 Click the map to check out our partner programs. Click the map to check out our partner programs. Annual Conference, Off to Vegas for an HIV PrEP Training, & Our Team is Growing (and Hiring!) Tags: Conference, Training A letter from the staff at NaRCAD At NaRCAD, we're getting ready for our busy season, which lately, has become a season that lasts all year long. And we're happy for it--because that means we get to help more programs across the US and Canada figure out the most impactful ways to use academic detailing to promote sustainable change. Whether public health programs are looking to increase prescriptions of HIV PrEP for patients at high-risk, encourage more referrals to nutritionists for patients with diabetes, or improve access to treatment for people struggling with opioid use disorder, we're there to help them, from program conception to implementation and evaluation.  Improving HIV Prevention, one training at a time. Improving HIV Prevention, one training at a time. You may know that we offer bi-annual trainings here in Boston for health professionals to learn the techniques of academic detailing with our team of clinical outreach education experts through our 2-day, intensive, hands-on course. But did you know we also travel across the country to train teams on-site in their own communities? Through a partnership with the CDC, NACCHO, and previous funding from AHRQ, we've been on the road for countless successful trainings in early 2018, and we'll be wrapping up the year and heading into 2019 with a bang! Our next stop is Las Vegas, to work with the Southern Nevada Health District on improving outcomes around HIV prevention this December. (And for once, we hope that "what happens in Vegas" doesn't "stay in Vegas"; our goal is to increase visibility and prescribing of HIV PrEP so that more clinicians everywhere are reaching the patients who need it most.)  Click to see our latest agenda! Click to see our latest agenda! Prior to December, we'll be busy here on our home turf for the fall, holding our now-full Fall Training on October 1 + 2, and our fantastic, annual international conference on AD on November 12 & 13. We hope you'll keep your eyes out for dates for our Spring 2019 Training (which will be announced by November!) and that you'll join us for our conference--this year is our 6th annual, and we're excited to announce our full agenda is live on our Conference Series page. Register today--space is limited for this event!  And visit our blog often--we'll be featuring new interviews this fall, showcasing best practices on topics like reducing polypharmacy, reducing opioid prescribing in rural counties, and increasing lung cancer screenings. Want to be featured? Contact us and tell us what you're working on! Our team is ready to custom-tailor our support, so we can offer you the best ideas, resources, and tools to help your program thrive.  We can't wait to see you this fall! -The NaRCAD Home Team (PS: Want to join our team as a Program Manager? Send us your resume & cover letter.)
0 Comments
Director’s Letter: Mike Fischer, MD, MS 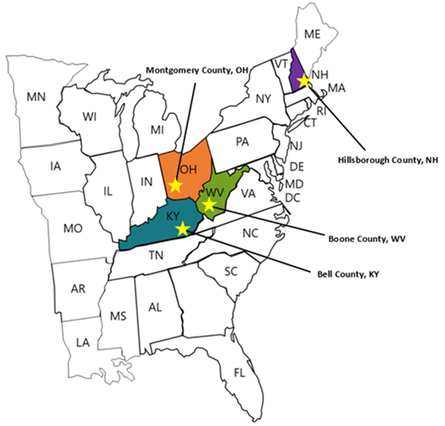 Tags: Director's Letter, LOOPR, Opioid Safety, Rural AD Programs, Training The opioid crisis has been recognized as a major national public health problem, but it actually reflects a collection of many thousands of local crises playing out in individual cities and counties. Each region faces a distinctive set of challenges, driven by economic and social factors, local medical practice patterns, political environment and pressures, and many other considerations. Identifying and implementing effective solutions to address the opioid crisis requires developing an understanding of how these individual challenges interact, and what strategies are most effective in specific situations--one of which is academic detailing.  The NaRCAD team is partnering with the CDC (Centers for Disease Control and Prevention) and NACCHO (the National Association of City and County Health Officials) on an exciting pilot program working with local health officials to develop customized interventions to reduce opioid overdose and death. Four sites experiencing significant public health problems related to opioids were selected: Boone County, Kentucky; Bell County, West Virginia; Manchester, New Hampshire; and Dayton, Ohio.  Public health officials at each site identified a wide range of local stakeholders to participate in developing a community action plan and recruited trainees to complete NaRCAD’s academic detailing training course, which we customized to address the unique challenges that each community faces. We also developed a specialized online toolkit for these sites, including discussion boards, local resources, and printable resources.  A trainee from Bell County, Kentucky, delivers a key message. A trainee from Bell County, Kentucky, delivers a key message. We traveled to each site in March and April of this year, facilitating hands-on trainings in the techniques of academic detailing in alignment with the CDC prescribing guidelines. Trainees came from diverse backgrounds, including pharmacists, nurses, public health officials, and students in the health professions, including pharmacy students, dental students, and medical school students. Plans for implementing AD varied by site depending on the local health care environment; some sites focused more heavily on appropriate prescribing of opioids by clinicians, while others prioritized increasing referral rates for patients with opioid use disorder (OUD), including access to medication-assisted treatment (MAT).  Practicing a concise introduction in Manchester, New Hampshire. Practicing a concise introduction in Manchester, New Hampshire. As the AD trainees at each pilot site continue their work in the field, we’ll learn more about how these diverse strategies succeed, and how we can support adaptations to make academic detailing more impactful. This important collaboration has allowed us to form invaluable partnerships with CDC and NACCHO, leveraging national resources to improve local responses to this epidemic through plans that respond more precisely to local needs and priorities. We’re excited for this pilot program to serve as a model for future opioid safety AD interventions, and we’ll be providing updates here on the blog. In the meantime, tell us: what's happening in your local community around the opioid crisis? Sound off in the comments section below, and let us know if you think clinician-facing education could be a strategy that would improve outcomes for your community. And join us for our next training and our terrific annual conference to learn more about this and other exciting AD projects. -Mike  Biography. Michael Fischer, MD, MS | Director of NaRCAD Dr. Fischer is a general internist, pharmacoepidemiologist, and health services researcher. He is an Associate Professor of Medicine at Harvard and a clinically active primary care physician and educator at Brigham & Women’s Hospital. With extensive experience in designing and evaluating interventions to improve medication use, he has published numerous studies demonstrating potential gains from improved prescribing. Read more.  Guest Blogger: Monica Mais, MSN, FNP Family Nurse Practioner/Academic Detailer California Opioid Safety Network, Fairchild Medical Clinic NaRCAD Training Alumnus Tags: Detailing Visits, Opioid Safety, Rural AD Programs, Training In 2011, I went from 15 years as an Emergency Room nurse to a new role as a Family Nurse Practitioner in a rural healthcare setting. I couldn’t believe the amounts of prescribed opioids that were coming out of our little clinic—the average chronic pain patient was receiving 240 Morphine Equivalents/day (MEDs), and many of these patients had been receiving these medications for years without oversight. In 2013 I introduced an evidence-based protocol and policy for safe prescribing of Opiates for Chronic Non-Cancer Pain (CNCP).
