Exercising Empathy, Planting Seeds: An Interview with the Manchester, NH Academic Detailing Team10/26/2018 Featuring: Carol Furlong, LCMHC, MAC, MBA, Director of Substance Use Disorders, Elliot Hospital Jill MacGregor, APRN, Catholic Medical Center, & Katie Sawyer, LICSW, MLADC, Director, Integrated Treatment of Co-Occurring Disorders, Network4Health/Mental Health Center of Greater Manchester Interview by Isabel Evans, Fellow, NACCHO, in partnership with NaRCAD  Tags: LOOPR, Opioid Safety, Stigma, Substance Use, Training EDITOR'S NOTE: Manchester, New Hampshire, was the third site of four selected for a 2018 pilot program of the CDC (Centers for Disease Control and Prevention), NACCHO (the National Association of County and City Health Officials), and NaRCAD (The National Resource Center for Academic Detailing). This exciting pilot program focused on community-level work with local public health departments to develop customized interventions to reduce opioid overdose and death. Four sites experiencing significant public health problems related to opioids were selected to be trained in academic detailing; those trained health professionals then conducted 1:1 field visits with front line clinicians to impact behavior around prescribing, treatment referrals, and patient care, with Manchester’s team focusing primarily on access to Medication Assisted Treatment [MAT]. As year 1 comes to a close, we’re showcasing successes from the field. Thanks for talking with us about your work in Manchester, New Hampshire. Can you tell us about your team? How were detailers chosen to represent the health department for this pilot project? Carol: Tim Soucy, from the Manchester Department of Health, contacted representatives at each of our organizations and gave a little bit of information about the training. He asked if our organizations had particular people that might be interested, and my supervisor thought of me, since I was in the middle of developing a MAT program for my organization. I jumped at the chance to participate. Jill: My organization received the same email, and as the primary care lead nurse practitioner, I was considered the most appropriate to participate. Katie: The invitation came from the site that received the CDC grant (City Health Department). The invitation was disseminated among a number of local human service/health agencies who are part of a Network of agencies as a result of our 1115 Waiver partnership.  The NaRCAD team came to your site back in March, 2018, helping you get ready to be ‘in the field’ and talk to clinicians about the opioid crisis. Tell us how that went, and how you applied what you learned in training. Carol: I’m a naturally shy person who dislikes being the center of attention, so I was incredibly nervous about the role plays during training. The turned out to be invaluable, since I use the skills I developed through practicing and receiving feedback during every visit. The role plays prepared me so well for meeting with providers, and I go into the conversations feeling confident and comfortable. When they ask questions, I feel that I know how to answer, or where to turn for more information, such as the wonderful handouts available on the NaRCAD website. Jill: For me, learning how to hold a discussion as a detailer was the most important element of the training. I learned how to frame a conversation using open-ended questions, which allows the discussion to progress. Understanding how to simultaneously get a provider’s perspective, while also giving them the information they need, is a critical detailing skill. Katie: We were able to role play, which has proven very helpful out in the field to stay focused, on topic, and empathetic to the position of each clinician that I speak to. The handouts that NaRCAD provided have easy to read information and great graphics, so they have also proved useful for staying on track with the key messages during detailing visits, along with providing supplemental information. 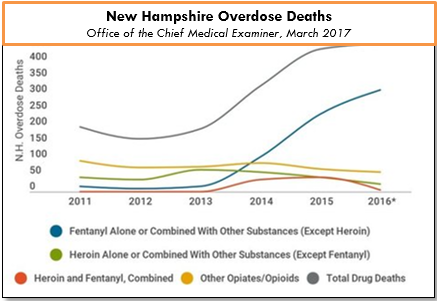 The opioid epidemic has affected many communities in unique ways. How have local clinicians responded to your visits? What do clinicians in Manchester see as major barriers to improving health for their patients struggling with this issue? Carol: Clinicians can be a little skeptical at first, since they’re often expecting that I’m going to try to “sell them” on something. When I focus on listening to their experiences and their concerns, I’m able to gently address those concerns and give resources or suggestions. Even just having a discussion can help clinicians to feel that you’re interested in how they feel, and that you genuinely want to help them – I would describe some clinicians as “dumbstruck” from our conversations, because they’re preparing to do battle with me, but they instead come to see me as a resource, and are more willing to meeting with me. As for challenges, we deal with a fair amount of stigmatization of substance use. It’s a major barrier, and we’ve had to spend a lot of time addressing that in my organization. Another