 Words of AD Wisdom is a series that features tried-and-true practices from AD experts. Our guest blogger this week is Chirag Rathod, PharmD, a NaRCAD Facilitator and Academic Detailer at Illinois ADVANCE. Tags: Detailing Visits, Evidence Based Medicine, Materials  Simplify your messaging! Prior to your detailing visit, think about ways to slow down and limit the amount of information you share with the clinician so that the visit is of most value to them. You can do this by asking focused needs assessment questions and providing the clinician ample opportunities to speak and engage in the conversation.  Focus. Focus. Focus. Resist the urge to cover too much content in your detailing aid during an AD visit. A more focused discussion on one section of your brochure can be more fruitful than trying to cover every key message during a single visit.  Open-ended questions will set you free! There is limited usefulness in asking closed-ended questions (e.g., confirming something about the clinician’s practice). The use of open-ended questions can help you gain layered insight into the clinician’s practice and tailor the visit to them. Asking open-ended questions allows opportunities for the clinician to speak about their experiences in detail and for you to listen and deliver supportive, relevant key messages.  Prime your “AD Kitchen.” In cooking shows, hosts show you how to prep a meal, pulling out the final, cooked meal from the oven in the following scene. For an AD visit, you should think about how you can prep your ‘ingredients’ for clinicians by making sure you’re well-versed in your materials and are ready to teach your clinicians how to adopt something practical and usable into their practice. Have a tool to share? Test it in advance of your visit, so you can confidently demonstrate effective use of the tool, leaving more time to discuss applying the tool successfully in practice with patients. Want more tips? Stay tuned for the next installment in our Words of AD Wisdom series, and reach out to the NaRCAD team, subscribe to our network, or check out our discussion forum to hear more tips and ways to prime your AD kitchen for an efficient visit!  Biography. Chirag is a clinical pharmacist, academic detailer and instructor with Illinois ADVANCE at the University of Illinois-Chicago (UIC). He graduated with a Doctor of Pharmacy degree from Midwestern University in 2012 and has been working at UIC ever since. During his time at UIC, he has been involved in a number of collaborations with the College of Pharmacy, College of Dentistry, and College of Medicine in addition to teaching Medical Improv, which utilizes the techniques of improvisation to improve communication skills amongst current and future healthcare practitioners. He has also been focused on academic detailing, including program planning, presentations to recruit organizations, creating educational material, training staff, facilitating role plays and providing individualized feedback, and detailing prescribers. He trained with NaRCAD in 2019 during their Spring Training Series to develop his skills as an academic detailer and has also presented at the NaRCAD annual conference. His interests include performing improv, podcasting, sports and hanging out with his sister’s dog. Fun fact: Chirag hiked Mount Kilimanjaro in February of 2022. An interview with Ellen Dancel, PharmD, MPH, Director of Clinical Materials Development, Alosa Health. Ellen completed her pharmacy practice residency at Massachusetts General Hospital and later completed her Master of Public Health at Boston University. by Anna Morgan, MPH, RN, PMP, NaRCAD Program Manager Tags: Materials Development, Detailing Visits, CME  Anna: Hi Ellen! Thanks for joining us today – we’re excited to hear about your 6+ years of experience developing impactful detailing materials. Can you walk us through the process you take when beginning to design a detailing aid? Ellen: Absolutely! The most important question to start with is, “who are you detailing with this material?” You also want to consider who is driving the goals of the intervention. Is there something your funder wants you to communicate in terms of key messages or is there new clinical information to convey? You then need to think about how to engage subject matter experts (SMEs). We work with an amazing endocrinologist for our diabetes modules and often ask, “what do you wish a primary care provider (PCP) knew before they referred a patient to you?” Having a specialist’s perception on what concerns they see in practice is key. We’re also fortunate to have access to focus groups at Alosa. We engage prescribers who receive our content to understand their needs on a topic. These peer-to-peer conversations are hosted by one of our clinicians. We also utilize our detailers’ years of expertise, gaining their insights on the materials. We use these two distinct focus groups to provide feedback on the content and messaging as well as the layout and visuals of our draft materials. We then take all this information and add it to the available literature to create a final detailing aid.  A screenshot of a cover page A screenshot of a cover page Anna: These first steps are crucial when thinking about developing materials. Let’s talk about the layout of the detailing aids. What does that look like? Ellen: When it comes to laying out the detailing aid, Alosa has a certain look and feel that we always use that’s part of our brand. The front of the document is a cover page with a title and graphic. Our graphic designer does a tremendous job of taking a concept that isn’t quite fleshed out and making sure that the end product is streamlined. A title that works well is something that is very clear, simple, and focuses on the overall message. Our team selects images for the cover page that relate to the topic but also tend to generate conversation. The back has our logos and a description of the authors. On the inside, we start with a “why do I care?” section, so we can explain why the topic we’re focusing on is of importance to the clinicians being visited. The next page is often a summary of the content that is within the detailing aid. A summary could be an algorithm for treatment or a graphic for a framework for thinking about how to approach management (e.g., the four stages of heart failure). This is followed by the evidence, data, and tips to support a PCP in order to put the key message into practice. We follow that with a cost page, so the clinicians are informed when presenting new medications to patients. Lastly, we include a reminder page that summarizes key points.  A screenshot of details on cost of medication A screenshot of details on cost of medication Anna: Wow! It’s so helpful to hear about the process your team uses for laying out content in the detailing aids at Alosa. From start to finish, how long does this entire process take? Ellen: It really depends on the topic. For example, if we’re updating a topic with a SME who has previously worked with the Alosa team, then we’d expect a timeline of around two to three months. For something new, such as a primary palliative care module or a serious illness module, we’d plan for a timeframe closer to four to six months, because we need the time to really look at the evidence and see how it shapes what we want to accomplish in the field. We also need the time to understand what our PCPs are interested in through feedback from a focus group and informally from our detailers. For AD programs with shorter timelines, we’ve found the resources at the CDC to be incredibly useful, such as the adapted patient materials for our latest immunizations module. There’s also a lot of academic detailing programs that have publicly accessible materials. Some may even allow you to use their graphics if you request permission or cite appropriately.  