However, patients who could not obtain opiates from our clinic quickly moved on to the clinic across town. This influx of opiate seeking patients was reason for concern from those receiving clinics. My colleagues and I opened our doors to neighboring clinics and providers and began sharing our policies and successes. Many other area clinics started adapting our policies to their own practice, reducing their opiate prescribing as well.  We formed a coalition called Siskiyou Against Rx Abuse (SARA), and based on our previous successes, we were all shocked to see data showing our county was among the highest opioid prescriptions per capita in California, and had a high overdose rate per capita, despite our efforts. Clearly, more needed to be done! Our coalition facilitator, Maggie Shepard, RN, along with our medical director, Dr. Sam Rabinowitz, and myself were all invited to attend training to become Academic Detailers in San Francisco with the San Francisco Department of Public Health, a partner with NaRCAD, the National Resource Center for Academic Detailing. We did scripting and role-playing throughout the training, learning the important social marketing and communication skills needed to conduct a personalized visit with a provider where the goal would be to change behaviors to continue to promote safe opioid prescribing, Naloxone, and Buprenorphine out to providers in our area. During the training, I was videotaped during a practice role-play, which was very helpful, as it reminded me to speak more slowly, and to organize my key messages and talking points. After the training, getting our detailing program into the field involved a step-by-step process. Here are important things to consider that have worked well for my detailing process:
I plan to continue AD throughout 2018. I believe we have experiences that we can share to encourage our colleagues to make positive changes in in their prescribing habits. Academic Detailing works due to mutual respect of one another’s experiences, professionalism, and willingness to receive new information—it’s an excellent way to foster change within a system! Biography
Monica Mais, MSN, FNP Family Nurse Practioner/Academic Detailer, Fairchild Medical Clinic Monica Mais is a Board Certified Family Nurse Practitioner working at an FQHC in Siskiyou County, located in far Northern California on the Oregon border. She is a founding member of Siskiyou Against Rx Abuse, member of the California Opioid Safety Network and an X-Waived prescriber, working with chronic pain and opioid dependent patients. As a former Emergency Room Nurse for 15 years, many of Monica’s shifts involved witnessing overdoses, drug-seeking behavior, violence, desperation, and healthcare worker burnout. It had been escalating every year to its current crisis level, and Monica wanted to be part of the solution to this heartbreaking epidemic. Questions on this piece for Monica Mais? Contact her at mmais@fairchildmed.org, or leave your thoughts in the discussion forum below.  As the Public Health Education Specialist for the WIC (Women, Infants & Children) program and the Opioid Task Force in Butte County, California, Stacy Piper, CLEC, acts as a regional liaison with the medical community as well as coalition's and various community partners. Learn more about Stacy in the bio at the end of this piece. Tags: Detailing Visits, Opioid Safety, Substance Use, Training NaRCAD: Hi, Stacy! Thanks for joining us. Tell us a little bit about your work—we understand you, like many folks in public health, wear multiple hats. As the Butte County Public Health Education Specialist for the WIC (Women, Infants & Children) program and the Opioid Task Force in Butte County, I act as a liaison with the medical community. I collaborate with hospitals, health care providers, public health programs, and community organizations to improve public health and continuity of care. 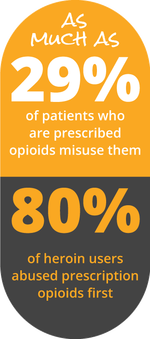 NaRCAD: Talk to us about detailing for the opioid crisis—you do this 1/4th of your time. How did you get started? After providing educational detailing for the WIC Program funded at 30 hours a week, I was asked to be an Opioid Academic Detailer for Butte County. In preparation, I attended the Academic Detailer Training in San Francisco. The training provided by the CA Health Department, San Francisco Public Health Department's Substance Use Research Unit, and NaRCAD was one of the finest training experiences - even after the countless hours of extremely comprehensive training I received in the Pharmaceutical Industry. Regarding impact on a local level, it is indescribable how every interaction with a healthcare provider is beneficial. Academic Detailing (AD) is an equal exchange of information. I consider it a huge responsibility, and a privilege, to be an educator for doctors and medical professionals. I prefer the word “educator” instead of “detailer” because I have concerns that a “detailer” may be initially viewed as a salesperson. I love and respect that AD is not driven by attempting to influence medical professionals for personal gain. It’s all about helping providers improve health outcomes in patients with the entire focus of the conversation about the real people in their practice that need help.  NaRCAD: Tell us a little about your background in pharma, and how this translates to your detailing work now. I was a Senior Executive Pharmaceutical Sales Representative for 15 years in Northern California, advocating for immunizations and promoting various prescription drugs. This provided first-hand experience of the astonishing evolution in the Medical, Pharmacy, and Insurance industries. Understanding the basic dynamics of medical offices has helped me navigate and gain access at a quicker pace for AD. Also, understanding the business acumen component of running a medical practice has proven to be valuable in my recent interactions.  NaRCAD: You mentioned that you’re committed to providing value for clinicians and patients alike. Talk to us about how you share key messages with the clinicians you visit. In my experience, to truly influence the behavior of a highly-educated and experienced individual, you must come to the table with the goal of learning. With attentive listening, you ‘hear’ the medical professional, and process what you have learned. Your intuition will guide you to ask the appropriate, insightful questions needed to evaluate his/her priorities and challenges. This is a beautiful thing, because trust starts to blossom and the partnership has begun. You can then confidently tailor key messages, valuable resources and solutions that are closely tied to those needs and challenges you uncovered. You should begin to see the individual’s genuine desire to truly change behavior and habits.  NaRCAD: Talking about opioids is a sensitive topic. What’s some of the typical pushback you get from clinicians you detail about opioid safety? The response to academic detailing really depends on the situation and the type of clinician and/or establishment I am working with. Sharing local opioid statistics compared to our state statistics is an eye opener! I try to paint real life pictures by telling true stories. For example, I’m honest about my own family members who were innocently caught up in this crisis, including the true story about the day my sister’s husband accidentally took his prescribed opioid medication twice. My sister lost her husband that day.  NaRCAD: Along with telling true stories, how do you handle pushback and stay positive, encouraging clinicians to pivot? Time, or lack of time, is the biggest culprit in keeping physicians from attempting to personally assist in ending the addiction cycle for patients. I passionately believe clinicians need more time with people on opioids. It takes several visits with an office to start moving in the right direction. Working with the medical assistants, nurses, and/ office managers is a key component. They can often have influence, give advice or insight, and even advocate when you are not there. Also, I review our county’s Safe Prescribing Guidelines. If clinicians cannot institute all items in the guidelines, I ask providers to choose what they can commit to doing and to think about some specific patients they can work with. I also ask them to consider prescribing Naloxone for patients on high doses of opioids (above 50 morphine milligram equivalents).  NaRCAD: What would you share with new detailers who are about to go into the field and use AD to tackle the opioid crisis? I have a few reminders and tips for detailers:
Biography.
Stacy M. Piper, CLEC, Public Health Educational Specialist Butte County California Public Health Department As a Public Health Education Specialist, Stacy was chosen to work with two CA State grant funded programs educating Medical Professionals, Hospitals and Community Organizations for the WIC Program and the Opioid Drug Abuse Prevention Program. She maintains an active involvement with the Butte County Opioid Task Force, as well as the Butte County Drug Addiction Prevention Coalition, ACE’s Coalition (Trauma Informed), Breastfeeding Roundtable Coalition, Butte County Breastfeeding Coalition, Mother Strong Coalition, and Perinatal Coalition. Stacy has had extensive training with the California Department of Public Health's Opioid Stewardship & Chronic Pain Detailing Program, ID Training, UCSD CLE (Certified Lactation Educator), Coalition & Equity Training, Advocacy Training and holds 14 years of ongoing training & certification in the Pharmaceutical Industry. She is a member of the team coordinating and orchestrating the 2018 Northern California Opioid Summit.  Tags: Detailing Visits, HIV/AIDS, LOOPR, Opioid Safety, Training We've been staying busy here at NaRCAD this spring! With public health challenges like the opioid crisis, and the continued need for HIV prevention, the team here at NaRCAD has been on the road for 5 trainings in 6 weeks, and we're not stopping yet! On February 14th - 16th, 2018, NaRCAD joined the amazing teams at San Francisco Department of Public Health and the New York City Department of Health and Mental Hygiene for an exciting initiative: A Public Health Detailing Institute on HIV PrEP and RAPID. Hosted in San Francisco's South Market neighborhood, 31 trainees attended, representing diverse public health departments from Texas, Connecticut, Alaska, Louisiana, Florida, Tennessee, Los Angeles, San Francisco, Mississippi, Michigan, Oregon, Nevada, Virginia, and beyond. These trainees joined the institute for a customized, 3-day event focusing on learning the techniques of academic detailing, along with showcasing best practices and success stories via special presentations and expert panels. 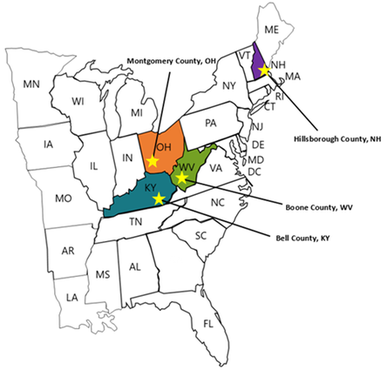 This past month, from March 7th through April 4th, 2018, NaRCAD hit the road four more times, as part of an exciting 4-site pilot project in partnership with our terrific colleagues at the CDC (Center for Disease Control) and NACCHO (The National Association of County and City Health Officials). Upon identifying counties and cities with the highest burden of fatal and non-fatal opioid overdose and high prescribing rates, the CDC selected Bell County, Kentucky; Boone County, West Virginia; Manchester, New Hampshire; and Dayton, Ohio as 4 pilot sites in which to convene with key community stakeholders and roll out community action plans, along with targeted academic detailing interventions.  