|
By: Aanchal Gupta, Program Coordinator, NaRCAD Tags: Detailing Visits, CME, E-Detailing You asked, we answered! Getting your foot-in-the-door to schedule a detailing visit is a challenge for many detailers. We’ve compiled some of our best tips about gaining access from our past interviewees on the DETAILS blog.  Relationship Building:
 Incentives:
Tools:
Our team at NaRCAD recognizes the difficulties detailers face in getting the 1:1 visit, and we’re here to support you! Check out the list below for more resources on gaining access. Additional Resources on Gaining Access:
Have any additional questions or thoughts on gaining access? Write to us in the comment section below! An interview with Carolyn Wilson, a Senior Health Program Coordinator at Ledge Light Health District. Ledge Light Health District is located in New London, Connecticut and is the regional health district serving the southern part of New London County. by Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Opioid Safety, Evidence Based Medicine, Substance Use  Ledge Light Healthwatch Ledge Light Healthwatch Anna: Carolyn, we’re thrilled to feature you on our DETAILS blog! I know you wear many hats – can you tell us about your current job role? Carolyn: I’m a health educator working within primary prevention, an academic detailer, and the host of our health district’s television program called Healthwatch. Healthwatch covers topics like mental health, physical health, disaster preparedness, general public health, COVID-19, environmental health, and disease prevention. I’ve been with Ledge Light Health District for 11 years. Anna: It seems like improving patient and community health outcomes is a common thread across all your roles. What primary prevention work or related projects complement your AD work? Carolyn: Depending on what topic I'm detailing on, I lean into my primary prevention work or the harm reduction work that my colleagues are working on. One of the larger initiatives I often share with clinicians during detailing visits is the Naloxone and Overdose Response App (NORA) project. The Department of Public Health developed a web-based application that can be downloaded directly to your phone. It has information about preventing, treating, and reporting opioid overdose. The app can be used by both folks in the community and clinicians. I also speak to clinicians about proper medication storage and disposal while promoting our “Take it To The Box” Initiative.  Anna: We love to see programs using AD to spread the word about broader, community-focused initiatives. Are there other ways that your opioid-related AD work overlaps with work being done within your department? Carolyn: Yes! I’m so lucky to be able to work in the office side-by-side a recovery navigator. She helps link folks in the community to addiction services. Every day we say things like, “hey, I overheard you talking to that pharmacist just now – do they know x clinician?” We often share resources and try to work together to ensure that community health goals are achieved, often by making sure that the work people are doing is connected rather than existing within silos. It all comes down to helping one another work towards a common goal. Anna: What better way to work towards a common goal than to share resources across colleagues and projects! Can you share a story from the field where there was an intersection among various projects?  Carolyn: I detail a lot of advanced practice nurses (APRNs) and also work with them on some of my primary prevention projects. The overlap in projects helps me build strong relationships with these clinicians. I sometimes work with school-based health centers as part of my prevention work, and these health centers are typically run by APRNs. These centers act as an access point to care for many students and families. It’s essentially a primary care clinic right in the school. The Child and Family Agency oversees the school-based health centers in southeastern Connecticut and reached out to me after a horrific event in a Connecticut middle school. A few months ago, a 12-year-old got access to fentanyl and brought it to school. He overdosed and passed away a few days later at the hospital. We haven’t seen many overdoses in schools, but after this happened, a lot of schools started looking at their policies and school-based health centers wanted to have naloxone on hand. The medical director of the Child and Family Agency advocated for a policy that required all school-based health centers to have naloxone and to be trained in administering it. Anna: What a devastating story. Have the school-based health centers been able to put these types of new policies into place? Carolyn: When one of the clinicians from the Child and Family Agency reached out to me, she said, “Carolyn, I know you do this kind of work. You trained me in naloxone not too long ago during an academic detailing visit. I’d like to have a naloxone training for my nurse practitioners in the school-based health centers. I want naloxone available in all of our clinics.” This type of request would typically be delegated to somebody else in our department, but because of the relationships I had built through academic detailing, I was asked to provide the training, and I did. As a result, the school-based health centers now all have access to naloxone and the clinicians know how to administer it.  