Optimism for the Opioid Crisis: Addressing Stigma and Disseminating Evidence to Clinicians4/30/2019 An Interview with Don Teater, MD, MPH, Founder, Teater Health Solutions by Kayland Arrington, MPH, Program Manager at NaRCAD Tags: Opioid Safety, Stigma  Don Teater role playing at an academic detailing training in Ware County, GA Don Teater role playing at an academic detailing training in Ware County, GA NaRCAD: Can you tell us about your background? How did you become an addiction treatment specialist? Don: I was trained as a primary care physician, and my wife, Martha, is a behavioral health specialist. The two of us had an integrated-care model, where we did a lot of addiction treatment. I wanted to address that more specifically. An important part of my practice has always been to help those who couldn’t otherwise get help. I did medical work in Honduras, and then I realized that we had a large population of migrant farm workers where I lived in North Carolina. Most of these farm workers didn’t speak English or have a way to receive healthcare. With the help of others, I then opened a free clinic. As far as addiction, I realized that so many patients initially became addicted from my colleagues and me prescribing opioids. The opioid crisis is a public health issue, and medical school doesn’t train you for public health work. Medical thinking addresses what is going on right now, but public health is so much bigger than that. I decided to get a master of public health degree at the University of North Carolina, and I completed that in 2017.  NaRCAD: How does Academic Detailing lend itself to the opioid crisis? Don: Academic detailing can help by having more people with lived-experience do the detailing. In Wisconsin, people with lived experience are either going out with a detailer as a team or doing the detailing themselves. There is also a shortage of people treating OUD. AD is a great program for sharing how to get waiver trained to prescribe buprenorphine for OUD. AD lends itself well to the opioid crisis because it’s an area where little changes can make a big impact. 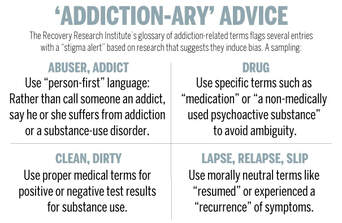 Source: Harvard Gazette Source: Harvard Gazette NaRCAD: There is a huge problem with stigma when it comes to opioid use disorder (OUD), as with any substance use disorder. How can we combat stigma? Don: I hear a lot from other clinicians that they don’t want “those people in my waiting room.” They are picturing someone who is all strung out on heroin on the street corner. We don’t get any education on addiction in medical school and the whole concept is overwhelming to clinicians. The best way to overcome stigma is for clinicians to have interactions with more people with OUD. I think that can be done by clinicians prescribing buprenorphine. I had to deal with my own stigma. For example, I had patients on opioids for chronic pain. I then found out they got arrested or were getting drugs from somewhere else, and I would just fire them from my practice. I saw them as bad people. Once I got trained to prescribe buprenorphine, I listened to their stories. I had made the same choices as many of my patients, yet they became addicted because of their personal history, social history, and genetics. There’s also the importance of language. A lot of the older language around OUD identifies with bad choices and bad people. For example, relapse is associated with a fault of the person. When we are talking about a person with OUD, we are talking about someone with a disease and relapse is a natural course of the disease. When a patient’s blood sugar goes up, we don’t call it a relapse. Just like people with diabetes, we will never cure a person with OUD, but we help them manage.  NaRCAD: We have heard from detailers that many clinicians ask "isn't medication-assisted treatment (MAT) just trading one drug for another?" What do you say to that? Don: There is so much data that shows the first and best treatment for OUD is MAT. There are 11 criteria for OUD, and they are all behavioral. Once people get on the medication, they meet zero of the criteria for OUD. We don’t have many medications for other diseases that can do that. France had a big problem with heroin, and by making buprenorphine more readily available, overdose rates dropped by 80% in 2 years.  NaRCAD: Based on all your research and knowledge, what can be done to stop the opioid crisis? Don: We need to prescribe fewer opioids. A lot of our medical education is still driven by pharmaceutical companies. AD can help by disseminating the evidence on the appropriate treatment of pain. It was only in 2016 that the CDC first came out with guidelines saying opioids should not be the first line of treatment for people with chronic pain. It typically takes 17 years for research to become routine care, and there has already been a lot of uptake with this. Next, we should have all clinicians prescribing buprenorphine, like what France did. We also need to change our criminal justice system to reduce penalties for being found with a controlled substance, including heroin. I am optimistic about each of these things, and think they are all likely to be done in our lifetime – hopefully in the near future.  Biography Don Teater, MD, MPH Founder Teater Health Solutions Don Teater is a family physician who has lived and worked in western North Carolina since 1988. His work in the southern Appalachian Mountains made him aware of the problems with opioid pain medications years ago. In 2004 he started a clinic to treat those addicted to opioids in his primary care practice. From 2013 to mid-2016, he worked as Medical Advisor at the National Safety Council addressing the national epidemic of opioid abuse, addiction, and overdose. Dr. Teater was lead facilitator for the expert panel discussion during the development of the CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. Dr. Teater has also served on the World Health Organization Committee addressing drugged driving that met in Mallorca Spain in December 2015. Since June 2016, Teater has worked for Teater Health Solutions to concentrate on educating prescribers and others on the science of opioids and how that should influence treatment and policy decisions. Currently he contracts with the Center for Disease Control on the academic detailing of prescribers to educate them on the appropriate use of opioids for the treatment of pain.He continues to work one day per week treating those afflicted by the disease of addiction at Meridian Behavioral Health Services in western North Carolina.
0 Comments
Leave a Reply. |
Highlighting Best PracticesWe highlight what's working in clinical education through interviews, features, event recaps, and guest blogs, offering clinical educators the chance to share successes and lessons learned from around the country & beyond. Search Archives
|