Our work has involved launching on-location trainings at each of these pilot sites, focusing on providing front line clinicians with tools and support to improve outcomes for patients. Messaging and support for these campaigns include lowering prescribing rates, referring patients to treatment for opioid use disorder (OUD) including Medication Assisted Training (MAT), and using their state's PDMP (Prescription Drug Monitoring Program) to identify troubling patterns of use, which may, in turn, help to identify those patients who need more support and care.  Trainees at each site of these pilot sites work with us across two days to learn the structure of an academic detailing visit, practice role playing 1:1 visits with clinicians, and become experts at using educational materials (including a suite of materials constructed by the CDC based on their 2016 Opioid Prescribing Guidelines). Our pilot site trainees walk away from our trainings ready to actively engage with clinicians to assess individual needs and provide customized support, and encourage behavior change for the opioid crisis in their respective communities.  NaRCAD's team will continue to focus on launching new academic detailing interventions across the U.S. well into 2018, with upcoming opioid-specific trainings being carried out in late May in Albuquerque, New Mexico, with the University of New Mexico's Health Sciences Center, and in late June in Lansing, Michigan, with the Michigan Public Health Institute.  Our next all-topic, AD techniques training in Boston will kick off at the end of this month, where we'll train 24 health professionals from across the U.S.--we'll report back after that training and share lessons learned, highlights, slide decks, and clinical topics from represented programs, and we look forward to sharing those with our community. Join our subscription list to receive alerts for upcoming training opportunities. Want to customize a clinical topic-specific training for 15 trainees or more, on site in your community? Reach out to us to schedule a training consultation call at narcad@partners.org. We can't wait to work with you! -The NaRCAD Team This press release originally appeared on publicnow.com and was written by UCSOP. Tags: LOOPR, Opioid Safety, Rural AD Programs, Substance Use, Training The University of Charleston School of Pharmacy (UCSOP) is partnering with the Centers for Disease Control and Prevention (CDC) to pilot the National Resource Center for Academic Detailing (NaRCAD) program at the Boone County Health Department in Southern West Virginia. Academic detailing is a one-on-one outreach education technique which allows pharmacists, pharmacy students and other health care professionals to educate prescribers on the dangers of overprescribing opioids and also recognize the signs of opioid abuse.  UCSOP participants include student pharmacists Angela Withrow (class of 2019), Amy Bateman (class of 2018), Joshua McIntyre (class of 2021), Jami Swift (class of 2021), and assistant professor Dr. Sarah Embrey. These individuals make up five of the seven selected persons being trained for the program. A two-day training will kick-off the program on March 14-15, 2018. 'Participation in this important pilot project is just one more way UCSOP students and faculty work to educate and serve communities throughout West Virginia on opioid use/abuse by sharing best prescribing practices, delivering prevention education, and encouraging recovery and treatment,' said Dr. Susan Gardner Bissett, Assistant Dean for Professional and Student Affairs. 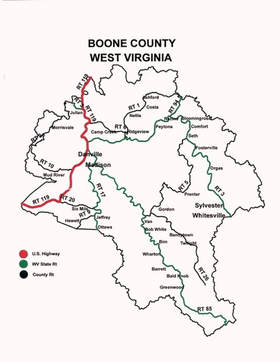 NaRCAD was founded in 2010 and is a national resource center that supports clinical outreach education programs across the United States. The goal through its trainings and program support is for clinical educators to have a greater impact when visiting clinicians and aiding those clinicians on making evidence-based decisions. Interventions supported include reducing opioid abuse, HIV/STI screening and prevention, prenatal health, smoking cessation, chronic disease management, and more. For more information, visit https://www.narcad.org/.  Tags: Conference, Training We’re noticing a pattern over here at NaRCAD. As we enter into our 8th(!) year as the only resource center dedicated to clinical outreach education, we’re proud of the recent work we’ve done together with our community, as we are every year. But the pattern we’re seeing is about much more than just pride. With each January that rolls around, we’re invigorated by the energy of our community members, and by the important programming that's taking place across North America. So it’s no surprise to us that we’re consistently excited to greet each year with the creative solutions, expertise, and events you need to make your program thrive. This year, some of those creative solutions are ready for you to take for a test drive. We’ve just launched our CoRE (Clinical Outreach Education) Podcast Series, featuring 20 minute episodes of insight, and innovation. (Listen to our pilot episode here, and suggest topics you’d like to hear in the comment section below.) We’re also proud to release our brand new Detailing Directory, highlighting shareable resources from successful field programs across the US and Canada. Explore the Detailing Directory by clinical topic, and explore our AD Fact Sheets, featuring toolkit examples, publications, and video sessions on specific topics in academic detailing. The goal of our Detailing Directory is to give you direct access to resources and building blocks to strengthen your program so you don’t have to reinvent the wheel. (Want to be featured and share your resources? Contact us today and we’ll be happy to add you to our directory.)  And while we’re proud of our ever-growing portfolio of virtual resources, what we love most is to connect with you person to person, program to program. That’s why we’re delighted to announce the dates (and open registration!) for our upcoming Spring Training on AD Techniques in Boston on April 30 & May 1st, 2018. We’ve also just released our Save the Date for our 6th annual International Conference on Academic Detailing on November 12th & 13th, 2018—and we’re taking submissions for presentations starting March 1st--we hope you'll consider applying! With so much happening for NaRCAD, and for our dedicated community members, who work tirelessly to improve patient care through clinician education, it's easy to see why we’re looking forward to the opportunities ahead. Thanks for continuing to share your insights with us--we’re here to support you, highlight your work, and ensure that your programming has the greatest possible impact.
We hope to connect with you soon. -The NaRCAD Team Year One of Colorado Department of Public Health & Environment’s Detailing Program Guest Blogger: Deborah Monaghan, MD Public Health/Academic Detailer Colorado Department of Public Health and Environment NaRCAD Training Alumnus Tags: As the first and only detailer hired by the Colorado Department of Public Health and Environment, which serves 5.6 million people (about 3 million of which cluster around one metro area), the idea of building a detailing program from the ground up was incredibly exciting…and daunting. From the outset, it was important to determine the place of detailing within the community and establish its fit in the department’s mission. Shortly after joining the team, I presented the intended scope of my work at a department meeting--and it generated tremendous interest in the use of academic detailing for public health initiatives far beyond the current planned intervention. This served to solidify the potential value of clinical education outreach to leadership throughout the department. Lessons learned are continually surfacing as we move into year two, and a few key concepts are worth sharing. 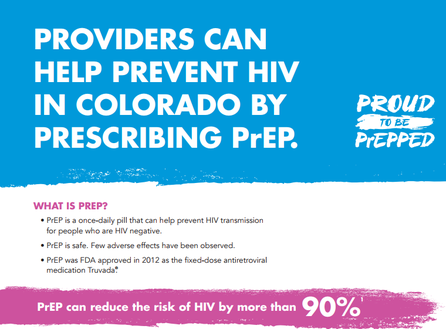 Particularly in the early stages of program establishment, it was essential to stretch resources and leverage partnerships. NaRCAD connections with other detailing programs facilitated the exchange of print resources, protocols and lessons learned, saving valuable development time. Through CDC-funded capacity building visits, I shadowed detailing teams at two other health departments' AD programs (San Francisco Department of Public Health and the New York City Department of Health & Mental Hygiene), which provided a framework for our own program’s function. At every opportunity, I presented our detailing goals to community partners and stakeholders, resulting in many connections to medical providers, which, in turn, generated most of our initial provider visits. Submitting articles for local clinical practice newsletters and magazines also established recognition and trust in the state’s new detailing initiatives.  Once provider-facing detailing visits began, two things became quite clear: Providers crave connection to their public health department. Providers want regional data. In a state with both urban and rural/frontier areas, urban clinicians wanted to be seen as “boots on the ground” to impact large populations by treating their own patients, while rural providers wanted to be acknowledged as part of the team and directed to resources they could access remotely. All clinicians, both urban and rural, wanted the latest disease and health data for their county, zip code, and even census tract level to compare to the rest of the state. It has taken multiple attempts to get in the door in many practices. However, after a detailing visit, most providers are outspoken that they found the session worthwhile, and we've used this opportunity to ask for referrals to other providers who might be open to visits. The time investment has also enabled two-way communication allowing us to get a “finger on the pulse” of regional health and disease, particularly in the more rural areas. The initial time invested to establish relationships with providers was high, but the rate of return has justified the investment. With a new detailing program, the responsibility falls to the detailer to establish credibility, both in resources provided as well as in value for time spent.  If I were starting a detailing program again, or could support new programs who were just getting started, I would love to be armed with these lessons learned: Establish as many protocols, procedures and resources as possible. Just start! Even if every detail isn’t in place, start visiting with providers. (The steep learning curve of on-the-ground visits is incredibly valuable and will continue to shape and improve your methods.) Document everything! As methods change and processes improve, document what is changing and why. Document with the goal of sharing not simply a starting point and a finished product but an entire story. Be willing to adjust in real time. Providers will have varying needs from one to another and from one day to the next, and our flexibility will ultimately strengthen the relationships we are trying to build, allowing academic detailing to have the greatest possible impact. Biography.