Anna: It’s so important to allow enough time to not only create and build a detailing aid, but also work through multiple revisions of it. Ellen: I couldn’t agree more. When I created my first detailing aid, it took me a week to even come up with the first draft, which was then subsequently torn apart. My draft looked nothing like what we ended up with at the end of the process. Programs need to plan for time for back and forth communication and to engage as many viewpoints as they can. Our modules are accredited for continuing medical education and we have reviewers assess the detail aid to ensure accuracy. We also make sure that our detailers, who will be using the material in the field, have an opportunity to try out the materials. We often end up changing key graphics that we thought were fantastic but turn out to not be effective during the detailing visit through this process. Anna: When thinking about the gold standard for creating a detailing aid that is accessible to both detailers and clinicians, what comes to mind? Ellen: It’s really a marriage of evidence-based recommendations and clinical practice. We’re trying to find a way to bridge recommendations in the literature with usable tools for a busy primary care provider’s practice. We make sure we’re providing the best and latest evidence in a way that can be helpful for the primary care provider without them having to do a complete system redesign. Materials should be streamlined and allow clinicians to be flexible in their approach by offering different options in adopting the key messages.  Anna: Thanks for walking us through this process, Ellen- what would you say are the key tips/takeaways for detailing programs who are just starting to do this? Ellen’s Tips for Creating Materials
Learn more by checking out the Alosa website, and these detailing aid building tools and examples from the NaRCAD team. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Ellen was a pharmacist at the Massachusetts General Hospital for ten years prior to joining Alosa Health, serving in various leadership roles. She received her MPH in epidemiology from Boston University where she worked on a project looking for potential economic efficiencies in the global donor-funded antiretroviral market. As Director of Clinical Materials Development, she leads the development of evidence-based, academic materials, in partnership with clinical experts, and oversees the production of clinical content from concept to completion. An interview with Julie Anne Bell, MPH, Program Manager of Clinical Operations, Bureau of HIV, New York City Department of Health and Mental Hygiene. The mission of the Clinical Operations and Technical Assistance Program (COTA) is to provide innovative, culturally responsive, needs-based technical assistance and training to organizations and individuals working with people impacted by HIV. by Anna Morgan, RN, BSN, MPH, NaRCAD Program Manager Tags: Detailing Visits, E-Detailing, HIV/AIDS, Materials Development  Anna: Thanks for joining us today, Julie Anne! Can you tell us about yourself and what brought you to your role as Program Manager of Clinical Operations at the New York City Department of Health and Mental Hygiene? Julie Anne: My first position out of graduate school was as a research assistant in the HIV program at the State University of New York. I’ve moved through a lot of sexual health work and have been with the Bureau of HIV at the New York City Department of Health and Mental Hygiene for three years. I love the programmatic work that I do in my current role. I deliver training, tailored technical assistance and public health detailing to clinical and non-clinical providers who care for people with HIV. Being a content expert and bringing the information directly to the clinics to support them is rewarding and, most of all, fun.  Anna: It sounds like your career path has led you to a wonderful position! What detailing topic is your program currently working on? Julie Anne: We’ve been focused on developing a public health e-Detailing campaign to support and strengthen providers’ initiation of immediate antiretroviral treatment, or “iART”. iART is for people newly diagnosed with HIV or returning to care after a long lapse. It recently became a standard of care in New York. Immediate initiation of ART is associated with several health benefits for people with HIV, including a significant decrease in the time to viral suppression, which ultimately, reduces the risk of disease progression, morbidity, and mortality for people with HIV as well as onward transmission and new HIV diagnoses. Prescribing ART immediately versus waiting for the patient to return after all lab work/genotype results come back can feel like a paradigm shift for providers, but HIV medications have advanced so much in terms of their high threshold to resistance and there is no longer a need to wait. Anna: Your team recently completed a campaign on strengthening the integrated care approach, which is a team-based approach where mental health care and medical care is offered to patients in the same setting. How did your previous campaign help shape your new iART campaign?  Julie Anne: During our previous campaign, we brought providers an array of materials and resources to help them meet New York City’s Ending the Epidemic benchmark. We included HIV-specific materials and resources, as well as additional tools to address substance use, housing, and mental health in order to strengthen their integrated care approach. Among those HIV-specific materials and resources was information about iART. During our detailing sessions, providers were consistently reporting the same barriers to implementing iART in their clinics. Barriers that were reported were lack of clinic workflow for iART, not knowing how to get the medications covered/paid for immediately, and feeling uncomfortable prescribing ART before receiving a lab based confirmatory HIV test and genotype testing result. We began to realize that the providers needed more support around this topic. Because our work is heavily data driven, we used the feedback we received from providers on the barriers they were experiencing around implementing iART to create our iART campaign and associated public health detailing action kit. The tools and resources in our detailing action kit highlight each component of iART, including HIV testing, payment options, genotype testing, and example clinic workflow. In the past, our program developed the public health detailing action kits and would hire consultants to do the detailing. For these campaigns, my colleague and I wanted to deliver the messages to the clinics ourselves and focus on relationship building. Anna: Having strong detailer-clinician relationships is an integral piece of a successful academic detailing program. How have you been able to build strong relationships with clinicians?  