barrier for clinicians is a preconceived notion that providing MAT is an onerous process, and too time-consuming to add into their schedules. And these two barriers really complement each other in a bad way – I often get providers saying that MAT is too much work and that their MAT patients will just end up using opioids again and ending up back in the emergency room. Breaking down these misconceptions about MAT and getting to the root of the stigma against MAT is a big challenge. However, we’re approaching these challenges with education and lots of conversations, since we’ve found that helping our staff to get a better sense of addiction as a disease is really invaluable to making them more open to MAT and treating people with opioid use disorder. The timing of the academic detailing initiative couldn’t have been better for my organization, because having conversations about addiction leads well into having conversations about MAT, and vice versa. Engaging in academic detailing has opened up a whole new avenue of clinician education for me. Jill: Because of my role at my health system, I talk to providers about many different topics and they’re used to me approaching them, which has definitely helped give me and automatic “in” and bring up sensitive topics. My institutional knowledge helps too, since I can answer questions specific to my organization and our various programs or resources around opioids.  A major challenge I face is that providers don’t think they have the time and resources to implement MAT into primary care, and they don’t feel they have the behavioral health support to do so successfully. However, I’ve found that this is often based around a lack of knowledge, since when I ask more probing questions about MAT, it’s often clear that they don’t really know much about it! Providers will come to conclusions without getting the right education, and I find that they often “change their tune” when I give them more information. Providers are also hesitant about writing a prescription for a MAT patient if there isn’t someone in their office who can talk to the patient about addiction itself. Right now, we’re working on integrating behavioral health clinicians into primary care, which I’m hopeful will help with this very real concern. Katie: There has been some hesitation in sharing with detailers, in regards to professional experience, as I believe most clinicians are on edge in trying to do the best that they can to address patient needs, while also supporting alternatives to typical or historical use of prescribed opioids. With an empathetic and interested stance, I’ve found that most clinicians are open with their experience and struggles. There are a number of themes among clinicians for challenges that I’ve noticed, including a limited behavioral health workforce to support what they view as an ideal MAT protocol, which would include individual and group counseling, regular urine toxicology screens, and wraparound services along the continuum of care. In addition, there is a concern among providers about the potential diversion of Buprenorphine by patients.
Katie: It has been rewarding to meet with each clinician for different reasons – I would view success as learning more about the clinicians that are already on board and excited to pursue getting a waiver, as it gets them talking and feeling a renewed energy to share with others. I view my conversations with clinicians who are not interested in pursuing a waiver as equally rewarding, since it allows for both of us to share and hear the other’s perspective. We can agree that the work is needed and challenging, no matter how we decide to go about addressing the needs of our patients. Lastly, what advice would you tell new detailers? What do you wish you knew when you started out? Carol: I would tell new detailers to take a deep breath and know that you’re ready for this – NaRCAD does such a good job of training us as detailers, and you just feel ready. Jill: I would say to recognize that everyone has a natural process for adapting to new ideas. You’ll get some providers who are ready and energized, some who will want to watch others in action before they jump in, and some who simply may not be interested. It can be frustrating when providers aren’t interested in your topic or resources, but understand that this is natural, and don’t take it personally! Every visit will be different, and that’s okay. Katie: My advice is to remember that success is not defined as “convincing” someone that the topic of your detailing visit is “the right answer”. In fact, trying to convince another person of anything is essentially walking against waves. Instead, be open to listening to that person and their experiences, and then value the experience that they have had. This is more likely to open the conversation to allow you to share your wealth of information and experiences. It’s all about planting seeds. Ideas? Comments? Questions? Sound off on this blog in the comments section below!
0 Comments
Leave a Reply. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|