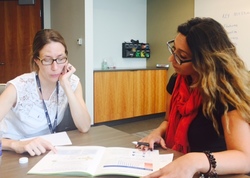
Deborah Monaghan, MD Public Health/Academic Detailer, Colorado Department of Public Health and Environment Deborah joined CDPHE in 2016 as the Department’s first detailer and currently provides clinical outreach on HIV prevention and sexual health. A graduate of the University of Mississippi School of Medicine, internship took Deborah to Drexel University in Philadelphia, Pennsylvania followed by residency at St Mary’s Hospital in Grand Junction, Colorado. She will complete her MSPH through the University of London School of Hygiene and Tropical Medicine in 2018. Initial response from the provider community receiving detailing has been overwhelmingly positive, and Deborah hopes to facilitate expansion of detailing efforts into other branches of public health to impact more Coloradans.  Tags: Conference, Training Here at NaRCAD, we're excited for our favorite (and busiest) time of year. We were on the road in San Francisco this month, working with the Pacific Aids Education & Training Center to run an HIV/PrEP-specific academic detailing techniques training. Now, we're gearing up for our annual Fall AD Training that we hold each September in Boston, focusing solely on teaching the social marketing techniques of clinical outreach education--our class is full, but we'll announce a new one soon!  What's next? Our 5th International Conference on Academic Detailing, with an exciting 2-day agenda lined up for this November 6th & 7th, 2017! If you haven't registered yet, take a look at our event page and contact us with any questions. We'll be posting our agenda soon, including terrific keynote speakers, as well as an emphasis on the critical clinical topics that our field is grappling with.  We won't slow down after that--in December, we're off to Madison, Wisconsin to facilitate another customized training session, this time supporting the CDC-funded Public Health Department of Madison and Dane County, working together to use academic detailing as a strategy to combat the opioid epidemic.  As we look to end 2017 with a bang, we don't want to miss a thing--tell us what you're up to and what resources you need to take your programming to the next level. Whether it's a refresher course, a strategy session via teleconference, connections with other programs, or new materials, we're here to help make your program more effective. Hope to see you over the next three months! -The NaRCAD Team  Bevin K. Shagoury, NaRCAD Communications Director Tags: Detailing Visits, Evidence-Based Medicine, Training We're getting ready for our September 2017 training course, and our waiting list is already packed with health professionals who are eager to learn the techniques of academic detailing. So, what's our 2-day training class all about? First, some background on why academic detailing ("AD") is a critical tool in healthcare improvement. AD, or "clinical outreach education", is a unique clinical outreach education strategy where a trained health professional visits a frontline clinician, providing custom-tailored, 1:1, interactive service to that clinician in order to share best evidence and promote specific behavior changes.  In a 1:1 clinician visit, best evidence is shared to promote changes in care across clinical topics and strategies, including anything from shifts in patient prescribing (e.g., to prescribe fewer antibiotics, or switch to a more effective statin) to increases in use of screening and prevention tools (e.g., using a new tool to assess fall risk for seniors, or increase colon cancer screening for a specific demographic.) But knowing the best evidence is only half the battle. Effective academic detailers must learn how to truly connect with a busy clinician, figure out quickly and accurately what that clinician needs to support his or her practice, and deliver information in a dynamic, engaging, and clinician-centric way. "AD" is never a lecture, nor is it simply a delivery of glossy printouts. It's a personalized service used to actively engage busy front line clinicians, and the only way to learn how to deliver that service is to practice doing it. We teach our trainees to prepare for inevitable pushback and artfully deliver critical information that a front line clinician needs in order to provide the best care.
 Over 300 of our trainees have completed our 2-day course ready to visit practices, build trusting relationships with front-line clinicians, skillfully share best evidence, and successfully implement effective health interventions. If you're thinking about attending but would like to know more, please drop us an e-mail and our team will be happy to discuss this unique training experience. You can also check out testimonials from previous trainees here. Ready to register? Just visit our training series page after July 1st, 2017, and save yourself a spot at our September 2017 session.  Director's Letter | Mike Fischer, MD, MS Tags: Conference, Director's Letter, Health Policy, Training The entire health care system is grappling with uncertainty. What will happen to the provisions of the Affordable Care Act? Will clinicians and health systems face major changes in how they are expected to provide care and how they are reimbursed? Will state and local public health agencies have support for the many initiatives undertaken in recent years? As we wait for answers to these questions, the role of academic detailing is more important than ever. AD programs will face new challenges, and will need to understand how AD can be adapted to fit changing constraints and still have a beneficial impact on clinician engagement, the quality of care, and patient outcomes. At NaRCAD, we look at this unpredictable environment and see a mandate to collaborate and innovate, working with our partners to develop and evaluate novel ways to implement AD.  At NaRCAD, we look at this unpredictable environment and see a mandate to collaborate and innovate. Planning for NaRCAD2017, our annual conference, is well underway, and the call for proposals is open. Submit results of your current work or your ideas for panels and breakout sessions that will let you share your work and inspire colleagues.  To keep AD growing and thriving requires an active pipeline of newly trained detailers, which we have just added to with our recent AD Techniques Training on March 30 & 31, 2017. This spring’s training class came to Boston to learn the techniques of academic detailing in order to support important interventions, including better use of smoking cessation treatment for patients with serious mental illness, increasing HPV vaccination rates, enhanced safety of opioid prescribing, and improving the care of chronic diseases such as COPD, HIV/AIDS, diabetes, heart failure, and kidney disease. Our trainees hailed from Canada, Brazil, and around the U.S., including South Carolina, Rhode Island, Idaho, Massachusetts, Oregon, Texas, Kentucky, Connecticut, and Colorado, bringing their unique experiences and backgrounds to 2 days filled with hands-on learning opportunities. Stay tuned for upcoming details about our Fall 2017 training, to be held this September--dates announced soon! What continues to motivate us during times of uncertainty is working with the NaRCAD community, and we want 2017 to continue to be a year of even deeper engagement. Submit to the 2017 conference, share your ideas, suggestions, and comments on our blog, or reach out to us directly. We’re excited to continue to support your work and to build new collaborations--tell us what you need as part of our community of clinical outreach educators. -Mike Biography. Michael Fischer, MD, MS, NaRCAD Director
Dr. Fischer is a general internist, pharmacoepidemiologist, and health services researcher. He is an Associate Professor of Medicine at Harvard and a clinically active primary care physician and educator at Brigham & Women’s Hospital. With extensive experience in designing and evaluating interventions to improve medication use, he has published numerous studies demonstrating potential gains from improved prescribing. Read more. Mike Fischer, MD, MS, Director of NaRCAD | January 2017 Director's Letter Tags: Conference, Director's Letter, Training Growth. Support. Engagement. These words characterized 2016 for NaRCAD, and have us planning for an exciting 2017. In 2016, we had our most successful and impactful year to date. Our community has grown to over 1000 national and international supporters of clinical outreach education.  At #NaRCAD2016, our 4th annual conference on academic detailing, the agenda reflected what’s happening in the field, composed largely of ideas and presentations submitted by you, the members of our network. Keep your eyes open for our Call for Presentations on our NaRCAD Conference Series page— #NaRCAD2017 will be held here in Boston on November 6th & 7th, 2017 and applications for presentations will be accepted starting March 1st. After this past year’s success, we’re even more committed to providing customized support to individuals, groups, and large organizations working on clinical outreach education.  In addition to our core training sessions in Boston (our next session is March 30th & 31st), we’re continuing to offer on-site topic-specific trainings, customized workshops, and special educational sessions on the principles and practice of AD. In addition to providing direct support, we’ve been excited to successfully connect people and programs with each other, allowing for the exchange of ideas and best practices among both national and international experts. We’re proud of our ability to meet our partners where they are, whether they’re starting, expanding, or adapting AD interventions, and this year, we’re looking forward to supporting and improving your work.  