Julie Anne: We visited over 100 clinics that provide HIV services in New York City during our last detailing campaign, and we now have friendly relationships with these providers because of the trusting relationships we’ve built with them through our previous detailing work. Our team also attends regional group meetings for HIV providers to bring more awareness to our work and continue to build relationships and connections. We recently hosted a virtual launch event for our iART campaign and we had over 200 providers register. We provided an overview of COTA, our services, and e-Detailing. We wanted the providers to know exactly how we’ve pivoted during COVID-19, why this work is still important, and that we would reach out to them in the coming weeks for an e-Detailing visit. Being with the health department, we know where people are getting their care for HIV in New York City. We’d love to reach everyone who’s working with people who are impacted by HIV, including non-clinical providers. Since iART is an integrated care approach, both clinical and non-clinical providers are an integral part of the process. The first steps in the iART process begin with a positive HIV test which can happen in a non-clinical setting, such as a community-based organization. The next steps include looping in a medical provider with the addition of non-clinical support, such as benefit navigation, social work, and peer navigation. It can take multiple providers of different training and expertise to work together to achieve iART seamlessly.  Anna: Wow! You’re certainly connected to a lot of clinics and it doesn’t sound like you’ll have issues recruiting clinical or non-clinical providers for your upcoming e-Detailing visits. How has your team prepared for e-Detailing? Julie Anne: When the reality of the pandemic hit, the idea of transitioning our detailing program to a virtual platform was overwhelming. We did a deep dive into the existing literature to see how programs have done virtual detailing in the past. NaRCAD has also been an amazing resource to learn from and we continually check the website for new resources on e-Detailing. We then developed a Standard Operating Procedure (SOP) for our iART e-Detailing campaign. We worked as a team to create a step-by-step guidebook that includes our key messages, how to do a needs assessment, and how to address barriers that we expect might come up. We’re currently working on doing mock e-Detailing sessions with our colleagues and with providers who are iART champions in New York City. Our SOP will help guide us during these mock sessions and help prepare us for our field visits this fall. Anna: Creating a Standard Operating Procedure is a great idea and will be extremely beneficial to prepare for field visits. What are some challenges that you expect to face when you begin your e-Detailing work? Julie Anne: We’re expecting the usual technical problems like poor internet connection and access issues, but we’re working on strategies to overcome this. We also expect that providers will be experiencing burn out, so they may be hesitant to make some of the changes in their clinic to implement iART, such as establishing a new clinic workflow. However, the resources we’ve selected and created for our iART detailing action kit are a direct result of what providers reported that they needed during our last detailing campaign. We’re hopeful that the tools we’re providing will enable an easy transition for providers to adopt our key messages related to iART.  Anna: It’s remarkable that you’ve been able to create your e-Detailing campaign based on the specific needs of the providers in your community. How else is your team working towards sustainability? Julie Anne: iART is a sustainable practice because once providers understand the “why” and “how” to do it and the steps involved, there is no reason to go back to waiting to initiate a patient with HIV on ART. It’s important that people with HIV are given the opportunity to start ART immediately because it provides individual and public health benefits. iART is the new standard of care in New York, which encourages providers’ commitment to the practice, and the iART detailing kit will introduce tools and resources to increase the knowledge and confidence of providers to prescribe ART immediately. Additionally, COTA offers ongoing technical assistance at the request of the providers and full-day trainings on iART for new providers. We’re currently focused on our iART e-Detailing project, but it’s always an open-door relationship with providers. Right now, it’s iART, but providers can reach out to us about anything they’re struggling with and we’ll work with them to overcome the challenges they’re facing. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Julie Anne began working at the NYC Health Department in 2016 with the Bureau of Sexually Transmitted Infections in a research role. She transferred to the Bureau of HIV in 2017 where she focused on health policy work, and was promoted to her current role with the Clinical Operations team. She now manages the team that focuses on providing data-driven technical assistance to clinical and non-clinical HIV providers across New York City on HIV specific and supportive topics that address social determinants of health for people with HIV. Julie Anne is currently preparing to conduct e-detailing visits with NYC providers to support and strengthen practices for initiation of immediate antiretroviral treatment (iART) for people with HIV. An interview with Ramona Shayegani, PharmD, Program Lead, Academic Detailing Service, Veterans Affairs Southern Nevada Healthcare System by Kristina Stefanini, NaRCAD Project Manager Tags: E-Detailing, International, Materials Development, Opioid Safety, Substance Use, Rural AD Programs  Kristina: Programs are transitioning their academic detailing (AD) efforts to e-Detailing or virtual detailing amid the COVID-19 pandemic. As part of your role at the Veterans Health Administration (VHA) Academic Detailing Service, you’ve completed e-Detailing visits, which you presented on at the NaRCAD 2019 conference. I wanted to interview you today, Ramona, to learn more about how you transitioned to e-Detailing. First, how did your program decide to do e-Detailing? Ramona: Thanks for interviewing me! We heard about an e-Detailing pilot project from our national office and we were excited to participate as our region is spread out and rural, covering Nevada, northern California, Hawaii, and Manilla, Philippines. We felt this would be an excellent setting in which to incorporate video calls into our communication with clinicians. As a result, e-Detailing has allowed us to reach our full potential as a service. Kristina: Amplifying a program’s impact and reach through e-Detailing is something many other programs want to experience. Have providers been receptive to e-Detailing visits given the current COVID-19 pandemic? Ramona: I think it varies by site, but for the most part, providers are very eager to learn about the VHA’s telehealth program. Initially, when we started e-Detailing, we launched a campaign to encourage clinicians to complete telehealth visits with patients. Now providers remember our names, and they reach out about setting up telehealth meetings with their patients and figuring out how to conduct video calls. It’s very rare for providers to reach out to academic detailers for help. We usually have to initiate outreach requests. Kristina: That’s terrific that clinicians are the ones reaching out for the service. When you’re getting ready for an e-Detailing visit, do you prepare the same way as you would for an in-person visit? What materials do you use, and how do you use them?  