. There are several other harm reduction approaches beyond syringe service programs, including:
It’s critical that academic detailers continue to encourage primary care clinicians to discuss harm reduction with their patients and link them to services within their community. Academic detailers have the ability to empower clinicians to have difficult conversations with patients to reduce infections, overdose, and death. Our team developed the following key messages to support primary care clinicians in caring for patients who would benefit from harm reduction. These key messages are currently being piloted across the United States in a project funded by NACCHO.  Harm Reduction: Key Messages to Improve Outcomes for People Who Use Drugs 1. Assess factors that may contribute to risk of Opioid Use Disorder (OUD) for patients who use opioids. 2. Identify opportunities to reduce risk of harm using a patient-centered approach. 3. Offer Medications for Opioid Use Disorder (MOUD) to patients identified as having OUD. 4. Connect patients with community harm reduction services and other services that meet identified needs. These evidence-based key messages can help clinicians provide support to their patients and build strong and trusting relationships with those who need it most. Building trust between clinicians and patients allows patients to feel heard and be open to seeking additional treatment, ultimately leading to improved health outcomes. Our team is looking forward to continuing to explore harm reduction and updating our key messages based on the results of the pilot through NACCHO. If your program is interested in collaborating with our team on future harm reduction work, or any other clinical topic, please reach out to us at [email protected]. Want to learn more? Stay tuned to learn about the results of the pilot and how clinicians responded to these key messages in the field. You can also join our discussion forum to interact with peers who are working on harm reduction! |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|