We started this process by sending you our first annual community survey in December, and we thank our many members who responded. (You can still weigh in if you have thoughts, although our raffle is over!) We’ve listened to your insightful suggestions, and we’re already taking action to support your needs. This year, we’ll be launching the new COrE (Clinical Outreach Education) Series, exploring AD program development, specific clinical content, and other topics you’ve suggested. Featuring AD experts, the NaRCAD team, and using both interview and live webinar formats, the COrE Series is a great opportunity for advanced learning, support, and collaboration. Stay tuned for more information! We’ll also be increasing engagement opportunities via our Partner Network; we’ll be reaching out individually to learn more about your current work, and we’ll offer an interactive site where you can make your own partner connections with experts working on similar topics. As we grow even more in the coming year, your ideas and reflections remain invaluable. You don’t have to wait for us to contact you! We invite you to be in touch with our team and tell us more about your program—what challenges you’ve faced, what successes you’ve experienced, best practices you’d like to share, programs you’d like to know more about, and the resources you need to help you succeed. -Mike  Biography. Michael Fischer, MD, MS, NaRCAD Director Dr. Fischer is a general internist, pharmacoepidemiologist, and health services researcher. He is an Associate Professor of Medicine at Harvard and a clinically active primary care physician and educator at Brigham & Women’s Hospital. With extensive experience in designing and evaluating interventions to improve medication use, he has published numerous studies demonstrating potential gains from improved prescribing. Read more. Director’s Letter: Fall 2016 | Mike Fischer, MD, MS, Director of NaRCAD Tags: Conference, Detailing Visits, Director's Letter, Training When the leaves start to turn here in Boston, we know it’s almost time for NaRCAD’s International Conference on Academic Detailing. This year’s 4th annual conference features several new and exciting sessions we’re excited to share with our community. #NaRCAD2016 highlights the work of innovators in academic detailing from many locations and organizations, ranging from large national health systems to small independent programs.  Diverse clinical topics will be featured at our interactive sessions, including pediatric developmental screening, smoking cessation in patients with serious mental illness, opioid misuse and overuse, screening for ADHD, and many others. Breakout sessions offer attendees a chance to work closely with leaders in the field, featuring in-depth and hands-on exploration of specific elements of academic detailing. Whether your focus is on training detailers, preparing clinical topic materials, or program evaluation, our dynamic breakout sessions offer a chance to network and acquire new skills.  Our conference is our largest event of the year, but our team has been busy this fall with other activities. At our Boston-based training in September we welcomed trainees from organizations across the country, all of whom concentrated on learning the techniques of academic detailing. We also spent two days this fall in San Francisco, working with the city’s Department of Public Health on an intervention to increase the use of pre-exposure prophylaxis (PrEP) for patients at risk of contracting HIV. We’re excited to continue supporting our partners at the SFDPH as they move forward on this important initiative.  Come join us at #NaRCAD2016! There’s only a month left to register, and space is limited. Check out our conference hub archival page to see what previous events were like, including on-demand video and program highlights. We’re excited that clinical outreach education has been such an effective strategy to address the pressing problems facing patients, clinicians, and health systems. This year, we know that the opportunity to learn, share ideas, and connect with experts will continue to ignite inspiration for our community’s important work in improving quality of care and patient outcomes in 2017 and beyond.  Biography. Michael Fischer, MD, MS | Director, NaRCAD Dr. Fischer is a general internist, pharmacoepidemiologist, and health services researcher. He is an Associate Professor of Medicine at Harvard and a clinically active primary care physician and educator at Brigham & Women’s Hospital. With extensive experience in designing and evaluating interventions to improve medication use, he has published numerous studies demonstrating potential gains from improved prescribing. Read more.  Bevin K. Shagoury, Communications & Education Director Tags: Conference, Training After another terrific 2-day Academic Detailing Training course here in Boston, it's easy to see how each new training class brings its own unique energy and important clinical interventions to the table. On September 19th and 20th, 2016, trainees from nearly every corner of the U.S. map joined us to learn the core, social marketing techniques of successful clinical outreach education.
 While each training has its own unique group discussions and trainees, our 2-day course always includes presentations on the evidence base and history behind academic detailing, the best ways to evaluate evidence for your intervention, the foundation of behavior change theory for academic detailing, how to use educational materials in an effective way. We lead interactive discussions, group activities, breakout role-plays, and for each training class, we customize a session encouraging the class to use the virtual resources on our Learning Center.  We hope you'll join us at a future training, and please join us for our upcoming conference this November, an exciting opportunity to engage in hands-on workshops, learn about best practices from experts in the field, and meet others doing similarly important work. Stay tuned for an upcoming announcement of dates for our Spring 2017 training course--registration will open in January 2017. Learn more about our amazing staff and facilitator team, and explore our blog's interviews and events recaps to see how NaRCAD supports and highlights health education professional who are using academic detailing to improve health outcomes, one educational visit at a time.  Biography. Bevin Kathleen Shagoury | Communications & Education Director Bevin manages NaRCAD’s external communications, working to magnify the impact of clinical education programs via strategic partnership development, best practices highlighting, and access to virtual learning platforms. Read more. NaRCAD's Interview Series: Public Health Detailing Program at New York City Department of Health and Mental Hygiene (DOHMH) Featuring Michelle Dresser, MPH, Senior Manager, Programming & Strategy Tags: Detailing Visits, Diabetes, Evaluation, Obesity, Program Management, Smoking Cessation, Training  Thanks for taking the time to share the great clinical outreach education work that’s being done by the NYC Department of Health and Mental Hygiene, Michelle! Tell us a bit about yourself and how you got involved in public health, specifically public health detailing. Michelle: Thank you for the opportunity to speak about the Public Health Detailing Program. I have over 20 years of public health experience in both the non-profit and government setting, with the last 12 here at the New York City DOHMH. Throughout my professional career, my specialty has been in healthcare marketing and provider education, emphasizing how providers and consumers can better communicate with each other by tailoring complex messages using health literacy principles.
 An excerpt from DOHMH's obesity pocket guide. An excerpt from DOHMH's obesity pocket guide. It’s essential our reps have excellent selling and communications skills, so when they engage providers and get their buy-in, providers are then equipped to get their patients “on board”. One-on-one provider engagement helps them understand how important it is to have a 2-way communication with patients. How can an outreach representative encourage providers to “get on board” and think about care as a dialogue? Michelle: Let’s use obesity as an example. With obesity, both providers and patients are frustrated, for different reasons. Providers may be frustrated that patients’ comorbid conditions are being exacerbated or don’t have the same kinds of tools to treat obesity as they do other conditions; patients might feel that providers aren’t using great communication techniques, like motivational interviewing (MI), to help them set goals and take small steps towards the goal. If a patient is only told, “You need to lose weight,” which is such a broad and overarching goal, they’ll be frustrated, and frankly, non-adherent. I know I would be.  Example of a coaching script created by DOHMH. Click to learn more. Example of a coaching script created by DOHMH. Click to learn more. Encouraging providers to have specific dialogues using a customized approach for each patient is important. This kind of dialogue takes into account patients’ literacy beyond the written and spoken word—it looks at scientific, fundamental, health and cultural literacy, too. We work on “coaching scripts”, which take the key recommendations and reframes them in order to custom-tailor the conversation for each patient.
One thing that’s unique about public health detailing is that we detail the whole team through one-on-one interactions. Evidence shows these types of interactions with providers and staff are more effective at changing behavior; however, sometimes due to the makeup of the practice we must conduct group presentations. It’s not ideal, but it still allows us to get the messages and materials out there.