Ramona: The campaigns we’re working now are so fast-paced, so we’re sharing materials via PowerPoint presentations on a video conferencing platform; we also use electronic PDFs. In addition to showing providers electronic materials, you can still model an approach as you would in person by holding up some of the materials on the camera. For example, with naloxone education, we have naloxone spray “dummy” versions that I show providers on video; I ask if they have ever seen what a naloxone spray looks like, and whether they would be interested if I sent a model version, which they usually say yes to. Kristina: That’s something we try and tell detailers who are pivoting to e-Detailing, which is that much of the interactive approach of an in-person visit is still accessible via video! Many detailers who are trying this out for the first time are eager to find ways to build a meaningful, trusting relationship with clinicians--do you have any advice for strong relationship-building approaches during e-Detailing visits?  Ramona: Sometimes, especially if it’s a new provider, I try to remind myself that I might not get to talk about any of the key messages. It’s really important to take that time to introduce yourself and your service. I don’t feel like it’s anything different than meeting someone face-to-face for the first time. However, detailers need some time to try this with each other, their team, or providers that they have a good relationship with. Detailers need to build that confidence before they go out and try these video calls with people they’ve never spoken with. The more I do it, the more confident I feel, which is key in building these relationships. Kristina: That makes sense—it’s about comfort and confidence as much as knowing the evidence. We’ve also encouraged detailers to know that it may take more time to build up to delivering the key messages than you’d like it to, and to be patient and focus on building the relationship when carrying out visits online. In your experience, have you seen any drawbacks to e-Detailing? Ramona: One thing is that detailers don’t have the luxury of getting a feel of what the clinic is like, which would be easy to observe in person. A lot of times when I am in a clinic, I get a chance to talk to an auxiliary support team, or I could just walk to the other room and talk to the nurse. I’ve found ways to adapt to e-Detailing to try and have more of the team’s perspective; I’ll often ask providers if they think it would helpful for the nurse to be on the call so we can have a group discussion. Kristina: It’s really about thinking outside the box and adapting the in-person approach, while trying to maintain connection. Is there anything else you’d like to share from your experiences with implementing e-Detailing? Ramona: Detailers should acknowledge that this is a brand-new approach; you may not feel like this is your preferred way to talk to providers. Remember that it will take some time to get comfortable with it. There’s a learning curve. Now that I use this approach full-time, I just love it, and I don’t want to go back! It’s just as effective, a lot more efficient, and it allows you to be flexible.  Biography. Ramona Shayegani is the program lead for VHA’s Academic Detailing service in northern California, Nevada, Hawaii and Manila. She received her Doctor of Pharmacy degree from Oregon State University in 2014 and has clinical background in mental health and addiction medicine. She was one of the first detailers to pilot e-Detailing at the VA and has completed over 400 virtual detailing visits. An interview with Zack Dumont, BSP, ACPR, MS, a clinical pharmacist with the RxFiles Academic Detailing Service in Regina, Saskatchewan, Canada and a NaRCAD Training Facilitator by Winnie Ho, NaRCAD Program Coordinator Overview: The Cannabis Act went into effect in Canada in October of 2018. The legalization of a drug with strong potential for a myriad of clinical uses was followed by many questions from patients and providers alike about its effectiveness, its safety, and lack of previous research. The RxFiles have carried out a cannabinoid academic detailing campaign to address the demand for truth in a time where research has just begun to shed light on previous myths, misconceptions, and clinical promises. Tags: Health Policy, International, Materials Development, Opioid Safety, Stigma, Substance Use  NaRCAD: Zack, thank you for taking the time to speaking with us today! RxFiles has been around for more than 20 years. What do you do you believe is driving the demand for the resources that academic detailing is providing? Zack: There’s an element of doubt in the information out there, because people have experienced misinformation before. People are often interested in the truth and that’s one of the most amazing things about academic detailing. There is also a desire for practical information that can be used to actually treat patients, and there’s a ton of overlap there. These things are important to these very, very busy providers who want the best for their patients. NaRCAD: We know that your team is working on a cannabinoid campaign, which can be a nebulous topic. Can you discuss a little more about cannabinoid policy and conceptions in Canada? Zack: We’re coming up on the one-year anniversary of recreational marijuana legalization, but medicinal cannabis has been legal for about two decades. With the legalization of recreational cannabis though, we’re seeing fairly rapid change in perceptions of what the truth is. It’s tough to keep up with. With academic detailing, it was challenging to decide how to tackle it – can we just talk about the medicinal cannabis side? Or do we have to dive deeper? When we dug into it, it became clear that we also had to talk about the recreational side. For example, the people we provided our services to also wanted to know, “if I decline my patient cannabis prescriptions, what will they be able to get on their own?”  NaRCAD: Did RxFiles choose to launch its cannabinoid campaign with the passage of the Act, or has this been planned for a longer period of time? Zack: It’s coinciding with our work on pain, following our work on pain and opioids. In addition, because legalization was approaching, the providers had more questions because their patients were asking about cannabis as an alternative to opioids. NaRCAD: How have provider responses been to the cannabinoid campaign so far? Zack: It’s welcomed. Our information is usually welcomed. There’s some frustration over how little information there is out there. While frustrating, I think it’s kind of comforting to know that we’re not that far behind. It’s kind of mixed, but at the same time, they’re still happy to get information from a trusted resource. There's a lot of gray area information right now because it's a newer field.  