Anna: It’s incredible that you’d built trusting relationships with clinicians enough to be asked to provide this training, contributing to changing a policy in a span of one or two months. Carolyn: It means a lot that they came to me because they trusted me and knew I could get it done for them. I truly don't think I would have been involved if it wasn’t for my academic detailing work. Anna: I agree. It’s been a pleasure learning about your work and your unique approach to academic detailing. We’re excited to follow along with you on your AD journey as you continue to promote health across your community. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Carolyn Wilson is a health educator and prevention specialist serving as a program coordinator at Ledge Light Health District in New London CT for 11 years. Carolyn studied public health and health education at New York Medical College. Keenly interested in health promotion and behavioral science, Carolyn enjoys bringing her passions and talents to both primary prevention and academic detailing work. Carolyn has been serving as an academic detailer for over 2 years and enjoys speaking with clinicians about strategies to prevent opioid related deaths. Carolyn also manages the Groton Alliance for Substance abuse Prevention @Groton_Prevents. In her spare time, Carolyn enjoys serving on the Board of Directors for the CT Association of Prevention Professionals and Fiddleheads Food Cooperative. To connect with Carolyn, find her on LinkedIn. Peer-to-Peer Learning: Building Meaningful Relationships through NaRCAD’s Peer Connection Program2/7/2022
An interview with Cheryl Radeloff, Senior Health Educator at the Southern Nevada Health District in the Office of Disease Surveillance. By Aanchal Gupta, Program Coordinator, NaRCAD Tags: Detailing Visits, HIV/AIDS, PrEP  Aanchal: Hi Cheryl, we’re looking forward to hearing more about your experience in the NaRCAD Peer Connection Program! How did you hear about the program and what encouraged you to sign up? Cheryl: I found out about the 2021 Peer Connection Program from a NaRCAD e-blast and was intrigued with the idea of joining a learning community. I instantly knew that I wanted to sign up since it would be a place where I could feel comfortable asking questions. I gravitated to the fact that I would be communicating with other peers in the field during cohort gatherings and learning about approaches that we could emulate in our program.  Aanchal: Yes, having that 1:1 time with your peer, as well as the cohort gatherings where other participants in the program come together, are added ways to network with the detailing community. Would you recommend this program to others that are interested in signing up? Cheryl: Absolutely! You should sign up even if you're a seasoned academic detailer or new to detailing. You're going to get tips, insights, and resources to get you started in a welcoming environment. This is a field where you never stop learning so it’s not only an opportunity to share lessons learned, but to learn from others as well. There are people from across the world who have different experiences and expertise that you can take back to your program.  Aanchal: One of the special aspects of the program is the sharing of resources and ideas. Are there any conversations that you had with your peer that made an impact on your detailing work or changed the way you thought about your program? Cheryl: The time spent with my peer was invaluable. During changing times with COVID-19, it can be daunting, and you tend to wonder if you’re doing things right or where you should even start. She was so generous in talking through challenges such as funding, recruiting providers, and more with me. She even shared a PowerPoint that they developed to educate pharmacy students about academic detailing. During the mid-point peer connection gathering, I was able to learn about a program in Chicago. They were very innovative; if they didn’t have an approach in place for their program, they designed it. Although my clinical topic may not be the same as others, there are still concepts and tools that I can model after these programs.  Aanchal: It’s great to hear about these fruitful conversations you had and how there’s always something to learn from others in the detailing community. How would you describe your experience overall with the peer connection program? Cheryl: Every time I attended a peer gathering, I always learned something and never had to question what I was gaining from these meetings. I think it’s essential to hear about what’s going on in the field. It’s difficult as we’re all busy people, yet it’s important not only for learning and development, but a necessary element to have peers to consult. I found the structure of this program to be helpful as we were given the reins to set up 1:1 meetings with our peer match over several months. In addition to that, there were gatherings where the entire cohort could come together and connect which I appreciated.  