 A coaching guide designed by the NYC DOHMH to aid clinicians in smoking cessation support for patients. A coaching guide designed by the NYC DOHMH to aid clinicians in smoking cessation support for patients. So when an outreach representative goes into an office, they detail...everyone? Michelle: If there are 15 people who work in an office, we’re going to detail all 15 of them. It’s a lot! Sometimes, the person who is the champion of a new behavior or workflow isn’t going to be the provider. We see the front desk staff as instrumental; they’re interacting with all of the patients. We work with our teams to ensure even the front desk staff receives the materials and information, rather than seeing them merely as a “gatekeeper” to get to the providers. Sounds like a lot of training goes into preparing for your campaigns, and for thinking about the entire process of effective outreach. Tell us more about your trainings, and about how you prepare outreach representatives on disease content training, as well as in marketing and communications skills.  Click to view more Public Health Action Kits (copyright of NYC's DOHMH) Click to view more Public Health Action Kits (copyright of NYC's DOHMH) Michelle: On average, our trainings are about 5 days in length and take place the week prior to launching a new campaign. About 40 percent of the training is disease content, so we work with our internal Health Department experts, as well as external experts, where we learn about prevention strategies, treatment strategies, epidemiology and the landscape around the key recommendations chosen based on the evidence of that topic. We need to know the ‘why’ behind the campaign. Once we have that under our belt, we shift to sessions on how to frame the issue, how to promote the materials, figuring out the “features and benefits” as well as the “barriers and objections” and finally “gaining a commitment”, which are phrases that come from pharmaceutical marketing. We’re “selling” and promoting public health interactions, so we work on those skills. We also do a great deal of role playing, including videotaped analysis of each rep. We look at body language, what communication skills are effective, we do knowledge assessments, quizzes—we make sure our team is well-prepared to go out and detail. We take this seriously—they’re representing the New York Department of Health and Mental Hygiene.
 What’s a major barrier your program has faced, and how have you tackled it? Michelle: A big challenge, when starting a detailing program, is access. The landscape of healthcare systems in NYC has drastically changed over the past few years. As an example, several years ago, the majority of our Brooklyn territory was almost entirely made of up of small practices where access wasn’t an issue. What’s changed since then? Michelle: Now, many of these sites have become part of larger institutions, so there’s corporate buy-in that needs to happen for people to come in and talk to the staff. As I mentioned before, although we try and limit group presentations, this has proven to be an effective strategy when entering into a new relationship. Once they get to know us and recognize the value of the program, they’re engaged in having us come back to conduct 1:1 visits on the follow-up and subsequent campaigns. How do you know when a campaign is working and becoming successful? Michelle: Evaluation is always on the top of our priorities, and can be a challenge for any program to evaluate effectiveness. For every campaign we conduct an initial and follow-up visit where we assess provider practice. This allows us to see if there has been a change in practice from the initial to the follow-up visit. Additionally, we rate what providers intend to adopt in terms of the key recommendations and supporting tools and resources. We also collect a large amount of qualitative data because it's also critical to gaining a more complete picture of the campaign’s success, especially when reporting on barriers, access and materials.
You can scale this up or down, depending on your need and organizational priorities. Our program focuses on where there’s the greatest need and potential for greatest impact. Programs should make sure to look at their organization’s agenda and goals. It’s important to look at the data and plan the best course of action within the capacity you have. Biography: Michelle Dresser. Michelle Dresser is the Senior Manager of Programming and Strategy for the Public Health Detailing Program within the Bureau of Chronic Disease Prevention and Tobacco Control at the New York City Department of Health and Mental Hygiene. In this role, she oversees the overall programmatic direction and strategy of the program. This includes, campaign strategy and timing, campaign content, training and economic incentive development, provider selection, identification of targets to ensure the greatest impact on populations most in need, and identification of “new needs” opportunities to expand program reach and achievement of program goals. She also oversees internal and external strategic relationships to enhance programmatic objectives.
An Interview with Mass Mental Health CenterFeaturing Mark Viron, MD, adult psychiatrist & Director of Health Home Services at the Department of Mental Health’s Massachusetts Mental Health Center (MMHC) in Boston; Assistant Professor at Harvard Medical School. Tags: Materials Development, Mental Health, Smoking Cessation, Training NaRCAD: We’re excited to talk about your program because it focuses on such an important population, and such a specific topic that’s been a focus of public health initiatives across the nation. Tell us about Massachusetts Mental Health Center (MMHC).  Mark Viron: MMHC is a Department of Mental Health (DMH) community mental health center in Boston that has provided mental health services for over 100 years to people with chronic and persistent mental illness. Its ultimate goal is to help people maintain meaningful and productive lives in their community. In 2013, to better address the significant unmet primary care needs of our patients, we launched the Wellness and Recovery Medicine (WaRM) Center. The WaRM Center offers co-located and integrated wellness and primary care services for all MMHC patients.
NaRCAD: Why, historically, have rates of tobacco use been higher in folks with serious mental illness (SMI)? Why has there been resistance for clinicians to promote tobacco cessation for this group? Mark: It’s a complicated issue. There are risk factors that increase the rate of smoking in this group and these are coupled with obstacles to getting appropriate treatment. People with SMI are overrepresented among populations that face social and environmental conditions that are typically associated with an increased prevalence of smoking – poverty, unemployment, limited education, etc. Obstacles to quitting include limited availability of resources, lack of clinician involvement, and poor social/peer support.
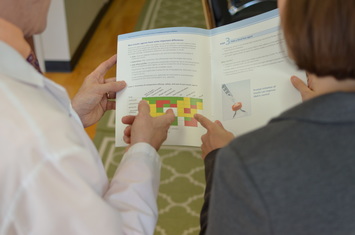
 The strategy of AD: 1:1 clinician-facing outreach. The strategy of AD: 1:1 clinician-facing outreach. NaRCAD: Agreed! What do these AD-focused, 1:1 visits between trained physician educators and psychiatric prescribers entail? Mark: The visits are 20-30 minutes long and follow the typical detailing visit structure. Visits are conducted by me, a psychiatrist at MMHC, or Gail Levine, MD, an internist and the Medical Director of our primary care clinic. We meet with the prescribers in their offices, and begin by asking open-ended questions to assess their needs and learn about their successes (and challenges) in addressing tobacco use with their patients. We celebrate successes and validate challenges, and then pivot to sharing evidence-based information and key messages that may help them address these issues with greater success. We conclude the visit by reviewing steps the prescriber can take to increase successful tobacco treatment, and provide a copy of our detail aid, along with a few high-yield references.  Click to see complete detail aid. Click to see complete detail aid. A key ingredient to our success has been our detail aid. A great psychiatry resident (now attending), Kathryn Zioto, worked with Gail and me and the NaRCAD team to develop a detail aid about tobacco treatment in people with serious mental illness. The detail aid contains cutting-edge, evidence-based information in clear language with colorful graphics. It includes information about the MMHC’S Smoke Free Team, and highlights our three “asks”, which helps clinicians frame their conversations with patients:
NaRCAD: We enjoyed working on this important project with you, and we know how important great materials are in engaging clinicians to consider behavior change. That said, how have psychiatric prescribers been responding? Mark: The response has been quite favorable. It's been rewarding to sit down with colleagues and learn from their experience and expertise and to be able to offer some useful information about tobacco treatment and the Smoke Free Program. The one-on-one detailing encounters, even as brief as they are, give us quality time with our colleagues to focus on their individual concerns and questions. We probably get as much information as we give!
 NaRCAD AD Trainings: hands-on and interactive. NaRCAD AD Trainings: hands-on and interactive. NaRCAD: Two members of your team, yourself and Gail Levine, attended our AD Techniques Training in 2015 to prepare for this initiative. How has the training helped you provide this education to prescribers? Mark: Your training gave us an in-depth immersion into the world of academic detailing, helping us understand theories and evidence and think about implementation issues. Getting to practice detailing and getting feedback from experts in the field was invaluable, as was the ability to talk with people from around the country who are working on similar projects. NaRCAD's training is incredibly worthwhile – it was compact, comprehensive, and helped us acquire the needed skills to implement this project successfully.