NaRCAD: Right now is a shifting and transformational time, especially with something like cannabinoids with a distinct history of stigma and legalization, even with all this new interest. As an academic detailer, how do you source your information knowing that there isn’t enough research out yet and a lot of gray area information? How do you begin to build a campaign around a topic like this? Zack: The evidence pyramid gives us the best approach for practical information, for people who are the interface of care. You want to find high quality, synthesized information. Whether its osteoporosis or COPD or pain or cannabis, you start with the guidelines and figure out what kind of information they are providing. We started with some recently published guidelines and it was a synthesis of systematic reviews, and made an attempt to summarize all the evidence of where cannabis was found to be of benefit. We also reviewed the bibliography with all the primary literature and metanalyses. This process is pretty similar for any academic detailing topic. The other process is going to the people we provide services for, and asking what their patients are asking to treat with cannabis. They tend to ask about cannabis for pain, insomnia, or for things like tremors and that gives us some guidance in terms of what kind of literature we want to find. Of course, we are also looking into what the key messages are in the information we find and distribute. With cannabis, the interesting thing was the lack of information on the different conditions it could be used for. In some ways, it was easier, as weird as it sounds. We didn’t have as much reading to do on that topic.  NaRCAD: Is there any advice you would give any other academic detailing organizations considering this topic for a campaign? Zack: One, you’re going to have your conversations about stigma. There isn’t a perfect picture of who uses cannabis and it could be absolutely anyone. You’ve got to have the conversation about stigma and get to know your own biases. In the same vein, we thought about how important word choice and language is. We thought about whether or not we call it cannabis, marijuana, pot, or cannabinoids. Do we call it a medication or a product? All of those words and the considerations that we’ve given opioids - do we call them "addicts", or is it "dependence", and what are the differences between addiction and dependence? The third piece would be that you’ve got to talk to your providers in your local area and find out what their main questions are. Your job is to provide a service, and if you can find out what their wants and needs are, you’ll provide a far more satisfying service for them and could establish strong relationships that you can build on. There will be a lot of information out there and you will need a lot of leads to help you sort through it all. This won’t be the last time we're addressing this. NaRCAD: Thank you for taking the time to speak with us, and for leading the charge in bringing cannabinoids to the conversation about treatment for pain.  Biography. Zack Dumont is an clinical pharmacist with the RxFiles Academic Detailing Service in Regina, Saskatchewan, Canada and a new expert facilitator for NaRCAD's training courses. He has been involved with the RxFiles since 2008, with experience in both academic detailing and content development of RxFiles’ evidence-based drug therapy comparison tools. Zack maintains clinical practices for inpatient internal medicine, with more specialized experience in anticoagulation and heart failure. His professional interests include teaching evidence-based medicine, knowledge translation, development of clinical decision supports, collaboration, and leadership. Zack graduated as a Pharmacist from the University of Saskatchewan in 2008. Following graduation, he completed a hospital pharmacy residency with the Regina Qu’Appelle Health Region, where he currently serves as a Clinical Support Pharmacist, with involvement in training new staff, precepting pharmacy residents and undergraduate students, and providing clinical support to various health region committees and working groups.  Tags: Detailing Visits, Evidence-Based Medicine, Materials Development, Jerry Avorn Here’s the good news: academic detailing is becoming so widely accepted that everyone wants to help provide the evidence that is disseminated. That’s also the bad news; worrisome examples range from the grotesque to the sinister. One eminent health policy expert wanted to know how much it would cost to put together a nationwide academic detailing program (my heart leaped) that would be underwritten by the pharmaceutical industry (dammit). Prescription drug management (PBM) companies now offer so-called academic detailing services as part of their contracts with payors to oversee drug choices and spending. Sounds good until one realizes that a large chunk of PBM revenue come from payments by manufacturers to move market share to their products. So much for communicating evidence that is neutral, unbiased, and non-commercial. You’d think we’d have learned our lesson by now. Do universities or insurers or government fail to offer enough continuing education about prescribing? No problem, drugmakers will be more than happy to fill the gap, either for free or at amazingly low cost…. often with really great food. That local clinical expert who shows up at Grand Rounds to provide an overview of all the new treatments for diabetes, at no cost to the hospital? Don’t ask who’s paying him to be there. And those convenient smartphone apps that provide so much handy dosing information for any drug you can think of? All you have to do is read the commercial messages that pop up on your way to the data, as the vendor promises its pharmaceutical sponsors the chance to "embed your brand message at multiple points across the care continuum."  There is a solution to the concern about who’s providing the content for academic detailing programs, and it’s much easier than figuring out whether a particular Facebook ad is brought to you by a Russian bot. Just expect that any purveyor of AD information will reveal clearly all the financial ties it and its authors have with any drug or device maker, in relation to program sponsorship as well as the creation and editing of the clinical content. After years of being misled about hidden data on adverse events or failed studies, we’ve developed a higher set of expectations about disclosing all information about clinical trials, and the need to reveal authors’ financial ties for published studies. Those same higher standards must also be applied to academic detailing programs, so that its audiences will know whether the material is the carefully vetted work of a team of unconflicted reviewers who don’t work for any manufacturers, or is instead yet another terribly sophisticated new way to market particular products. Want more? Peruse the archive of Jerry's pieces here on DETAILS. _____________________________________________________________ Biography.