Aanchal: Those are some great takeaways, and we are glad to hear about the impact the program has had on your work! To wrap up, we’d love to learn more about what you’ve been up to at the Southern Nevada Health District. Cheryl: I’ve been with the Southern Nevada Health District for 13 years. Along with being a detailer, I’m also the public health co-chair for our HIV prevention planning group. We meet a few times a year to talk about HIV prevention initiatives, as required by the CDC. I also work with many of our community-based organizations to talk about the fundamentals of HIV. Academic detailing has been an important strategy for the work that we do. Our main AD initiatives we've been working on are uptake of PrEP and PEP. We have two PrEP navigators who've been educating the community about these initiatives. Lastly, congenital syphilis has been a big topic for us as we’re currently fourth in the country for the highest rates of syphilis. Aanchal: Thank you so much for sharing your experience, Cheryl. We’re so glad that the Peer Connection Program has had a positive impact on your detailing work and can’t wait to hear more about your program’s AD initiatives in the future. We look forward to continuing these connections with our 2022 cohort! Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography: Cheryl Radeloff is currently a Senior Health Educator with the Southern Nevada Health District Office of Epidemiology and Disease Surveillance. Formerly she was Disease Investigation and Intervention Specialist II. She is also an adjunct professor of Sociology at UNLV as well as Women’s Studies at the College of Southern Nevada. She received her Ph.D. in Sociology from the University of Nevada, Las Vegas in 2004. Her dissertation “Vectors, Polluters, and Murderers: HIV Testing Policies toward Prostitutes in Nevada” explored the development of mandatory testing laws for legal and non-legal sex workers in the state of Nevada. Her work duties include serving as the public health co-chair for the Southern Nevada HIV/AIDS Prevention Planning Group as well as training community providers on Rapid HIV Testing. She is the co-author of multiple editions of Transforming Scholarship: Why Women’s and Gender Studies Students are Changing Themselves and the World with Michele T. Berger for Routledge Press. The Impact of Childhood Experiences on Patient Health: AD to Encourage Trauma-Informed Care1/31/2022
By Anna Morgan-Barsamian, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD  As we’ve jumped right into 2022 programming, our team at NaRCAD continues to support detailing efforts that improve outcomes for vulnerable populations, recognizing that patient needs are complex and often informed by social determinants of health. One critical topic for which we’ve developed resources focuses on detailing to improve patient health as informed by both adverse and positive childhood experiences. We’re seeing an increased need from our community members to support detailing efforts related to this critical topic. We partnered with the National Association of County and City Health Officials (NACCHO), Centers for Disease Control and Prevention (CDC), and consultants from Brigham and Women’s Hospital and Tufts Medical Center over the past two years to develop academic detailing materials for clinicians working with both adults and children. The CDC defines adverse childhood experiences (ACEs) as traumatic events that occur in childhood, including abuse, neglect, and family dysfunction. These events are linked to poor health outcomes in adulthood like chronic health problems, mental health conditions, and substance use. When considering the impact of environment on health, the CDC notes that children are likely to flourish when they have safe, nurturing relationships. These supportive settings create the opportunity for positive childhood experiences (PCEs). PCEs can mitigate the effects of ACEs and toxic stress, promote healing from traumatic events, and foster healthy development and learning in children.  Encouraging clinicians to consider both ACEs and PCEs is a natural fit for clinical outreach educators. There are many reasons that clinicians may not be prepared to have conversations with patients about childhood experiences. Perhaps the clinician doesn’t have a behavioral health provider to consult within their practice, so they don’t know who to turn to if a patient discloses a traumatic experience. A detailer can encourage a clinician to explore this concern, as well as provide a list of local behavioral health providers in the community. Another barrier may be that clinicians could feel hesitant to approach discussions related to trauma, or may not have the skills to do so with sensitivity. In this case, detailers can offer tools that illustrate supportive language that creates a safe environment for patients to share their experiences. Supporting clinicians in using evidence-based tools to build trust with their patients signals that it’s not only okay to talk to patients about this sensitive topic; it’s vital for clinicians to lead these conversations in order to ascertain their patients’ needs and promote patient-centered decision making. A detailer can encourage clinicians to adopt new behaviors through specific key messages, including asking clinicians to take the following steps to support adult patients:
 When clinicians are supporting pediatric patients, detailers can deliver this set of evidence-based key messages, encouraging clinicians to:
 With evidence-based tools, successful AD interventions related to ACEs can result in multi-faceted support for patients, such as stronger connections with community resources, mental health supports, and more trusting relationships between clinicians and their patients. We hope to continue to explore this important and complex topic together as a community. If your program is currently working on an ACEs or PCEs AD campaign, or is interested in starting one, please reach out to us so we can support the development of your programming. We always love collaborating and learning more about the important work that you’re doing, and we hope to continue to build our resources and create toolkits in support of complex topics such as these that intersect with other behavioral health and prevention-focused AD campaigns. Have thoughts on our DETAILS Blog posts?
You can head on over to our Discussion Forum to continue the conversation! By: Aanchal Gupta, Program Coordinator, NaRCAD As we kick off 2022, it’s been incredible seeing the detailing community build on new and previous strategies over the past year. We’re continuously learning and sharing insights together. Let’s take a look at some of the advice shared on our DETAILS Best Practices Blog this past year.  Planning and Team Building: Communication, Trust, Building Morale
 Gaining Access to Clinicians
 Conducting Field Visits: Resilience, Empowerment, and Leverage
 Data Collection and Evaluation
Our team is incredibly proud to see all the dedication from the community each year. We look forward to seeing what opportunities and innovations 2022 brings.
Best, The NaRCAD Team  We’re featuring a snapshot from an academic detailing visit with Corinne Puchalla, PharmD, BCPS, a clinical pharmacist and academic detailer at Illinois ADVANCE. By Anna Morgan, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Substance Use, Detailing Visit  Hi Corinne! Can you tell us about a recent academic detailing visit that you’re proud of? Academic detailing does not come naturally to me—each visit starts with excitement, nervous energy, and the tingling anticipation of the unknown: Will the prescriber be in a good mood and be receptive to the key messages? Will I be able to express myself adequately? Will I negotiate the right “ask”? NaRCAD’s training elevated my confidence in making “the ask.” I’ve learned how to set small, quantifiable goals and give the prescriber a short timeframe for follow-up. My first academic detailing visit after the NaRCAD training had the potential to be a doozy. The topic for discussion was the CDC guidelines for chronic pain management, and I was scheduled to meet with someone who only dealt with acute pain management in cardiothoracic surgery.  Adding to my sense of foreboding was the knowledge that the prescriber had been singled out by her employer for this AD visit based on the number of opioid prescriptions she’d written. Using the communication strategies I learned at NaRCAD, I researched and prepared more for this visit than I had for any other. I practiced with multiple colleagues. On the day of my visit, I felt ready—but uncertain. My practice paid off. What began as a terse, somewhat tense conversation with the prescriber turned into an educational, productive, and collegial visit. I used my AD communication skills to dovetail from one question into another, ultimately discovering how my key messages resonated with the prescriber. I’m proud of the strides I made during that AD visit. I remained calm despite my anxiety, used my research on acute pain management to ask open-ended questions, translated what I know about chronic pain to support her in the acute pain setting, and laid the foundation for a strong, collaborative relationship. Best of all, I made a solid “ask.” I’m motivated to do it all over again with my next prescriber and take each learning opportunity as it comes. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation! Biography. Corinne is a clinical pharmacist at the University of Illinois at Chicago (UIC) College of Pharmacy. She uses her passion for drug information and advancing patient care in her role as a clinical instructor and academic detailer. Her areas of interest include hepatitis C, migraine, and diabetes pharmacotherapy, and new drug approvals. Corinne is a proud graduate of the UIC College of Pharmacy, Class of 2016. Her enthusiasm for science, health, and helping others prompted her to pursue a career in pharmacy. Before beginning her career in pharmacy, Corinne was a symphonic bassoonist and also worked as personnel manager for The Florida Orchestra. She graduated from the University of Iowa with a Bachelor of Music in 2001 and from Indiana University with a Masters in Music in 2006.