 Provider education, engagement and activation are key, and AD provides a framework that has a proven track record in producing results in these areas. Plus, AD is efficient and easily implemented relative to other interventions--especially when you have assistance from NaRCAD! NaRCAD: Thanks for taking the time to connect with us. We’ve enjoyed helping to support this initiative with training and materials development! We look forward to continuing to learn about the impact you have on improving the health of people with serious mental illness, and sharing it with the community. We can't wait to hear more about this intervention at our conference this fall!  Biography. Mark Viron, MD is an adult psychiatrist and Director of Health Home Services at the Department of Mental Health’s Massachusetts Mental Health Center (MMHC) in Boston and an Assistant Professor at Harvard Medical School. He specializes in the treatment of psychotic disorders and the integration of primary and behavioral healthcare for people with serious mental illness. He graduated from Tulane University School of Medicine and completed his psychiatry residency at the Massachusetts General Hospital/McLean Residency Program. He serves as an attending at MMHC’s partial hospital program, where he teaches and trains residents and medical students. He is also the project director for two grant-funded initiatives that aim to enhance MMHC’s ability to provide integrated primary and behavioral healthcare. Director's Letter, Summer 2016 Mike Fischer, MD, MS, NaRCAD Director Tags: Conference, Director's Letter, Training Summer is in full swing, but we’re already looking ahead to #NaRCAD2016, our 4th International Conference on Academic Detailing, which we’ll host this fall on November 14th & 15th in Boston. We received a wonderful response to our first-ever call for proposals, with submissions from across the country and around the world, making the 2016 conference our most exciting and community-informed meeting yet. Our team was inspired by the innovative and diverse proposals we received. Following in the footsteps of previous conference series programming, this year’s applications demonstrated a dedication to improving the quality of care and patient outcomes. #NaRCAD2016 applicants showcased success across a broad spectrum of AD interventions: in outpatient and inpatient settings, in public and private systems, and for a wide range of clinical topics. We’re thankful to all who applied for #NaRCAD2016, and we encourage those who are just beginning to roll out an intervention to consider applying for next year’s conference. Along with presentations from our selected applicants, this year’s program will include carefully designed content from leaders in the field, interactive learning sessions, and networking opportunities, including an evening reception. This year will be your chance to learn about cutting edge interventions being implemented across the globe, to share your unique perspective and experiences, and to collaborate with a thriving community of clinical outreach education colleagues. In that spirit of collaboration, we’re always eager to hear from you, the members of our learning network. We can support your AD programming with expert techniques training, materials development, evaluation, or by highlighting your work. We’re also dedicated to personally connecting our network members to one another, working to amplify our community’s knowledge, tools, and impact. Take a minute to tell us what resources you need, to explore our Learning Center, or to join the conversation—either virtually, or in Boston in November.
We’ll see you at #NaRCAD2016—registration is now open, and space is limited! If you have questions, let our team know. -Mike Expert Trainer Insight Series, Part 2:An Interview with Amanda Kennedy, PharmD, BCPS, Director of the Vermont Academic Detailing Program Tags: Detailing Visits, Expert Training Insight Series, Rural AD Programs, Training  Dr. Amanda Kennedy & NaRCAD's Dr. Jerry Avorn Dr. Amanda Kennedy & NaRCAD's Dr. Jerry Avorn NaRCAD: Hi, Amanda! We’re looking forward to chatting with you. You’ve been an academic detailer for about 13 or 14 years—tell us about the Vermont program. Amanda: The Vermont Academic Detailing Program was started in 1999, by Amy Jaeger, PharmD. I trained with Dr. Jaeger as a pharmacy resident. When she left Vermont in the early 2000s, she wanted to leave the program to someone who would be passionate about evidence-based prescribing in primary care. So the job was mine! Amy unfortunately passed away unexpectedly in 2005, but her mentoring and passion for patient care has stayed with me, and has forever shaped the way I think about pharmacy and academic detailing. We’ve evolved over time into a more organized program, with a grassroots focus of serving our state’s primary care providers. This commitment to service is how we succeed in building strong relationships with providers over time, and we infuse the spirit of service into all of our sessions. 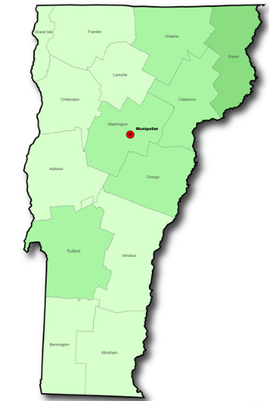 NaRCAD: What challenges do you face that are specific to being a rural program? Amanda: Our program has been stable, but it's been low budget over time. Despite being a small state, we face many challenges balancing the feasibility of delivering sessions to providers with our rural geography. The evidence-base for academic detailing clearly demonstrates the value of a 1:1 ratio of academic detailer to provider. However, it doesn’t make sense for us to travel 2 hours each way to see one provider only to repeat the process the next day for a second provider within the same practice. So we mostly deliver small group academic detailing sessions, as a way to serve as many providers as possible within our budget. We‘re mindful that “small group” means about 3 prescribers, which matches the types of practices we serve. NaRCAD: Along with being a seasoned academic detailer, you also help us here at NaRCAD to train groups of new detailers at our Boston-based techniques trainings. Can you share some highlights? Amanda: The power of the NaRCAD trainings is in the power of the individuals who attend. Realizing that other people are struggling with the same issues, and trying to address these issues with academic detailing, is so powerful.
 Amanda works 1:1 with a trainee at a 2016 NaRCAD course. Amanda works 1:1 with a trainee at a 2016 NaRCAD course. NaRCAD: What would you tell someone who’s thinking about coming to a future NaRCAD training? Amanda: I'd tell them to have fun with it! This training is a special opportunity to focus on how to best communicate with people around behavior change. It allows one to put aside specific topics and come together in a group to think about how best to deliver complex information. The model applies across topics, allowing people from all types of programs to work towards a common goal. The training is hard work, but so rewarding, and offers the chance to learn and network with other trainees. The best part is that it’s immediately applicable upon returning to your program. NaRCAD: That’s good advice—we agree that learning opportunities should be both challenging and enjoyable. In other news, we heard you recently presented at a U.S. House of Representatives Congressional Briefing. Tell us about that. Amanda: I was invited to present at the briefing entitled, “Getting the Medications Right”: An essential ingredient in achieving the goals of H.R. 4878 – the Medicare Better Care, Lower Cost Act. The briefing was presented by the American College of Clinical Pharmacy and the College of Psychiatric and Neurologic Pharmacists. The purpose of the briefing was to highlight pharmacists as members of the primary care team. I specifically presented some of my Vermont research that involved partnering pharmacists within patient-centered medical homes. It was the perfect opportunity to showcase the innovative work we are doing here in Vermont. I think there was a great response from those who attended and for me personally, it was an absolute honor to be there.
NaRCAD: Thanks so much for taking the time to connect with us, Amanda. We’re delighted to have you as part of our core team of training facilitators, and we’re excited to share what you’re doing in Vermont with our community. Learn more about Amanda Kennedy, or visit our Team Page to learn more about NaRCAD staff. Join Us: NaRCAD's next training is open for registration.
Ask the Expert: Questions for Amanda? Ideas for us? Thoughts on detailing? Share your response in the comment section below for community discussion!  Director Dr. Mike Fischer chats with trainees about their goals. Director Dr. Mike Fischer chats with trainees about their goals. Bevin K. Shagoury, Communications & Education Director @ NaRCAD Tags: Detailing Visits, Training We’ve just wrapped up our Spring Academic Detailing Training here in Boston, and we're excited to share a recap of an important event. With each new class of trainees, we see new ways that academic detailing can improve health outcomes for a variety of topics and populations. This May 16th & 17th, the NaRCAD team hosted 18 trainees from across the U.S. and Europe. Our trainees represented programs looking to increase STD screening and sex education in Philadelphia, reduce overmedication of elderly long-term care residents across Indiana, teach safer opiate prescribing in Wisconsin, and implement other quality improvement initiatives in Ireland, Denmark, Georgia, Rhode Island, and North Dakota.
 Join us at our next training event. Join us at our next training event. Everyone at NaRCAD would like to thank our fantastic, enthusiastic class of trainees for participating. We’ll be keeping in close touch as they go out into the field to implement important academic detailing interventions. For other members of our community, we hope you’ll consider joining us this Fall at our next 2-day course on September 19th & 20th, 2016--it's the core of what we do. If it helps to convince you, 100% of our trainees from this week's course said they'd recommend our course to a colleague, so save the date, and be sure to register early as space is limited and seats fill quickly. Registration opens on June 15th-we're looking forward to seeing you there! Until then, remember: "Good information doesn't disseminate itself."  Tags: Autism, CME, Conference, Detailing Visits, Pediatrics, Practice Facilitation, Training NaRCAD: Hi, Meagan and Mindy—thanks for taking the time to talk with us about your clinical outreach education programming at Colorado ABCD. Can you give us an overview about ABCD and its mission to improve child development? Meagan Shallcross: Colorado Assuring Better Child Health & Development (ABCD) works with community partners, pediatric healthcare providers, early learning providers, and families across Colorado communities. The goal is to strengthen systems and identify children with developmental delays, connecting them with community services as early as possible.