Jerry Avorn, MD | NaRCAD Co-Director Dr. Avorn is Professor of Medicine at Harvard Medical School and Chief of the Division of Pharmacoepidemiology and Pharmacoeconomics (DoPE) at Brigham & Women's Hospital. A general internist, geriatrician, and drug epidemiologist, he pioneered the concept of academic detailing and is recognized internationally as a leading expert on this topic and on optimal medication use, particularly in the elderly. Read more.  Guest Blogger: Joseph Leishman Academic Detailer/Masters in Public Health Candidate Center for Clinical Management Research, Ann Arbor VA The University of Michigan School of Public Health NaRCAD Training Alumnus Tags: Cancer, Detailing Visits, Materials Development, Training  NaRCAD: How did you get into AD? What were you doing before? Joe: I’m a graduate student at The University of Michigan School of Public Health studying epidemiology. As a student I started working at the Ann Arbor VA Center for Clinical Management Research on a lung cancer-screening project. Our project involves 8 different VA sites across the country. As we shifted into an implementation phase, academic detailing was selected as an implementation method. I transitioned to an academic detailer role because of my background in epidemiology, my understanding of lung cancer screening (LCS), and my ability to communicate these principles. I attended the NaRCAD academic detailing techniques training and things took off from there! 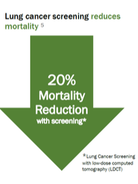 NaRCAD: Why is AD for lung cancer screening so important? Joe: Lung cancer screening can be more complex and complicated compared to other preventative services, and most primary care physicians have very limited time to discuss lung cancer screening with patients. There are a number of potential downsides to screening – false positives, overdiagnosis, invasive procedures, and complications from invasive procedures. The benefits of the screening outweigh the challenges, and we have developed a tool for doctors to quickly evaluate a patient’s lung cancer risk, facilitate shared decision making, and make personalized screening recommendations. NaRCAD: Tell us about the lung cancer screening detailing aid and related tools that you made with NaRCAD’s support. How was the process of developing the detailing aid? Joe: Our detailing aid contains background information on lung cancer screening and some of the key evidence behind our tool. It also outlines some of the reasons and benefits behind using this risk-based approach. We tried to keep the detailing aid simple enough that doctors could quickly understand the concepts with little or no additional explanation. This was our group’s first attempt at making something like this. We worked with NaRCAD during the creation of the detailing aid to improve the clinical content, layout, and language. There was a lot of trial and error to create the detailing aid. We ended up going through 10 versions before it was finalized.  NaRCAD: How did you decide what information was most important to put on your detailing aid? Joe: Initially, we started out with too much information. It was too complicated and wordy to effectively communicate our message. We tested it out with our team to see if our message was clear. It was obvious when sections of detailing aid didn’t work well. We really had to focus on narrowing down the main evidence and messages we wished to convey. We used the primary lung cancer screening evidence from the US Preventative Task Force and the National Lung Screening Trial. Our tool goes a step beyond screening eligibility to look at individual risk, life expectancy, and patient preferences, which help providers get past some of the difficulties and complexities of lung cancer screening.  NaRCAD: How does your website complement the detailing aid when you are 1:1 detailing? Joe: A link to the tool is embedded in the Computerized Patient Record System (CPRS), the EMR system that the VA uses. However, it can be also accessed outside the VA with a URL. What I typically do is I have PCPs pull up the website in their workspace after going through the detailing aid. I have providers role play with a sample patient, and I demonstrate how the tool could be used for that specific patient. Using the actual web tool in a detailing meeting really helps to reinforce our message. We feel like it increases the likelihood that it’ll be adopted in an actual clinical practice. NaRCAD: How have clinicians been responding to your campaign? Joe: So far there has been a decent response from the doctors we have worked with. Some of the doctors in the VA have met with detailers before which makes the initial contact easy. However, the most majority of the doctors I have met were receptive to my visits. We’ve been tracking the use of our tool before and after academic detailing at a site level. We don’t have exact numbers, but there has been an increase between before and after AD. We’d be happy to share more complete data in a future blog post.  NaRCAD: That'd be terrific, we'd love to share that when it's ready! What other reflections do you have from this process that you'd like to share with our community? Joe: Academic detailing is a new approach for our group. It has been a real learning experience for discovering what does and doesn’t work and how to best address provider needs. For me, going through this process has been a lot of fun. I love talking with doctors about their struggles and being able to offer a tool that can help them better handle lung cancer screening with their patients. An Interview with Mass Mental Health CenterFeaturing Mark Viron, MD, adult psychiatrist & Director of Health Home Services at the Department of Mental Health’s Massachusetts Mental Health Center (MMHC) in Boston; Assistant Professor at Harvard Medical School. Tags: Materials Development, Mental Health, Smoking Cessation, Training NaRCAD: We’re excited to talk about your program because it focuses on such an important population, and such a specific topic that’s been a focus of public health initiatives across the nation. Tell us about Massachusetts Mental Health Center (MMHC).  Mark Viron: MMHC is a Department of Mental Health (DMH) community mental health center in Boston that has provided mental health services for over 100 years to people with chronic and persistent mental illness. Its ultimate goal is to help people maintain meaningful and productive lives in their community. In 2013, to better address the significant unmet primary care needs of our patients, we launched the Wellness and Recovery Medicine (WaRM) Center. The WaRM Center offers co-located and integrated wellness and primary care services for all MMHC patients.