Academic Detailing to Address Substance Use in New Jersey: An “All-Hands-on-Deck” Approach11/30/2021
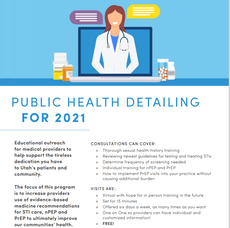
An interview with Clement Chen, PharmD, BCPS, Clinical Pharmacist Specialist, Rutgers New Jersey Medical School. by Anna Morgan, MPH, RN, PMP, Senior Manager, Training & Education, NaRCAD Tags: Substance Use, Detailing Visits, Evidence Based Medicine  Anna: Hi Clement! We can’t wait to hear about all the impactful work you’ve been doing in New Jersey. Tell us a little about your academic detailing program. Clement: The Northern New Jersey Medication-Assisted Treatment Center of Excellence was established in 2019 and is funded by the New Jersey Department of Human Services. Our goal is to not only increase access to medications for opioid use disorder (MOUD) in office-based addiction treatment practices, but also to ensure that providers treat this chronic disease with evidence-based practices. Our vision is to end the stigma of addiction and ensure that all people with substance use disorders have access to high quality care so they may live full and satisfied lives. I was hired as the academic detailer to provide education and identify the needs of providers in these practices. Anna: Tell me more about the types of providers you visit. Clement: I’ve been working with providers from all areas of care. In addition to office-based providers, they also include those from hospital settings, psychiatric hospitals, community health centers, substance use licensed facilities, and prison settings. Addressing the substance use crisis requires an “all-hands-on-deck” approach. Any setting where patients seek care are environments where detailing can improve patient access to support. Anna: It’s so important to approach academic detailing with a wider lens and consider where it can fit in with other community initiatives. Can you walk us through some of the work you’ve done so far, or are planning to do, in each of these settings? Clement: I’d be happy to!  Hospital Setting: One of the inner-city hospitals that we are working with is looking to establish an addiction medicine service within their hospital system. The goal is to provide trainings and consultations on best practices for addiction medicine, in addition to technical assistance in setting up a program. I’ll be working with their attending physicians and residents to provide evidence-based practice trainings. Another one of our partners, an addiction medicine provider, has been pushing for greater initiation of MOUD in her own hospital system. The main issue is to ensure that providers use MOUD in an evidence-based manner and adhere to the latest findings. For example, the provider has been receiving pushback from other providers due to the lack of referral sources. These providers have shared that they believe MOUD should not be initiated without a “warm handoff.” Furthermore, buprenorphine has been discontinued during the pre and peri-operative settings and only resumed post-operatively despite growing evidence for continuing buprenorphine in these settings. I plan to detail these providers in-person to provide literature supporting the use of MOUD, even when warm handoffs are unavailable. I’ve provided supporting literature and a summary to the addiction medicine provider to assist with her case to expand this initiative, which helped her to develop an information sheet to justify the expansion of MOUD in her hospital. Psychiatric Hospital Setting: We’ve also partnered with physician champions at some of the psychiatric hospitals in New Jersey. Stigma and the inaccurate idea that patients do not experience acute withdrawal for opioid use has made many providers hesitant to start therapy with buprenorphine. Psychiatric hospitals have been fervently looking to provide treatment for opioid use disorders. The goal is to implement a clinic designed for initiating and maintaining those on buprenorphine and naltrexone extended release. We’ll be assisting with the implementation of the clinic and provide individual in-person detailing visits for the providers at the hospital. To prepare for this, we’ve developed several informational sheets on MOUD and other related information to give to the providers.  