 Meagan Shallcross, MPH Meagan Shallcross, MPH NaRCAD: Tell us a bit about your backgrounds. How did you each get into healthcare improvement? Meagan: My background in public health, along with experience working in clinical settings and behavioral science research, developed my interest in healthcare improvement that aims to bridge community work and clinical practice, standardize clinical workflows, and ultimately improve experiences and outcomes for patients and families  Mindy Craig, PA-C, M.S. Mindy Craig, PA-C, M.S. Mindy Craig: My path to healthcare improvement is a little different than what you might expect. I worked for Northwest Airlines as a flight attendant for several years straight out of college. At that time the airline industry was losing a large amount of money and needed to find a new way of operating. They decided to utilize a Total Quality Management approach and enlisted people from every department to undergo training in TQM and then facilitate small departmental groups in quality efforts. It was through this process that I began to understand the importance of doing business with a quality framework.  Learn more at coloradoabcd.org. Learn more at coloradoabcd.org. Eventually, I left Northwest and started working in a Neurology clinic while going back to school with the goal of becoming a PA. After completing my degree I worked in primary care settings for about 10 years. I participated in small clinic QI efforts over the years and continued to be interested in quality improvement. I was hired by ABCD 8 years ago to bring a clinical perspective to their physician outreach. It was a natural progression for me to start approaching our work at ABCD with a quality improvement framework. The power of engaging front line staff to implement changes that result in improvement remains as strong as it was when I worked in the airline industry. NaRCAD: Talk with us about your academic detailing programming at ABCD—you’ve been doing this for about 10 years, right? Mindy: We started our work encouraging the use of standardized developmental screening tools in the primary care settings. This was supported by the American Academy of Pediatrics policy statement in 2006 recommending the use of these tools at well child visits. We offered informal outreach to physicians providing instructions on screening tools, billing information, AAP recommendations and information on referral resources. We quickly recognized that screening alone wasn’t sufficient and began talking about the referral process and how to ensure successful referrals were being made. At around this time, research was showing us that only about 50% of children referred for Early Intervention services were actually connecting to that referral. It was easy to identify children with concerns but not as easy to ensure they received needed support. We decided to try formalizing our approach to outreach by offering Continuing Medical Education [CME] credits. While we didn’t change content, offering CME changed the way providers saw us as detailers. We appreciated the new credibility, but still struggled with recruiting new practices. NaRCAD: Recruiting practices to participate is a challenge for many programs. How did this struggle transform into quality improvement?
We now offer Quality Improvement [QI] and MOC projects for implementing developmental screening, autism screening and postpartum depression screening in addition to a project that aims to increase the percentage of children who successfully connect with Early Intervention when referred from their primary care provider. We have been thrilled with the response from physicians for participating in these projects and just received funding to continue and grow our outreach efforts. NaRCAD: What have been some other challenges you’ve faced when going in to talk to clinicians about implementing developmental screening? Mindy: I started working at ABCD unsure of how to provide physician outreach, so I naturally modeled my efforts on the one successful approach I knew very well, which was pharmaceutical sales. As the recipient of pharmaceutical detailing, it was pretty easy to begin my outreach efforts in a similar fashion. I quickly learned how it feels to be a detailer. Front office staff rejected me repeatedly, I made hundreds of phone calls that didn’t get returned, and when I did get to speak to a provider I had to speak quickly and to the point to keep their attention. The challenge of gaining access was the biggest barrier I confronted early on and remains at the top of the list.
 A key challenge: gaining access to clinicians. A key challenge: gaining access to clinicians. NaRCAD: When dealing with those challenges, what’s helped you to build relationships with clinicians in order to gain commitment? Meagan: To deal with the challenges that arise, we have found that it helps to get creative in our approach to gain access to clinicians and add credibility to our messages. A barrier we have encountered when trying to schedule times to meet with clinicians is the expectation that we will provide food. Our funders and budgets do not allow us to pay for food, so we have opted to provide other incentives for clinicians, such as CME or MOC credit. Not only is offering CME/MOC credits an educational incentive for providers, but it lends credibility to our messages. We facilitate our QI projects through multiple meetings at the practice and have found that, by developing relationships and a presence in the office, we can overcome clinicians’ resistance to implementing screening or other changes in their practice.
 Resource and best practices exchange at #NaRCAD2015 Resource and best practices exchange at #NaRCAD2015 NaRCAD: We were happy to see you at our 3rd International Conference on Academic Detailing here in Boston a few months ago. Tell us more about how the conference helped you think about your work in a different way. Mindy: We were thrilled to be able to attend the conference and came away very energized. We highly recommend the conference to anyone doing similar work. Some of our key “take-aways” were around the fundamentals of academic detailing, including the need for profession materials and repeated visits to develop relationships. We came home committed to find money for developing professional materials and to attend the two-day intensive training offered by NaRCAD.
However, I’ve struggled with our role as a non-profit in meeting these needs. Up to this point, ABCD has utilized a very hands-on approach. We plan meetings, take notes, write up PDSA cycles, make “To Do” lists – anything we can do to make the process easy for the practice and allow the providers to concentrate on patient care. A true practice facilitation model is more concerned with increasing the capacity of the practice to continue quality improvement work after the facilitation had ended. The goal isn’t to do all the work, but to help the practice find capacity to do it themselves. NaRCAD: What other advice would give to a new and emerging AD program that’s just getting started, or that you’d give yourself if you could go back in time 10 years? Meagan: We have found NaRCAD’s training and tips to be very helpful, so we would recommend that new clinical educators attend a NaRCAD techniques training to hone their skills in communicating their messages with clinicians and gaining commitment to behavior change. One of our main takeaways from the NaRCAD conference was the importance of high-quality, professional materials, so we would recommend that new programs budget for the development of professional materials as well as food, which can be an incentive when setting up meetings with clinicians. Over the years, we’ve realized how critical it is to work with community partners before going into healthcare practices to ensure that clinical workflows, such as processes for making referrals to external agencies, are aligned with community-defined processes and so that clinicians are aware of the resources available to patients and families in their communities. NaRCAD: Thanks so much for sharing important insights from your program to improve childhood health outcomes. We look forward to seeing you at a future training and hearing more about your program's future successes! BiographiesMindy Craig, PA-C, M.S., Director of Physician Outreach, has been with the ABCD team for 8 years and brings with her experience in the clinical setting. She earned her physician assistant degree at the University of Colorado Health Science Center’s Child Health Associate/Physician Assistant program in May 2000. Concurrently, she completed additional course work and research to earn her Master of Science degree in Pediatrics. Ms. Craig worked as a physician assistant in a number of settings for ten years prior to joining the ABCD team. Her medical career has included a variety of medical office positions from medical records clerk to practice manager. This range of experience positions her to fully understand the unique dynamics and flow in a typical office, which allows her to deliver technical assistance to practices at a meaningful level.
Ms. Craig’s quality improvement experience began in the business sector where she was extensively trained on Total Quality Management (TQM) at Northwest Airlines. She worked at the airline as a facilitator, training inflight and ground personnel in the principles of quality improvement. This experience with quality continued in the clinical setting, as she has participated in and/or chaired a number of quality improvement projects over her career as a physician assistant. In addition to her work at ABCD, Ms. Craig also does consulting work for organizations needing assistance with physician outreach and education. Meagan Shallcross, MPH, Healthy Steps/Physician Outreach Coordinator, joined the ABCD team in June 2015 as the Healthy Steps and Physician Outreach Coordinator. Meagan is passionate about building systems and environments that support children’s healthy development through clinical-community partnerships and integrated care delivery approaches. Meagan earned a Master of Public Health degree at the University of Michigan, where she supported Patient and Family Centered Care projects at the university health system and was involved with community-based participatory research addressing health equity, as well as research focused on provider-patient communication. Learn more at www.coloradoabcd.org. All photos used with permission. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|