NaRCAD: Why, historically, have rates of tobacco use been higher in folks with serious mental illness (SMI)? Why has there been resistance for clinicians to promote tobacco cessation for this group? Mark: It’s a complicated issue. There are risk factors that increase the rate of smoking in this group and these are coupled with obstacles to getting appropriate treatment. People with SMI are overrepresented among populations that face social and environmental conditions that are typically associated with an increased prevalence of smoking – poverty, unemployment, limited education, etc. Obstacles to quitting include limited availability of resources, lack of clinician involvement, and poor social/peer support.
 The strategy of AD: 1:1 clinician-facing outreach. The strategy of AD: 1:1 clinician-facing outreach. NaRCAD: Agreed! What do these AD-focused, 1:1 visits between trained physician educators and psychiatric prescribers entail? Mark: The visits are 20-30 minutes long and follow the typical detailing visit structure. Visits are conducted by me, a psychiatrist at MMHC, or Gail Levine, MD, an internist and the Medical Director of our primary care clinic. We meet with the prescribers in their offices, and begin by asking open-ended questions to assess their needs and learn about their successes (and challenges) in addressing tobacco use with their patients. We celebrate successes and validate challenges, and then pivot to sharing evidence-based information and key messages that may help them address these issues with greater success. We conclude the visit by reviewing steps the prescriber can take to increase successful tobacco treatment, and provide a copy of our detail aid, along with a few high-yield references.  Click to see complete detail aid. Click to see complete detail aid. A key ingredient to our success has been our detail aid. A great psychiatry resident (now attending), Kathryn Zioto, worked with Gail and me and the NaRCAD team to develop a detail aid about tobacco treatment in people with serious mental illness. The detail aid contains cutting-edge, evidence-based information in clear language with colorful graphics. It includes information about the MMHC’S Smoke Free Team, and highlights our three “asks”, which helps clinicians frame their conversations with patients:
NaRCAD: We enjoyed working on this important project with you, and we know how important great materials are in engaging clinicians to consider behavior change. That said, how have psychiatric prescribers been responding? Mark: The response has been quite favorable. It's been rewarding to sit down with colleagues and learn from their experience and expertise and to be able to offer some useful information about tobacco treatment and the Smoke Free Program. The one-on-one detailing encounters, even as brief as they are, give us quality time with our colleagues to focus on their individual concerns and questions. We probably get as much information as we give!
 NaRCAD AD Trainings: hands-on and interactive. NaRCAD AD Trainings: hands-on and interactive. NaRCAD: Two members of your team, yourself and Gail Levine, attended our AD Techniques Training in 2015 to prepare for this initiative. How has the training helped you provide this education to prescribers? Mark: Your training gave us an in-depth immersion into the world of academic detailing, helping us understand theories and evidence and think about implementation issues. Getting to practice detailing and getting feedback from experts in the field was invaluable, as was the ability to talk with people from around the country who are working on similar projects. NaRCAD's training is incredibly worthwhile – it was compact, comprehensive, and helped us acquire the needed skills to implement this project successfully.