Community Health Center Setting: One of the community health centers that we’ve partnered with wants to begin providing MOUD for those already on the therapy. There are several advanced nurse practitioners and physicians at the health centers looking for more guidance and support on the appropriate prescribing of buprenorphine. I’ll be working with their team to provide them with evidence-based practices and help them with buprenorphine induction strategies. Substance Use Licensed Facility Setting: One of the substance use licensed facilities I’ve consulted with mentioned that fentanyl has made initiation of buprenorphine very difficult due to the increase in the number of cases with precipitated withdrawal. As a detailer, I’ve worked closely with their lead providers, providing them with available literature on alternative buprenorphine induction strategies. They're in the process of updating their protocols for the induction of buprenorphine. Another facility is working with us to start prescribing MOUD within their residential settings. Prison Setting: I regularly consult with the Department of Corrections providers since access to MOUD have traditionally been low in the prison system. Their patients also have unique needs compared to those in the community setting. I meet with them on a monthly basis via a case conference and discuss clinical solutions in order to help them provide the best care to their patients.  Anna: Your work is incredibly comprehensive and thoughtful. It’s truly amazing to see how your team has incorporated academic detailing into so many initiatives and clinical settings within your community. Clement: We believe that to overcome this crisis, all patients with opioid use disorder need equitable and timely access to care. With the record number of overdose deaths reaching over 100,000 in one year, this is our greatest focus. We’re confident that our academic detailing work will help us achieve this goal. Have thoughts on our DETAILS Blog posts? You can head on over to our Discussion Forum to continue the conversation!  Biography. Dr. Clement Chen graduated from the Ernest Mario School of Pharmacy at Rutgers University in 2013 with his Pharm.D. He then completed a one-year residency at the Hudson Valley Veterans Affairs Ambulatory Care Clinic. Thereafter, he has worked as a staff pharmacist at St. Michael’s Medical Center in Newark and as a cardiology heart failure clinical pharmacist specialist at University Hospital in Newark. In addition to working as a clinical pharmacist specialist, he was a Transitions of Care pharmacist at Hunterdon Medical Center from 2016-2020. This has helped him to balance his inpatient and outpatient roles as a pharmacist. To further demonstrate proficiency in clinical pharmacy care, he received his Board Certification in Pharmacotherapy in July of 2016. His current role is as the academic detailer in the Northern NJ Center of Excellence, with the goal of providing education and support to increase statewide capacity to provide medications for addictions treatment (MAT) for patients with substance use disorders with a focus on opioid use disorder. Aanchal Gupta, NaRCAD Program Coordinator Tags: Conference, Detailing Visits, Stigma, E Detailing, Opioid Safety Take a peek at the NaRCAD2021 conference materials on our Conference Hub.  Fresh from our move to Boston Medical Center, our team at NaRCAD hosted the 9th annual International Conference on Academic Detailing, a virtual event concentrating on “Cultivating Relationships for Community Resilience.” There were robust discussions on critical topics, useful tools shared, and connections built. With over 300 registrants from across the globe, the AD community continues to learn and grow thanks to your support and passion for this work. Check out some of the highlights from our 2021 conference below. Day 1 + 2 Welcome Addresses
Field Presentations
Breakout Sessions
Expert Panels
Special Presentation: “Detailer Training in Action: Ask the Experts”
Real-time Roundtable
 Our team at NaRCAD is immensely grateful for your continued feedback and insights during our conference. This community has a wealth of knowledge to share, and as we approach 2022, we plan to continue to facilitate opportunities to connect you with others in the field, create a space to have conversations about stigma, and support your needs in the field. We look forward to seeing you in 2022. -The NaRCAD Team A special thank you to all of our NaRCAD2021 presenters! |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|