 Provider education, engagement and activation are key, and AD provides a framework that has a proven track record in producing results in these areas. Plus, AD is efficient and easily implemented relative to other interventions--especially when you have assistance from NaRCAD! NaRCAD: Thanks for taking the time to connect with us. We’ve enjoyed helping to support this initiative with training and materials development! We look forward to continuing to learn about the impact you have on improving the health of people with serious mental illness, and sharing it with the community. We can't wait to hear more about this intervention at our conference this fall!  Biography. Mark Viron, MD is an adult psychiatrist and Director of Health Home Services at the Department of Mental Health’s Massachusetts Mental Health Center (MMHC) in Boston and an Assistant Professor at Harvard Medical School. He specializes in the treatment of psychotic disorders and the integration of primary and behavioral healthcare for people with serious mental illness. He graduated from Tulane University School of Medicine and completed his psychiatry residency at the Massachusetts General Hospital/McLean Residency Program. He serves as an attending at MMHC’s partial hospital program, where he teaches and trains residents and medical students. He is also the project director for two grant-funded initiatives that aim to enhance MMHC’s ability to provide integrated primary and behavioral healthcare.  by NaRCAD Staff Tags: Materials Development Mr. Wolfson is Executive Vice President and COO of the ABIM Foundation, a non-profit foundation focused on advancing medical professionalism and physician leadership to improve the health care system. Mr. Wolfson has been instrumental in leading the Choosing Wisely® campaign (www.choosingwisely.org), a multi-year effort engaging nearly 45 medical specialty societies to promote conversations between physicians and patients about utilizing the most appropriate tests and treatments and avoiding care that may be unnecessary and could cause harm. NaRCAD: Why did ABIM Foundation initiate Choosing Wisely®? Wolfson: The mission of the ABIM Foundation is to advance medical professionalism to improve health care. One of the ways we do this is through a small grant program called Putting the Charter into Practice. The National Physicans Alliance received one of these grants and used it to create the Good Stewardship Project, through which “Top 5” lists of overused tests and procedures were identified in internal medicine, family medicine and pediatrics. It was around the same time that Howard Brody called on specialty societies to create their own “Top 5” lists in the New England Journal of Medicine. We recognized this as an opportunity to tap in to physicians’ intrinsic motivation to care for their patients, as well as the alignment with the ideals of the Physician Charter. From there the Choosing Wisely® campaign was born. I think it’s one of the greatest examples of professionalism in action. NaRCAD: What are the primary goals of the Choosing Wisely® campaign? Wolfson: The goal of Choosing Wisely® has always been to encourage clinicians and patients to engage in conversations aimed at avoiding wasteful or overused tests, treatments or procedures. We do this by educating clinicians through lists created by specialty societies, and patient-friendly materials developed by Consumer Reports. There are many groups advancing the campaign throughout the country, including more than 20 grantees thanks to support from the Robert Wood Johnson Foundation. NaRCAD: What have been the biggest challenges to developing recommendations? Wolfson: In some ways one of the biggest challenges has been the sheer number of recommendations the campaign has generated. Oftentimes societies will survey their members for potential items to include on their list, resulting in far more recommendations than could feasibly be addressed. Culling these recommendations down to a manageable number is no small task for the societies; however it’s incredibly important so that we can focus efforts on reducing overuse in areas with the greatest potential to improve care. NaRCAD: Who is the audience for the recommendations – clinicians, patients, policy makers, or other groups? Wolfson: We think there are multiple audiences for the Choosing Wisely®recommendations, but the two primary audiences are clinicians and their patients. Each of the societies has created lists of tests, treatments and procedures in their own specialty they say are overused and should be questioned. This is important information for the clinician—but conversations are a two way street. That’s why the work of Consumer Reports is so important in translating complex medical information into materials patients can understand. Now clinicians and patients can engage in informed conversations based on sound evidence and science about what care is truly needed. NaRCAD: How is the ABIM Foundation disseminating the Choosing Wisely® messages? What role do you see for techniques such as academic detailing in that process? Wolfson: The ABIM Foundation works with the specialty societies to help disseminate messages about Choosing Wisely® to their members. This can take many forms, such as newsletter articles, videos, journals and at conferences. We’ve found Choosing Wisely® messages have really resonated through social media as well and inspired others to tweet and blog on the campaign regularly. The campaign has also reached consumer audiences through the work of Consumer Reports and a coalition of partners that includes AARP. And we’ve been pleasantly surprised by the coverage by mainstream media in outlets such as the New York Times, NPR, Vogue, Men’s Health, and all the major television networks. I think there’s an important role for academic detailing in advancing Choosing Wisely®. We know when information comes from a trusted source—such as a specialty society or colleague—that there’s a greater likelihood of behavior change. NaRCAD: In 5 years, how do you think Choosing Wisely® recommendations will have changed clinical care? Wolfson: Five years from now I hope the question “Are you Choosing Wisely?” becomes shorthand for clinicians in settings all across the country whenever they see areas of waste or overuse. I believe Choosing Wisely® will continue to inspire not just conversations between clinicians and patients, but also new projects that will formalize and put a structure around efforts to reduce waste and overuse. I’m very optimistic about our future. Bio: Daniel B.Wolfson, MHSA, is Executive Vice President and COO of the ABIM Foundation. Previously, Mr. Wolfson served for nearly two decades as the founding president and CEO of the Alliance of Community Health Plans (formerly The HMO Group), the nation’s leading association of not-for-profit and provider-sponsored health plans. During his tenure, Mr. Wolfson earned national recognition for spearheading the development of the Health Plan Employer Data and Information Set (HEDIS™), convening the RxHealthValue coalition to provide independent information on the pharmaceutical industry, and co-sponsoring with the American College of Physicians the journal Effective Clinical Practice. Previously, Mr. Wolfson was the Director of Planning and Research at the Fallon Community Health Plan. During that time, he led the product development team that launched the nation’s first Medicare risk contract with the Health Care Financing Administration. Mr. Wolfson received his master’s degree in Health Services Administration from the University of Michigan, School of Public Health. Learn more about Choosing Wisely. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|
